g. The demand-only IV PCA incorporates several safety features to minimize the possibility of a patient receiving unsafe doses of IV opioid. First, the PCA pump is programmed to limit the amount of opioid per patient request and per hour. Second, if the patient is very sedated, she will be unable to push the PCA demand button and the current opioid effect will diminish. Unfortunately, even with these safeguards, adverse outcomes have occurred with IV PCA in post-CD patients. Examples include visitors activating the PCA demand button for the patient (i.e., PCA by proxy) and medication and programming errors.15,16
CLINICAL PEARL IV PCA opioid administration offers superior pain relief compared to intermittent administration by health care workers. Its safety is maximized if given by patient demand only without use of a low-dose baseline infusion.
3. Epidural opioids
a. Specific medications studied include morphine, meperidine, hydromorphone, fentanyl, sufentanil, oxymorphone, methadone, nalbuphine, butorphanol, buprenorphine, and diamorphine (not available in the United States).
b. The rationale for neuraxial (i.e., epidural or spinal) administration of opioids is to improve the analgesic efficacy while minimizing the side effects of the opioids when administered by other routes. These side effects include sedation, respiratory depression, nausea and vomiting, itching, and urinary retention. However, all these side effects can occur with either systemic or neuraxial opioids.
c. A single dose of epidural morphine:
(1) Provides better post-CD analgesia than a saline placebo17 or IM opioids12,18
(2) Has similar analgesic efficacy and patient satisfaction compared to IV PCA morphine12,18
(3) Is associated with more pruritus than IV PCA or IM morphine
(4) May be less effective than if given by continuous infusion19
d. Studies of PCEA in patients receiving post-CD analgesia with fentanyl, sufentanil, or hydromorphone demonstrate:
(1) Better pain relief, less medication administration, and more pruritus compared to IV PCA opioids20,21
(2) No benefit of continuous basal infusion PCEA versus demand-only PCEA22,23
e. A single dose of epidural fentanyl should be diluted to an injection volume of at least 10 mL for the best effect.24 However, injection volume variations with single doses of epidural morphine do not have a significant effect on post-CD analgesic efficacy.25
f. Extended-release epidural morphine
(1) It was approved by the U.S. Food and Drug Administration (FDA) in 2004 for postoperative analgesia, with the trade name of DepoDur.26
(2) Two prospective randomized studies have compared DepoDur® to conventional morphine for post-CD epidural analgesia.27,28 The patients who received DepoDur had improved pain scores at rest and with movement as well as improved functional ability. The differences between DepoDur and conventional morphine were restricted to the 24 to 48 hour postoperative time frame, but the magnitude of those differences was clinically modest.
(3) Although it is approved for clinical use, it is currently not being produced by the pharmaceutical company, Pacira, who currently own the license. They are using the carrier, DepoFoam to manufacture the long acting local anesthetic preparation, Exparel.
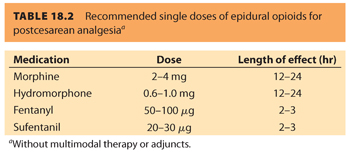
g. Table 18.2 lists the recommended single doses of conventional epidural opioids, based on prospective randomized studies.
h. Adjuncts and epidural opioids
(1) Clonidine (75 to 150 µg) improves post-CD analgesia when added to single epidural doses of fentanyl or morphine.29,30 However, there is an FDA black box warning for clonidine. “Duraclon® (epidural clonidine) is not recommended for obstetric, postpartum, or perioperative pain management . . . ” Use of clonidine alone does not offer significant analgesic improvement over neuraxial opioid use, and the associated side effects of frequent sedation and hypotension mitigate against its routine use.
(2) Epinephrine has demonstrated inconsistent effects in improving analgesia and reducing side effects when added to single doses of epidural opioids.
(3) The use of N-methyl-D-aspartate (NMDA) antagonists (e.g., ketamine, magnesium), although safe and effective in producing analgesia in a very limited number of studies, should be considered experimental at present.
4. Intrathecal Opioids
a. Specific medications studied include morphine, meperidine, fentanyl, sufentanil, nalbuphine, butorphanol, and buprenorphine.
b. In contrast to systemic and epidural routes of administration, IT administration of opioids does not lead to clinically significant maternal serum concentrations of these agents.31,32
c. In most circumstances, IT opioid administration implies a “single-shot” opioid delivery as part of a spinal or combined spinal-epidural (CSE) anesthetic. A number of IT local anesthetics have been combined successfully with IT opioids including lidocaine, bupivacaine, tetracaine, mepivacaine, and ropivacaine.
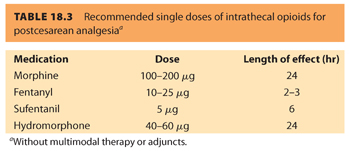
d. Direct comparisons of the IT and epidural routes of administration for single-dose morphine show similar efficacy for post-CD analgesia.31,32 However, the recommended dose is reduced by approximately 20-fold in the IT space.
e. In many instances, pruritus is more prevalent and intense with IT opioids, compared with either epidural or systemic administration.
f. Table 18.3 lists the recommended single doses of IT opioids based on the best available evidence.
g. Adjuncts and IT opioids
(1) Clonidine (60 to 150 µg) improves postcesarean analgesia when added to a single IT dose of morphine or sufentanil.33–35 IT clonidine is likely to increase the duration of the spinal anesthetic as well as maternal intraoperative sedation.34,35 Refer to section III.A.3.h.(1) for the FDA “black box” warning on neuraxial clonidine.
(2) Neostigmine (12.5 μg) improves post-CD analgesia and may reduce side effects when added to a subtherapeutic dose of IT morphine.36 Its short duration of action and side effect profile do not convey significant benefit over use of neuraxial opioids.
(3) Epinephrine does not seem to improve post-CD analgesia when used with IT opioids.
(4) IT ketamine and magnesium use should be considered experimental.
CLINICAL PEARLNeuraxial administered morphine offers superior analgesia of long duration. The use of adjunct medications does not appear to offer significant advantages when added to single-shot neuraxial morphine.
5. Opioid side effects
a. Respiratory depression, with the risk of apnea and hypoxic injury or death, is the most serious side effect of opioids. This complication is encountered in postoperative patients after opioid administration by any route. The American Society of Anesthesiologists developed a practice guideline focused on potential respiratory depression after neuraxial opioid administration.37 Some recommendations included in this document are:
(1) The anesthesiologist should conduct a focused history and physical examination to identify patient characteristics associated with a risk of respiratory depression (obesity, obstructive sleep apnea, coexisting respiratory disease).
(2) Although neuraxial opioids may be safely used in place of parenteral opioids without increasing the risk of respiratory depression, the concomitant administration of parenteral opioids and other sedatives requires increased monitoring due to increased risk.
(3) All patients receiving neuraxial opioids should be monitored for the adequacy of ventilation (respiratory rate, depth of breathing), oxygenation (pulse oximetry depending on patient condition), and level of consciousness, without disturbing a sleeping patient.
(4) After a single injection of lipophilic opioid, monitoring should continue for a minimum of 2 hours, after which the patient’s overall clinical condition should guide monitoring. After a single injection of a hydrophilic opioid, monitoring should be performed for a period of 24 hours, with monitoring at hourly intervals for the first 12 hours and every 2 hours for the next 12 hours.
(5) Supplemental oxygen should be available to all patients and administered to those with signs of respiratory depression or hypoxemia. An IV line should be maintained for administration of reversal agents if needed.
(6) Women after CD may be at lower risk for respiratory depression after neuraxial opioid use compared to other surgical patients. A recent retrospective study of women after CD treated with common doses of epidural or spinal morphine found no instances of respiratory depression in more than 5,000 patients.38
b. Pruritus is a common side effect of neuraxial opioid treatment. In many instances, it seems to worsen with increasing doses of a given opioid and may be more intense with IT as opposed to epidural administration. A number of therapies have been proposed.39
(1) Opioid antagonists. The most consistent treatment is with opioid antagonist medications, either a pure antagonist (e.g., naloxone40) or a mixed agonist–antagonist (e.g., nalbuphine41).
(2) Diphenhydramine. Diphenhydramine 25 mg IV can be helpful in the treatment of pruritus. Although its mechanism of action in this setting is unknown, it can produce profound sedation. Because opioid-induced pruritus does not appear to be mediated by histamine release, the antihistamine-effects of diphenhydramine do not appear to play a significant role in reducing pruritus.
(3) 5-HT3 receptor antagonists. Because morphine is known to activate 5-HT3 receptors by a mechanism independent of opioid receptors, morphine may directly stimulate 5-HT3 receptors and cause IT morphine-induced pruritus. Consequently, occupation of 5-HT3 receptors by a 5-HT3 receptor antagonist potentially prevents the pruritus. Both ondansetron and dolasetron have been administered prophylactically in the treatment of IT morphine-induced pruritus with variable results.
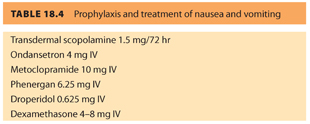
c. Nausea and vomiting has a multifactorial etiology after CD.39 Clearly, opioids can contribute significantly to this problem. As with pruritus, one strategy has been to minimize opioid doses whenever possible through multimodal therapy. There is little consensus about specific therapies to prevent or treat postcesarean nausea and vomiting. Table 18.4 provides suggested prophylactic and therapeutic interventions for nausea and vomiting.
CLINICAL PEARLOpioid agonist/antagonist drugs are effective in treating the pruritus associated with neuraxially administered opioids. Nausea and vomiting are effectively treated with a variety of medications because many factors affect its incidence and severity.
B. Local anesthetics
1. Epidural
a. Local anesthetics, alone or in combination with opioids, may be infused by the lumbar epidural route for post-CD analgesia. The infusion strategy may be continuous or by PCEA, analogous to postoperative analgesia regimens for other lower abdominal surgeries.5
b. Adding a local anesthetic to an epidural opioid infusion may have a dose-sparing effect,42 but it can result in lower extremity motor block and delayed ambulation in women after CD.43
2. Iliohypogastric and ilioinguinal peripheral nerve blocks
a. These two peripheral nerves originate from the L1 spinal nerve root and innervate the abdominal wall region that corresponds to a lower transverse cesarean incision. The blocks need to be performed bilaterally.
b. The existing literature with single-shot nerve blocks presents conflicting results about the effectiveness of perioperative placement of these blocks in decreasing subsequent supplemental opioid use after low transverse CD.44–46
c. A case series of ultrasound-guided continuous ilioinguinal and iliohypogastric nerve blocks in post-CD patients describes apparent opioid-sparing in the postoperative period.47
3. Transversus abdominis plane blocks
a. A transversus abdominis plane (TAP) block is a lower abdominal wall block accomplished by placing local anesthetic medications in the fascial plane between the internal oblique and the transversus abdominis muscles. It must be performed bilaterally and uses approximately 20 mL of local anesthetic per side. Although initially described using surface anatomy landmarks, it is now placed with real-time ultrasound guidance.
b. When used after spinal anesthesia for CD, the TAP block adds value only when IT morphine is omitted from a multimodal analgesic regimen.48,49 A prospective direct comparison study in post-CD patients demonstrates that IT morphine is a more effective analgesic technique compared to a TAP block, but with a higher side effect profile.50 A case series in this patient population describes a continuous bilateral TAP block technique using 20 gauge epidural catheters placed with ultrasound guidance.51
c. The role of TAP blocks in for post-CD analgesia is evolving. Their best use maybe in treating pain after general anesthesia or as rescue treatment after spinal anesthesia52 when neuraxial opioids have failed or are not indicated. Adding 75 µg of clonidine to each side of a post-CD local anesthetic TAP block did not improve its performance in a multimodal analgesic regimen that included IT morphine.53
4. Surgical wound infiltration
a. Single-injection direct surgical wound infiltration with 20 mL of bupivacaine 0.5% at wound closure does not significantly change postoperative supplemental analgesic use after low transverse CD54,55; however, injection of local anesthetic at the fascial level during wound closure decreases opioid requirements during the first 12 hours of recovery.56
b. Postoperative wound infusion, using a catheter inserted at the time of surgery, is an effective post-CD analgesic technique.57,58 Direct comparisons show postoperative wound infusions with local anesthetics are more effective than epidural morphine and similar to systemic diclofenac.58,59 Catheter infusions are most effective when located deep to the fascia at the time of wound closure60 and should be placed using ultrasound guidance to improve success.
c. Postoperative wound infusions with local anesthesia affect specific inflammatory mediators measured in wound exudates, suggesting an interaction with the wound healing process.61
d. It remains to be seen if infiltration of the wound with Exparel®, the long acting local anesthetic product, improves post-CD analgesia, especially on day 2 postoperatively
CLINICAL PEARLTAP blocks do not offer improved analgesia when added to single-shot neuraxially administered morphine. Continuous catheter techniques can improve analgesia but should be placed under ultrasound guidance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







