INTRODUCTION AND EPIDEMIOLOGY
Pneumothorax occurs when free air enters the potential space between the visceral and parietal pleura. Primary pneumothoraces occur without clinically apparent lung disease, either spontaneously or from penetration of the intrapleural space by trauma. Secondary pneumothoraces occur in patients with underlying lung disease.
The incidence of primary spontaneous pneumothorax is 10 to 18 cases for men and 2 to 5 cases for women per 100,000 population.1 Associated factors include cigarette smoking, male gender, mitral valve prolapse, Marfan’s syndrome, and changes in ambient pressure. Familial patterns also suggest an inherited association.2 Physical activity or exertion can precipitate but is not a common pneumothorax-triggering factor. Traumatic pneumothoraces are subdivided into iatrogenic and noniatrogenic. Noniatrogenic pneumothoraces will be further discussed in the chapter 261, “Pulmonary Trauma.”
Causes of secondary spontaneous pneumothorax are listed in Table 68-1. Chronic obstructive pulmonary disease remains the most common cause.3 Pneumothorax occurs in 5% of patients with acquired immunodeficiency syndrome, is associated with subpleural necrosis by Pneumocystis infection, and carries a high mortality. Because of necrosis of lung tissue and continued air leak, simple aspiration fails in this group of patients. Hemopneumothorax occurs in 2% to 7% of patients with secondary pneumothorax and, if associated with a large amount of blood in the pleural cavity, can be life threatening.4,5,6,7 Treating the underlying disease may help decrease the risk of future pneumothorax.
Airway disease
Interstitial lung disease
Infection
Connective tissue disease
Cancer
Catamenial pneumothorax |
PATHOPHYSIOLOGY
Under normal conditions, the parietal and visceral pleura are in close apposition. The pleural space is negatively pressured at –5 mm Hg with fluctuations of 6 to 8 mm Hg between inspiration and expiration. The inherent tendency of the chest wall is to expand and for the lungs to collapse from elastic recoil. With the loss of the normal negative pressure in the pleural space that “adheres” the visceral pleura (lungs) to the parietal pleura (ribs), the affected lung collapses. A primary spontaneous pneumothorax occurs when a subpleural bleb ruptures, disrupting pleural integrity. Rupture in primary spontaneous pneumothoraces usually involves the lung apex.6,7,8 In secondary spontaneous pneumothoraces, disruption of the visceral pleura occurs secondary to underlying pulmonary disease processes.
Once there is a break in the visceral pleura, air travels down a pressure gradient into the intrapleural space, until pressure equilibrium occurs with partial or total lung collapse. Altered ventilation–perfusion relationships and decreased vital capacity contribute to dyspnea and hypoxemia. If air continues to enter the pleural space, intrapleural pressure becomes positive. Tension pneumothorax develops as inhaled air accumulates in the pleural space but cannot exit due to a check-valve system. As intrathoracic pressure (>15 to 20 mm Hg) increases, the great vessels and heart are compressed and shifted contralaterally, severely restricting venous return, diastolic filling, and cardiac output causing ventilation-perfusion mismatch, and resulting in hypoxia and shock.8 Tension pneumothorax can develop in the presence of a chest tube if gas egress is obstructed, including from the adjacent lung.
CLINICAL FEATURES
Classic symptoms of primary spontaneous pneumothorax are sudden onset of dyspnea and ipsilateral, pleuritic chest pain. The pleuritic component of the pneumothorax may resolve within the first 24 hours. Profound dyspnea is rare, unless the patient has poor reserve due to underlying parenchymal disease or develops a tension pneumothorax. Sinus tachycardia is the most common physical finding. Because many pneumothoraces are small, other classic findings like ipsilateral decreased breath sounds, hyperresonance to percussion, and decreased or absent tactile fremitus are absent. In traumatic pneumothorax, the positive predictive value of ipsilateral decreased breath sounds is 86% to 97% for the diagnosis.9 Cough and exertional complaints are not common signs or symptoms.2 Except for trauma, physical exam alone is not sensitive enough to exclude the diagnosis.
The clinical hallmarks of tension pneumothorax are tracheal deviation away from the involved side, hyperresonance of the affected side, hypotension, and significant dyspnea.8
DIAGNOSIS
Pneumothorax is an important differential consideration in patients with chest pain, especially in those with underlying lung disease. Patients with pleurisy, pleural effusions, infiltrates, or shingles can present with pain similar to those with pneumothorax.
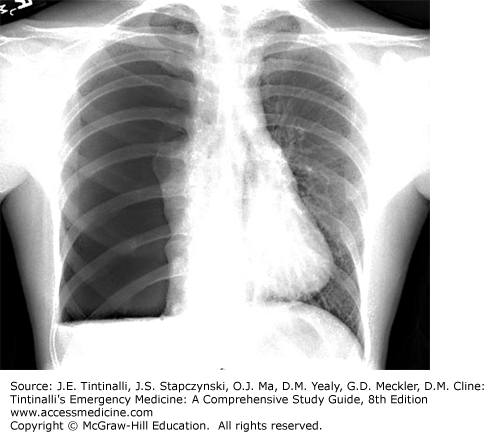
A standard erect posteroanterior chest radiograph is the usual initial test and demonstrates loss of lung markings in the periphery and a pleural line that runs parallel to the chest wall (Figure 68-1). Ensure that the line does not extend outside of the chest cavity, suggesting a confluence of shadows or skin line. A lateral radiograph will identify a pneumothorax in an additional 14% of cases.10 An expiratory radiograph does not identify many additional pneumothoraces. The sensitivity of anteroposterior chest radiography, when compared with CT, was 75.5% (95% confidence interval, 61.7% to 86.2%), with a specificity of 100% (95% confidence interval, 97.1% to 100%).10,11,12 In critically ill patients, when they cannot be moved to an erect position, look for the deep sulcus sign, a deep lateral costophrenic angle, on the affected side.
Large bullae in patients with chronic obstructive pulmonary disease may look like a pneumothorax, although a pneumothorax pleural line will run parallel with the chest wall, whereas bullae will have a medially concave appearance. Pneumothoraces usually cross more than one lung segment, whereas bullae are limited to a single lobe. A chest CT can differentiate the two. A thoracostomy with the chest tube inserted into a bulla mistaken for a pneumothorax results in a large pneumothorax, associated bronchopulmonary fistula, and its complications.12 Pleural adhesions cement the visceral and parietal pleura together, changing the appearance of the pneumothorax.
Pneumothorax size may be calculated by the Light index or Collins or Rhea methods, but most published formulae show only a modest correlation to actual pneumothorax size.13,14,15,16 The American College of Chest Physicians supports a method of measurement from the apex of the lung to the cupula of the thoracic cavity on an upright posteroanterior film.17 A measurement of less than 3 cm in this cephalad area is considered a small pneumothorax. Another method is to measure the interpleural distance at the level of the hilum; in this area, a distance of 2 cm correlates with a pneumothorax of approximately 50% by volume.18 The British Thoracic Society defines a small pneumothorax as one with a <2-cm rim between the lung edge and chest wall and a large pneumothorax as one with a ≥2-cm rim.18
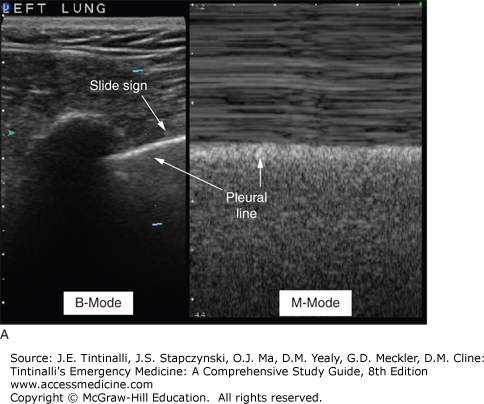
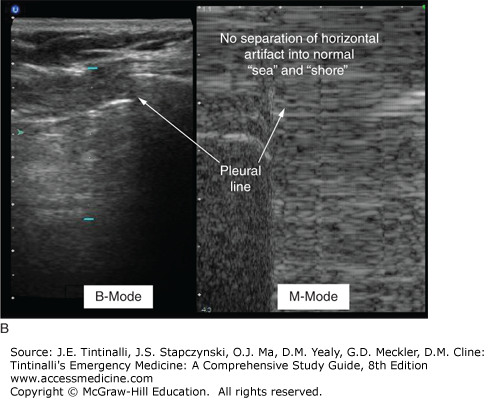
US detects traumatic pneumothorax, with a reported sensitivity of 98.1% (95% confidence interval, 89.9% to 99.9%) and specificity of 99.2% (95% confidence interval, 95.6% to 99.9%).13 The movement of the lung (ocean) against the stationary chest wall (shore) is often referred to as the “seashore.” In a normal lung, there is commonly a sonographic reverberation distal to the pleura that looks like a comet tail and a sliding sign of the movement of the visceral pleura along the parietal pleura (Figure 68-2). In the presence of intrapleural air, pleural adhesions, effusions, and parenchymal disease, small pneumothoraces may be loculated, and therefore, the sliding sign and the comet tail reverberation are lost, limiting the specificity for pneumothorax.14,15
Chest CT detects between 25% and 40% of pneumothoraces not visualized on a postprocedure chest radiograph.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree