INTRODUCTION
Procedural sedation is the administration of sedatives or dissociative anesthetics to induce a depressed level of consciousness while maintaining cardiorespiratory function so that a medical procedure can be performed with little or no patient reaction or memory.1 Procedural sedation and analgesia is the addition of agents to reduce or eliminate pain.1 Levels of sedation are defined by the patient’s level of responsiveness and cardiopulmonary function, not by the agents used (Table 37-1).2 By definition, patients receiving procedural sedation do not require routine airway protection with endotracheal intubation or other airway adjuncts, as opposed to general anesthesia, which typically requires airway protection. Procedural sedation is commonly done for scheduled outpatient medical procedures by nonanesthesiologists3,4 and is an accepted technique in emergency medicine.5,6,7,8 Procedural sedation performed in the ED presents different issues to the practitioner than scheduled outpatient sedation (Table 37-2).1,7,8
| Responsiveness | Airway | Breathing | Circulation | |
|---|---|---|---|---|
| Minimal sedation (aka “anxiolysis”) | Normal but slowed response to verbal stimulation | Unaffected | Unaffected | Unaffected |
| Moderate sedation (aka “conscious sedation”) | Purposeful response to verbal or physical stimulation | Usually maintained | Usually adequate | Usually maintained |
| Deep sedation | Purposeful response after repeated or painful physical stimulation | May be impaired | May be suppressed | Usually maintained |
| Outpatient | ED | |
|---|---|---|
| Occurrence | Scheduled | Unpredictable |
| Timing | Not time dependent, can be rescheduled | More time dependent, sometimes emergent |
| Gastric state | Fasting | Variable |
| Preprocedure pain | Minimal to none | Often moderate to severe |
| Patient selection | Preselected for little to no systemic disease to reduce sedation risk | Unselected, may have moderate systemic disease |
SEDATION LEVEL
There are several key principles that must be followed to safely perform procedural sedation and analgesia (Table 37-3).1,2,7,8 Despite careful planning and performance, the depth of sedation needed or achieved cannot always be predicted. It is therefore important to prepare for managing deeper levels of sedation than anticipated. Most of the agents used can produce variable levels of sedation, so pay particular attention to dosing and to the patient’s responses to the medications.
Determine appropriate level of sedation desired Have appropriate monitoring and rescue equipment Administer analgesic before sedative Titrate agents to desired level of sedation Observe and monitor until recovery to baseline mental status |
Minimal sedation is characterized by anxiolysis but with normal, although sometimes slowed, response to verbal stimuli. Minimal sedation is typically used for procedures that require patient cooperation and those in which pain is controlled by local or regional anesthesia. Minimal sedation procedures might include abscess incision and drainage, lumbar puncture, simple fracture reductions, and laceration repair. During minimal sedation, ventilatory function is usually maintained with a low risk of hypoxia or hypoventilation. Agents typically used for minimal sedation in adults include nitrous oxide, midazolam, fentanyl, pentobarbital, and low-dose ketamine.
Moderate sedation is characterized by a depressed level of consciousness and a slower but purposeful motor response to simple verbal or tactile stimuli. Moderate sedation most closely matches the formerly used term “conscious sedation.” Patients at this level generally have their eyes closed and respond slowly to verbal commands. Moderate sedation can be used for procedures in which detailed patient cooperation is not necessary, and muscular relaxation with diminished pain reaction is desired. During moderate sedation, the patient is usually able to maintain a patent airway with adequate respirations.9 Depending on the agent, the incidence of hypoxia and/or hypoventilation during moderate sedation is 10% to 30%.10,11,12 Procedures performed using moderate sedation include reduction of dislocated joints, thoracostomy tube insertion, and synchronized cardioversion. Agents used for moderate sedation in adults include propofol, etomidate, ketamine, methohexital, and the combination of fentanyl and midazolam.
Dissociative sedation is a type of moderate sedation. Dissociation is a state in which the cortical centers are prevented from receiving sensory stimuli, but cardiopulmonary activity and responses are preserved. Ketamine is the agent most commonly used for dissociative sedation.13
Deep sedation is characterized by a profoundly depressed level of consciousness, with a purposeful motor response elicited only after repeated or painful stimuli. Deep sedation may be required with procedures that are painful and require muscular relaxation with minimal patient reaction. The risk of losing airway patency or developing hypoxia or hypoventilation is greater with deep sedation than with moderate or minimal sedation.10,14,15 Examples of ED procedures sometimes requiring deep sedation are reducing fracture dislocations, open fracture reductions, and burn wound care. Deep sedation generally is achieved in the ED with the same agents as moderate sedation, but with larger or more frequent doses.
RISK ASSESSMENT AND PATIENT SAFETY
Complications are primarily determined by the interaction of the depth of sedation and the patient’s current medical condition. A common tool for assessing the patient’s underlying medical condition is the American Society of Anesthesiologists’ physical status classification system.16 The risk of a significant complication from ED procedural sedation and analgesia in American Society of Anesthesiologists class I (healthy normal patient) and II (patient with mild systemic disease) is low, usually less than 5%.1,5,6,7,8 The risk of an adverse procedural sedation and analgesia event is correspondingly higher in patients with an American Society of Anesthesiologists class of III (patient with severe systemic disease) or IV (severe systemic disease that is a constant threat to life).17,18
To prepare for procedural sedation, perform a focused history and physical examination.1,3,4,8 The focused history should determine the fasting state, prior experiences with sedation or anesthesia, current medications, and allergies. The focused physical examination identifies a potentially difficult airway or cardiorespiratory problems. A potentially difficult airway should be anticipated when the following findings or conditions are present: short neck, micrognathia, large tongue, trismus, morbid obesity, a history of difficult intubation, or anatomic anomalies of the airway and neck. The implications of these individual factors vary,19,20,21 partially due to the weak interobserver reproducibility.22 Additionally, studies on the association between these findings and difficult intubation are usually done on patients going to the operating room for general anesthesia, and these findings may not be entirely relevant to the ED patient.23 If time allows and an anesthesiologist is available, consultation may be advisable before undertaking procedural sedation in a patient with a potentially difficult airway. At a minimum, difficult airway equipment should be present and available.
Cardiorespiratory conditions increase the complication rate. Most agents can cause vasodilatation and hypotension, particularly in patients with preexisting hypovolemia. Clinically active obstructive pulmonary disease and active upper respiratory infections may predispose the patient to heightened airway reactivity during the procedure and promote hypoventilation. Drug or alcohol intoxication or reduced level of consciousness increases the risk of hypoxemia and hypoventilation. If possible, delay procedural sedation in intoxicated patients until mental status improves.
Routine laboratory studies are not necessary in otherwise healthy patients. Directed ancillary testing may be useful in patients with conditions such as airway abnormalities, infections, advanced age, hepatic or renal disease, dehydration, fever, or hypovolemia. Such conditions may increase the risk of hypotension, prolonged sedation, or hypoxemia. These should be corrected if possible. If correction before procedural sedation is not possible, either delay the procedure or use the lowest possible level of sedation.
The need for sedation is sometimes more urgent than a full preprocedure evaluation. Emergent indications include cardioversion for life-threatening arrhythmias, neuroimaging for head trauma, reduction of fractures or dislocations with soft tissue or vascular compromise, care of contaminated wounds, or intractable pain. Stable fractures, abscess incision and drainage, care of clean wounds, foreign body removal, and laceration repair require less urgent procedural sedation. Nonurgent indications for sedation include the removal of a soft tissue foreign body, placing splints on fractures that require minimal manipulation, or changing splints on fractures that have already been reduced.
RISKS AND PRECAUTIONS
There is no primary evidence that the risk of aspiration during procedural sedation is increased with recent oral intake.24,25,26 Current guidelines regarding the safe fasting period prior to procedural sedation were developed by expert consensus,27 and the American Society of Anesthesiologists guidelines for fasting prior to general anesthesia are of limited relevance to the risk of aspiration with ED procedural sedation.25 Thus recent food intake is not a contraindication.27 If the risk of aspiration is concerning, waiting 3 hours after the last oral intake before performing procedural sedation is associated with a low risk of aspiration, regardless of the level of sedation.27
The anesthesia model for procedural sedation consists of two physicians, one to perform sedation and monitor the patient and the other to perform the procedure. In theory, if one physician is dedicated to administering procedural sedation, it should be possible to monitor the level of sedation, titrate the medication carefully, and identify adverse events earlier. Despite such potential benefits, clinical experience indicates that one emergency physician—providing sedation and performing the procedure—may achieve the same low risk of adverse events as having two physicians.1,28 Thus, for minimal and moderate levels of sedation, one emergency physician simultaneously administering sedation and performing the procedure with a nurse monitoring the patient appears to be an appropriate practice. If available, a clinical pharmacist can provide useful information and assist during procedural sedation, with the potential to reduce the likelihood for medication errors.29
EQUIPMENT
The sedation area should include all necessary size-appropriate equipment for airway management and resuscitation, including oxygen, a bag-mask ventilation device, suction, oral/nasal airway(s), and intubation equipment.1,3,4,8 A defibrillator should be available. Reversal agents, such as opioid receptor and benzodiazepine receptor antagonists, should also be readily available.
PROCEDURAL SEDATION MONITORING
Two types of monitoring are used for ED procedural sedation: interactive monitoring by dedicated observers and electronic monitoring with equipment connected to the patient. The recommended extent of monitoring is determined by the level of sedation (Table 37-4). No matter which method is used, patients must be checked after each dose of medication to assess the response, determine the need for further doses, and make appropriate interventions if adverse events arise.
| Target Level of Sedation | Level of Consciousness | Heart Rate | Respiratory Rate | Blood Pressure | Oxygen Saturation | Capnography End-Tidal CO2 |
|---|---|---|---|---|---|---|
| Minimal | Observe frequently | Measure every 15 min | Measure every 15 min | Measure every 15 min and after sedative boluses | Monitor continuously | No recommendation |
| Moderate or dissociative | Observe constantly | Monitor continuously | Continuous direct observation | Record every 5 min and after sedative boluses | Monitor continuously | Consider continuous monitoring |
| Deep | Observe constantly | Monitor continuously | Continuous direct observation | Record every 5 min and after sedative boluses | Monitor continuously | Recommend continuous monitoring for prolonged procedures |
Interactive monitoring is the direct observation of the patient to assess the depth of sedation and observe for hypoventilation or apnea, upper airway obstruction, laryngospasm, vomiting, or aspiration. Thus interactive monitoring requires an unobstructed view of the patient’s face, mouth, and chest wall.
For minimal sedation, the risk of adverse events is so low that observation by the physician performing the procedure is usually adequate. For moderate and deep sedation, a dedicated observer—typically a nurse in the one-physician model—should continuously monitor the patient while the physician oversees drug administration and performs the procedure.
Electronic monitoring uses equipment to assess arterial oxygenation, ventilation, blood pressure, and cardiac rate and rhythm. Moderate and deep sedation require constant observation and continuous monitoring. Cardiac monitoring is particularly recommended for patients with preexisting cardiac disease or dysrhythmias or during procedures in which the cardiac rhythm is of interest, such as during cardioversion. Arterial oxygen saturation is monitored with pulse oximetry. For almost all patients undergoing minimal sedation and many undergoing moderate sedation, pulse oximetry is adequate as the sole mechanical monitoring modality. However, pulse oximetry is not a substitute for monitoring ventilation, as hypoventilation or apnea develop before oxygen saturation decreases, especially in patients who receive supplemental oxygen.30,31,32,33
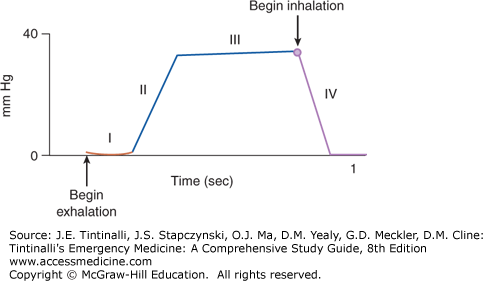
Ventilation can be electronically monitored using capnography, the measurement of the partial pressure of carbon dioxide in exhaled breath.32,33 Many experts suggest that capnography should be used to monitor procedural sedation.34,35,36 The capnography device uses an infrared carbon dioxide detector placed at the nares to sample inhaled and exhaled gases. The partial pressure of carbon dioxide detected at the nares during the respiratory cycle is represented by the carbon dioxide waveform (capnogram) that can be displayed on the monitor (Figure 37-1). A value commonly reported on the capnography device is the end-tidal carbon dioxide: the maximum carbon dioxide concentration at the end of each tidal breath. The end-tidal carbon dioxide correlates with arterial partial pressure of carbon dioxide so that an end-tidal carbon dioxide above 50 mm Hg or an increase in end-tidal carbon dioxide >10 mm Hg indicates hypoventilation. Capnography can assess the severity of ventilatory abnormalities and the response to interventions. Most importantly, capnography can detect changes in ventilation before clinical observation.32,33
FIGURE 37-1.
Normal capnogram. Phase I: At the start of exhalation, carbon dioxide concentration in the exhaled gas is essentially zero, representing gas from the anatomic dead space that does not participate in gas exchange. Phase II: As the anatomic dead space is exhaled, carbon dioxide concentration rises as alveolar gas exits the airway. Phase III: For most of exhalation, carbon dioxide concentration is constant and reflects the concentration of carbon dioxide in alveolar gas. Phase IV: During inhalation, carbon dioxide concentration decreases to zero as atmospheric air enters the airway. [Reproduced with permission from Krauss B, Hess DR: Capnography for procedural sedation and analgesia in the emergency department. Ann Emerg Med 50: 172, 2007 (Table 1, p. 176). Copyright Elsevier.]
Variations in the capnogram can identify specific conditions, such as apnea, upper airway obstruction, laryngospasm, bronchospasm, and respiratory failure.32 A flat-line capnogram can be due to apnea, upper airway obstruction, or complete laryngospasm. Normalization of the waveform after airway alignment maneuvers (chin lift, jaw thrust, or oral airway placement) confirms that apnea was due to upper airway obstruction.
Capnography during procedural sedation allows the early recognition of adverse events.1,32,33 Because the risk of respiratory depression increases with the depth of sedation, capnography should be considered for moderate sedation and is recommended for prolonged deep sedation.
Vital signs (pulse, blood pressure, and respiratory rate) and oxygen saturation should be obtained and recorded before the procedure, after each dose of medication, upon completion of the procedure, at the beginning of the recovery period, and before discharge.1,3,4,8 For mild sedation, intermittent measurements are sufficient. For moderate and deep sedation, it is recommended that blood pressure be assessed every 5 minutes and heart rate and pulse oximetry be continuously monitored. Patients are at the highest risk of hypoxia and hypoventilation during the period immediately after IV medication administration (until the peak effect of the medication has been reached) and during the immediate postprocedure period (when external stimuli are discontinued and the stimulating pain of the procedure has subsided).
Predesigned documentation forms are a good practice because such forms can guide the providers through the procedure, improve the quality of the documentation of the procedure,37 and better tabulate sedation-related events for quality-auditing purposes.38
The level of sedation can be assessed using structured scoring techniques, such as the Ramsay Sedation Scale© and the Observer’s Assessment of Alertness/Sedation Scale©. However, regular patient monitoring is more important than the application of scales. Specific central nervous system monitoring, such as the bispectral index scale that uses processed electroencephalogram signals to measure the depth of sedation, is primarily a research tool for procedural sedation.11,15,39,40
STEP-BY-STEP TECHNIQUE
The administration of morphine or fentanyl for pain control before the start of procedural sedation will provide the patient with analgesia during the procedure. Pain should be controlled so the patient is comfortable, but if preprocedure pain is intractable and if the procedure itself will result in pain relief, do not wait for complete pain control to begin.
Begin procedural sedation after the last dose of analgesic has reached its peak effect (3 to 5 minutes for IV morphine and 2 to 3 minutes for IV fentanyl). The administration of propofol or etomidate concurrently with analgesics may increase the likelihood of adverse events, so these medications should be titrated separately.18,41
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree