![]() To alleviate compartment syndrome in ischemic low-flow (veno-occlusive) priapism
To alleviate compartment syndrome in ischemic low-flow (veno-occlusive) priapism
![]() May be caused by:
May be caused by:
![]() Trauma (genital, pelvic, perineal)
Trauma (genital, pelvic, perineal)
![]() Thromboembolism (sickle cell disease, leukemia)
Thromboembolism (sickle cell disease, leukemia)
![]() Medications (cyclic guanosine monophosphate [cGMP] inhibitors, neuroleptics, erectile-dysfunction treatment, cocaine/marijuana/ecstasy, and others)
Medications (cyclic guanosine monophosphate [cGMP] inhibitors, neuroleptics, erectile-dysfunction treatment, cocaine/marijuana/ecstasy, and others)
![]() Neoplasm (primary or metastatic)
Neoplasm (primary or metastatic)
![]() Neurologic disorders (spinal cord injury, spinal stenosis)
Neurologic disorders (spinal cord injury, spinal stenosis)
![]() Infection (recent infection with Mycoplasma pneumoniae, malaria)
Infection (recent infection with Mycoplasma pneumoniae, malaria)
CONTRAINDICATIONS
![]() Absolute Contraindications
Absolute Contraindications
![]() Nonischemic high-flow (arterial) priapism
Nonischemic high-flow (arterial) priapism
![]() Use history, physical, and selected laboratory tests to help distinguish low- from high-flow priapism. Note especially that high-flow priapism is usually not painful.
Use history, physical, and selected laboratory tests to help distinguish low- from high-flow priapism. Note especially that high-flow priapism is usually not painful.
![]() See “Technique” section for further methods of differentiation
See “Technique” section for further methods of differentiation
![]() Priapism relieved noninvasively
Priapism relieved noninvasively
![]() Medical treatment of underlying etiology
Medical treatment of underlying etiology
![]() Maneuvers (e.g., ice packs to groin, “steal phenomenon”)
Maneuvers (e.g., ice packs to groin, “steal phenomenon”)
![]() Relative Contraindications
Relative Contraindications
![]() Coagulopathy
Coagulopathy
RISKS/CONSENT ISSUES
![]() Major risk of priapism with or without treatment is long-term impotence. This should be explained clearly to the patient and documented.
Major risk of priapism with or without treatment is long-term impotence. This should be explained clearly to the patient and documented.
![]() Procedure may cause pain (anesthesia will be given)
Procedure may cause pain (anesthesia will be given)
![]() Needle puncture may cause local bleeding and scarring
Needle puncture may cause local bleeding and scarring
![]() Potential for infection (sterile technique will be used)
Potential for infection (sterile technique will be used)
![]() If phenylephrine is injected, untoward cardiac effects may be seen (the patient must be monitored)
If phenylephrine is injected, untoward cardiac effects may be seen (the patient must be monitored)
![]() General Basic Steps
General Basic Steps
If aspiration does not result in detumescence, continue with the subsequent steps. If, after completing the steps below, detumescence is not achieved or maintained, emergent urologic evaluation is required.
![]() Anesthesia (penile nerve block)
Anesthesia (penile nerve block)
![]() Verify priapism is ischemic/low-flow (penile blood gas)
Verify priapism is ischemic/low-flow (penile blood gas)
![]() Aspiration
Aspiration
![]() Irrigation
Irrigation
![]() Injection/aspiration cycles
Injection/aspiration cycles
![]() Dressing
Dressing
LANDMARKS
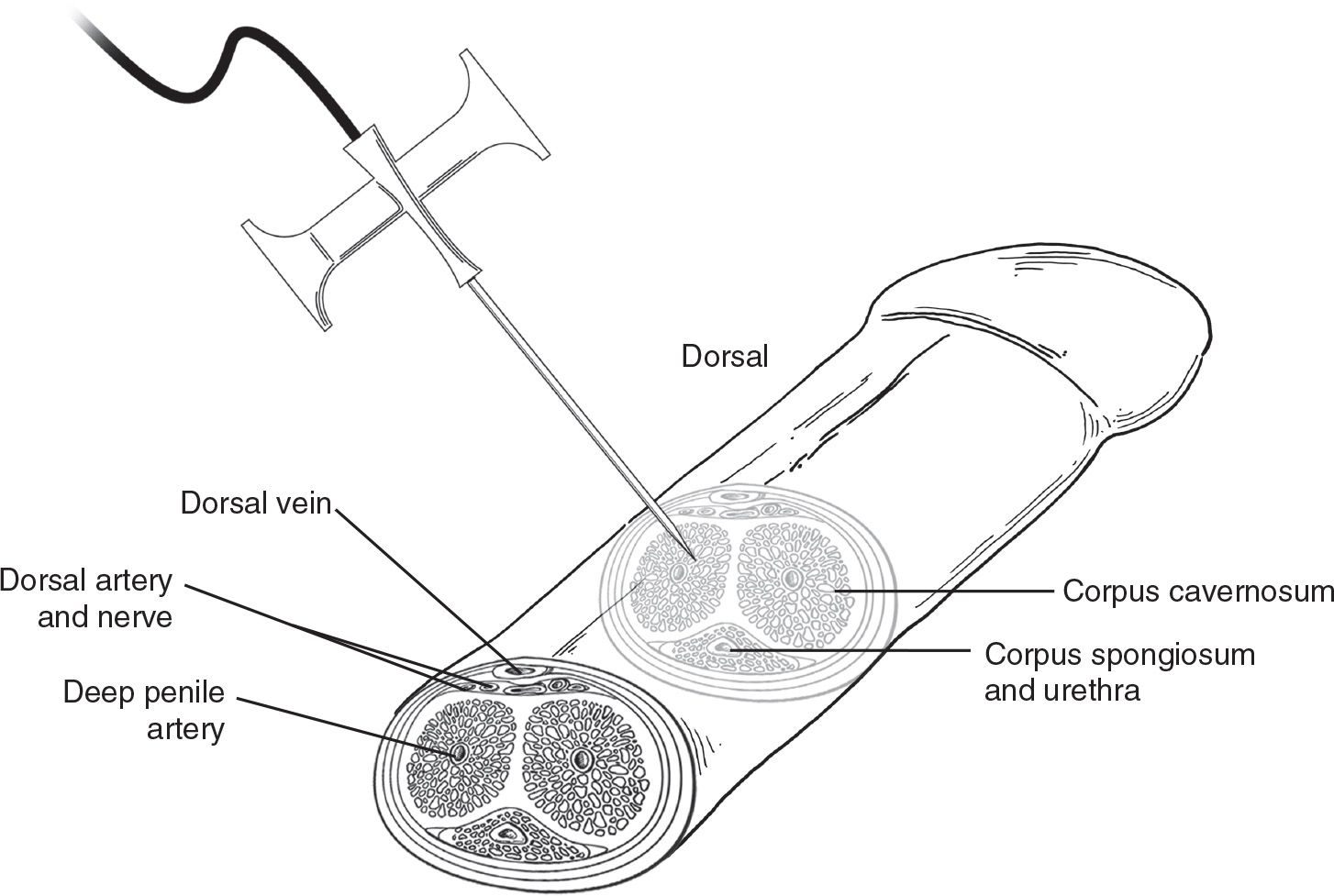
![]() Needle aspiration/irrigation of one of the paired cavernosa is performed dorsolaterally on the shaft of the penis, at either the 3- or 9 o’clock position. This technique avoids the corpus spongiosum and urethra ventrally and the neurovascular bundle and penile vein dorsally.
Needle aspiration/irrigation of one of the paired cavernosa is performed dorsolaterally on the shaft of the penis, at either the 3- or 9 o’clock position. This technique avoids the corpus spongiosum and urethra ventrally and the neurovascular bundle and penile vein dorsally.
SUPPLIES
![]() Povidone–iodine or chlorhexidine
Povidone–iodine or chlorhexidine
![]() 1% Lidocaine without epinephrine
1% Lidocaine without epinephrine
![]() 27-gauge needle (for penile block)
27-gauge needle (for penile block)
![]() Sterile field supplies
Sterile field supplies
![]() Sterile gloves
Sterile gloves
![]() Scalp vein (“butterfly”) needle
Scalp vein (“butterfly”) needle
![]() Prepubescent boys: 21 to 23 gauge
Prepubescent boys: 21 to 23 gauge
![]() Adolescents and adults: 19 gauge
Adolescents and adults: 19 gauge
![]() Three-way stopcock
Three-way stopcock
![]() 10-mL empty syringe
10-mL empty syringe
![]() 10-mL syringe with normal saline
10-mL syringe with normal saline
![]() 10-mL syringe with phenylephrine solution (see text below)
10-mL syringe with phenylephrine solution (see text below)
![]() 4- × 4-cm gauze
4- × 4-cm gauze
![]() Kerlix™ (bandage roll) gauze or Coban™ (self-adhesive bandage roll) gauze
Kerlix™ (bandage roll) gauze or Coban™ (self-adhesive bandage roll) gauze
TECHNIQUE
![]() Anesthesia
Anesthesia
![]() Perform a penile ring block: Clean the base of the penis with povidone–iodine or chlorhexidine (preferred) solution. Use 1% lidocaine and a 27-gauge needle to perform a ring block around the entire base of the penile shaft (see chapter 36 for details).
Perform a penile ring block: Clean the base of the penis with povidone–iodine or chlorhexidine (preferred) solution. Use 1% lidocaine and a 27-gauge needle to perform a ring block around the entire base of the penile shaft (see chapter 36 for details).
![]() Consider systemic analgesia as well
Consider systemic analgesia as well
![]() Verification
Verification
![]() Perform a penile blood gas: Clean the shaft of the penis as above. If the ring block is incomplete, infiltrate 1 mL of 1% lidocaine with a tuberculin syringe for supplemental local anesthesia. Use a scalp vein (“butterfly”) needle attached to the syringe to puncture perpendicularly at the 3- or 9 o’clock position on the penile shaft to draw blood gas (FIGURE 39.1).
Perform a penile blood gas: Clean the shaft of the penis as above. If the ring block is incomplete, infiltrate 1 mL of 1% lidocaine with a tuberculin syringe for supplemental local anesthesia. Use a scalp vein (“butterfly”) needle attached to the syringe to puncture perpendicularly at the 3- or 9 o’clock position on the penile shaft to draw blood gas (FIGURE 39.1).
![]() Note the color of aspirated blood. As a guideline, low-flow priapism is more consistent with the following: pH <7.0 to 7.25, PO2 <30 mm Hg, and PCO2 >60 mm Hg. A high-flow lesion will more closely reflect normal arterial values.
Note the color of aspirated blood. As a guideline, low-flow priapism is more consistent with the following: pH <7.0 to 7.25, PO2 <30 mm Hg, and PCO2 >60 mm Hg. A high-flow lesion will more closely reflect normal arterial values.
![]() A penile Doppler ultrasonography may be considered, if available, to aid in distinguishing high- from low-flow priapism
A penile Doppler ultrasonography may be considered, if available, to aid in distinguishing high- from low-flow priapism
![]() Penile aspiration is indicated only for low-flow priapism (FIGURE 39.2)
Penile aspiration is indicated only for low-flow priapism (FIGURE 39.2)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree