CHAPTER 24 Posterior sciatic block
Clinical anatomy
The sciatic nerve originates from the lumbar and sacral plexes and is the largest nerve in the body. The ventral rami of L4 and L5 join with those of S1, 2, and 3 to form the sciatic nerve. It is made up of two major nerves: the common peroneal and the tibial. The sciatic nerve arises on the pelvic surface of the piriformis muscle. It then passes out of the pelvis into the gluteal region through the greater sciatic foramen below the piriformis muscle, and descends between the greater trochanter of the femur and the ischial tuberosity (Figs 24.1 and 24.2). Once it emerges from under cover of the gluteus maximus, it becomes superficial as it passes down the posterior thigh.
Surface anatomy
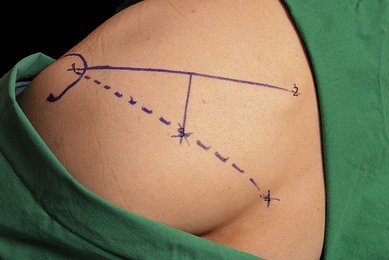
A consistent method of outlining the greater trochanter is needed because this is a large structure and variations can affect further marking. It is suggested that the outer perimeter of the greater trochanter is used for line drawings. A line is drawn between the posterior superior iliac spine and the greater trochanter (Fig. 24.3). This line is bisected and a perpendicular line is drawn passing downward from its midpoint. A further line is drawn from the sacral hiatus to the greater trochanter. The point at which this line intersects with the perpendicular line marks the point for needle insertion. The intersection is usually 5 cm along the perpendicular line.
Sonoanatomy
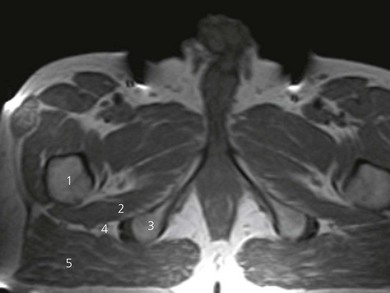
The patient is positioned laterally, with the side to be anesthetized uppermost and with the hip and knee flexed (Fig. 24.4). Perform a systematic anatomical survey from cephalad to caudad and from superficial to deep using a low-frequency, 5–2 MHz, curved array ultrasound transducer. The prominence of the greater trochanter and the ischial tuberosity are identified. These are seen as hyperechoic lines with shadowing beneath. On a sonogram, the ‘subgluteal space’ is seen as a hypoechoic area between the hyperechoic perimysium of the gluteus maximus and the quadratus femoris muscles (Fig. 24.5). It extends from the greater trochanter laterally to the ischial tuberosity medially. At this level, the sciatic nerve is seen as an oval hyperechoic nodule approximately 1.5–2 cm in diameter within the subgluteal space. It is often difficult to see the sciatic nerve due to tissue depth and reflections of muscles and fascial coverings. Follow the nerve by scanning proximally (cephalad) and distally (caudad) to follow the course of the nerve. It may be necessary to first identify the nerve in the posterior thigh region and then trace the nerve proximally, should visualization be difficult.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree