
Pneumonia
Gregory J. Moran and David A. Talan
In the United States, more than 3 million persons contract community-acquired pneumonia (CAP) annually, resulting in about 500,000 hospital admissions. Pneumonia is the most common infectious cause of death in the United States. Most deaths occur in the elderly or immunosuppressed, but pneumonia also occurs in otherwise healthy persons. To manage patients with pneumonia successfully, emergency physicians must maintain an awareness of the expanding spectrum of pathogens, changing antibiotic-resistance patterns, and availability of new antimicrobial agents.
Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, and viruses continue to be the most common causes of CAP, with Legionella sp and Chlamydophila pneumoniae less frequently diagnosed (1). Less common etiologies include gram-negative bacilli and oral anaerobes. Staphylococcus aureus was considered an uncommon cause of CAP, but recent studies indicate it is among the more common pathogens, particularly in seriously ill patients (2). Pneumocystis jirovecii (previously known as P. carinii) and Mycobacterium tuberculosis are important as pathogens related to pulmonary infections in patients with acquired immunodeficiency syndrome (AIDS). Knowledge of local prevalence patterns for pathogens of CAP is important to make appropriate choices regarding evaluation and treatment.
CLINICAL PRESENTATION
Typical and Atypical Pneumonias
Pneumonia is often divided into typical (pyogenic bacterial) and atypical categories, but this division is somewhat artificial. Prediction of these etiologies based on clinical and radiographic findings is inaccurate. The classic presentation of typical pyogenic bacterial pneumonia is the abrupt onset of fever and chills, followed by development of productive cough with purulent sputum and pleuritic chest pain. Elderly or debilitated patients can present with nonspecific complaints, such as altered mental status. Tachypnea and tachycardia are usually present. Physical examination signs of pneumonia include findings of consolidation such as dullness to percussion, coarse rales, bronchial breath sounds, or increased tactile fremitus.
The atypical pneumonia syndrome is caused by organisms such as M. pneumoniae, C. pneumoniae, viruses, Legionella sp, or rickettsial organisms such as Coxiella burnetii. Patients with this type of pneumonia generally present with a subacute onset of systemic complaints, such as fever, headache, malaise, and myalgias, associated with a nonproductive cough. Although mucopurulent sputum generally indicates the presence of pyogenic bacterial pneumonia or bronchitis, it can also be present with mycoplasmal or viral pneumonia. Chest examination often reveals scattered rhonchi or rales. Signs of consolidation are less common.
The high degree of overlap between the clinical and radiographic features of typical pyogenic and atypical pneumonia makes it impossible to accurately predict the specific type of pneumonia. Typical and atypical pathogens sometimes coexist in the same patient, and bacterial infections often coexist or follow viral respiratory infections. It is usually not possible to determine the specific etiology of pneumonia within the timeframe of an emergency department (ED) evaluation, however, certain clinical factors can suggest a likely etiology and guide empiric therapy. The clinical characteristics of several types of pneumonia are noted next.
Common Etiologies
S. pneumoniae is the single most common identified etiologic agent among adults with CAP. The classic presentation of pneumococcal pneumonia is the abrupt onset of a single shaking chill, followed by fever, cough productive of rust-colored sputum, and pleuritic chest pain. However, many patients have a more insidious onset. Patients with a history of asplenia, sickle-cell disease, AIDS, multiple myeloma, or agammaglobulinemia are at increased risk of pneumococcal bacteremia and sepsis. Extrapulmonary complications such as meningitis, endocarditis, or arthritis occasionally develop.
In a recent study of hospitalized ED patients, staphylococcal pneumonia was the second most common identified etiology of CAP. Although CAP due to methicillin-resistant S. aureus (CA-MRSA) occurred in less than 3% overall, patients were distinctly more seriously ill and had chest radiographs with cavitation characteristic of necrotizing pneumonia (2). Intravenous (IV) drug users can present with pneumonia due to septic emboli from hematogenous spread of S. aureus (often associated with tricuspid-valve endocarditis), and with multiple small bilateral infiltrates.
H. influenzae is a common pathogen in adults with chronic obstructive pulmonary disease (COPD), alcoholism, malnutrition, malignancy, or diabetes. Moraxella catarrhalis is a gram-negative rod that can be found in patients with COPD and appears to be associated with exacerbations of chronic bronchitis much more frequently than it is associated with pneumonia.
Klebsiella pneumoniae is a rare cause of CAP, but it can cause severe pneumonia in debilitated patients with alcoholism, diabetes, or other chronic illness. Pseudomonas aeruginosa is also uncommon, but it can be present in patients with underlying lung disease, such as bronchiectasis or cystic fibrosis, or in patients who have recently been in a hospital or nursing home.
C. pneumoniae is a relatively common etiology of CAP, accounting for at least 8% of cases in adults; however, this is probably an underestimate because of the difficulty in diagnosing infection with this organism. Most infections in young adults cause a minor, self-limited upper-respiratory illness; radiographically evident pneumonia is more common in the elderly, in contrast to the common perception that atypical pneumonias occur in the young.
M. pneumoniae is one of the most common causes of CAP in previously healthy patients <40 years of age. It tends to be a more mild illness, with extrapulmonary manifestations such as maculopapular, vesicular, urticarial, or erythema-multiforme–type rashes and rarely pericarditis, glomerulonephritis, aseptic meningitis, and Guillain–Barré syndrome. Many patients complain of sore throat or ear pain, but the classic finding of bullous myringitis is less common and is nonspecific. Legionella sp is an intracellular organism that lives in aquatic environments, including tap water. There is no person-to-person transmission but outbreaks can occur due to a common water-related point-source exposure. Some patients present with a mild, self-limited atypical pneumonia, but older patients with chronic disease are at risk for more severe systemic illness. Gastrointestinal symptoms such as diarrhea are often prominent.
Winter influenza outbreaks, usually caused by influenza type A, result in an average of 20,000 deaths yearly in the United States, mostly among persons age 65 years or older (3). Cytomegalovirus (CMV) can cause pneumonia in persons with severe immunosuppression (e.g., transplant recipients). Varicella zoster virus (chickenpox) may rarely cause pneumonia; it is seen more often in adults and especially with pregnancy. Periodically, new viral pneumonia threats emerge in various parts of the world, including avian influenza strains, some with high case fatality, and novel coronaviruses. Emergency physicians should be aware of newly emerging pathogens, and screen for geographic exposures when appropriate. Up-to-date information on outbreaks can be found on the US Centers for Disease Control and Prevention (CDC) website, cdc.gov.
Although P. jirovecii pneumonia (PCP) does not occur in normal hosts, the possibility of opportunistic infection and unrecognized AIDS must always be considered. Many patients are unaware of their human immunodeficiency virus (HIV) status. All patients who present with pulmonary complaints should be questioned about HIV risk factors, and clinicians should search for signs of immunosuppression, such as weight loss, lymphadenopathy, and oral thrush. PCP typically presents subacutely with fatigue, exertional dyspnea, nonproductive cough, pleuritic chest pain, and fever.
Lower-respiratory infection caused by anaerobic organisms generally results from the aspiration of oropharyngeal contents. These infections are typically polymicrobial, including many anaerobes such as Peptostreptococcus sp, Bacteroides sp, Fusobacterium sp, and Prevotella sp. Clinical factors that suggest an anaerobic infection include risk for aspiration (e.g., central nervous system depression or swallowing dysfunction), severe periodontal disease, fetid sputum, and radiographic appearance (e.g., location in posterior segment of right upper lobe or superior segment of lower lobe, lung abscess).
Fungal infections caused by organisms such as Histoplasma capsulatum, Blastomyces dermatitidis, and Coccidioides immitis commonly present as pulmonary disease. These organisms are present in the soil in various geographic areas of the United States: H. capsulatum in the Mississippi and Ohio River valleys, B. dermatitidis in a poorly defined area extending beyond that of H. capsulatum, and C. immitis in desert areas of the Southwest. These infections should be considered in persons in appropriate geographic areas, especially those near activities that disturb the soil (e.g., construction, dirt bike riding), or those who fail to respond to antibacterial treatment. The clinical presentation ranges from an acute or chronic pneumonia to an incidental finding of asymptomatic granulomas on chest radiography.
Unusual Causes of Pneumonia
Hantaviruses have been associated with a syndrome of severe respiratory distress (hantavirus pulmonary syndrome) and shock that has occurred in persons in several areas of the United States. Infection appears to occur from inhalation of aerosols of material contaminated with rodent urine and feces. Characteristic laboratory findings include thrombocytopenia, hemoconcentration, leukocytosis, and mild elevation of hepatic transaminases. The chest radiograph demonstrates bilateral interstitial lung infiltrates that are more pronounced in dependent areas. While there is no known effective antiviral therapy, if the patient can be adequately supported, including the use of extracorporeal membrane oxygenation (ECMO) if necessary, then recovery is usually complete.
Plague, caused by Yersinia pestis, is endemic in many parts of the world and has been implicated as an organism that could be used in biologic terrorism. Plague occurs in the southwestern states of the United States in persons bitten by fleas from infected rodents or carnivores. Hematogenous spread may lead to severe pneumonia that is highly contagious.
Anthrax (caused by Bacillus anthracis) has been used as an agent of biologic terrorism. Inhalation of anthrax spores can cause a syndrome that presents as severe sepsis with or without pneumonia and meningitis. Chest radiography may reveal a wide mediastinum caused by swelling of mediastinal nodes.
Tularemia is a febrile illness, caused by Francisella tularensis, that is spread by contact with body fluids of infected mammals (especially rabbits) or the bite of an infected arthropod. The illness usually begins with an ulcerated skin lesion and painful regional lymphadenopathy. Some patients have a typhoidal form, with only fever, malaise, and weight loss. Pneumonia can occur with either form.
Psittacosis is a chlamydial infection that can be spread to humans from infected birds. Illness often begins rapidly with chills, high fever, myalgias, and nonproductive cough; severe headache is often the major complaint.
Q fever is an acute febrile illness caused by the rickettsial organism C. burnetii that may present as pneumonia, often with severe headache. Q fever is most common in persons with occupational exposure to animals.
DIFFERENTIAL DIAGNOSIS
Cough is a very common presenting complaint; however, only a small fraction of patients presenting with cough have pneumonia. Most patients with acute cough have a viral upper-respiratory infection or bronchitis. Several noninfectious etiologies can also result in inflammatory lung processes. These include exposure to mineral dusts (e.g., silicosis), chemical fumes (e.g., chlorine, ammonia), toxic drugs (e.g., bleomycin), radiation, thermal injury, or oxygen toxicity. Immunologic diseases such as sarcoidosis, Goodpasture syndrome, and granulomatosis with polyangiitis (GPA, previously known as Wegener’s) may cause pneumonia. Tumors can mimic pneumonia radiographically or present initially as a postobstructive infection. Pulmonary emboli and infarcts must be considered in patients who present with tachypnea, hypoxia, tachycardia, or chest pain in the appropriate clinical setting. Cardiac illness often presents with respiratory complaints such as dyspnea. Aspiration of a foreign body may cause a focal pulmonary infiltrate, and should be considered in at-risk patients (e.g., toddler).
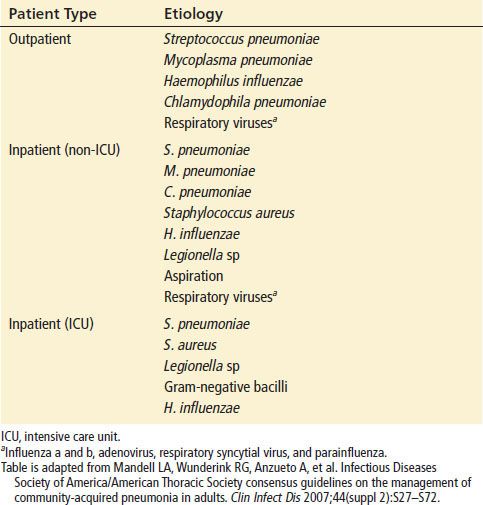
No microbial etiology can be determined in one-third to one-half of CAP cases, even after thorough investigation. To a great extent, the likely etiologies must be predicted based on epidemiologic considerations and prevalence of pathogens in research studies (Table 74.1). In general, the likelihood of S. pneumoniae is higher with greater severity of illness, accounting for as many as 50% of intensive care unit (ICU)-admitted and fatal cases, with CA-MRSA also now associated with severe disease. Atypical organisms such as viruses and Mycoplasma sp account for a relatively higher proportion of pneumonias in those who have milder illness amenable to outpatient therapy.
TABLE 74.1
Most Common Etiologies of Community-Acquired Pneumonia
ED EVALUATION
ED evaluation should focus on establishing the diagnosis of pneumonia, identifying host factors that will influence decisions regarding the need for hospitalization, and determining the presence of clinical features associated with specific infectious etiologies that will guide choice of antibiotics. In most healthy older children and adults, the diagnosis of pneumonia can be reasonably excluded on the basis of history and physical examination, with suspected cases further evaluated by chest radiograph. Absence of any abnormalities in vital signs or chest auscultation substantially reduces the likelihood of pneumonia. No single clinical finding is highly reliable in establishing or excluding a diagnosis of pneumonia (4).
Chest Radiography
The chest radiograph is generally the most important test to determine the presence of pneumonia. Predictive models have been developed to optimize chest x-ray use in patients with cough in whom pneumonia is suspected. Clinical findings found to be associated with radiographically confirmed pneumonia are fever, tachycardia, and tachypnea; rales or decreased breath sounds, sputum production. Absence of rhinorrhea or sore throat have also been predictive in some models. Predictive models can reduce unnecessary chest x-rays but appear to be less sensitive than physician judgment (5). Chest x-ray, because of its relatively low cost and risk, is appropriate when management will be affected by the result (e.g., hospital admission, antimicrobial use, exclusion of other diagnoses). Chest x-ray can be particularly useful in groups who often have subtle clinical signs of pneumonia, such as the elderly and those at risk for tuberculosis (TB), to quickly establish the need for isolation. Healthy adults who will receive outpatient treatment with empirical antimicrobials can have the chest radiograph deferred unless there is suspicion of immunosuppression or other unusual features of disease. Routine chest radiography for patients with exacerbation of chronic bronchitis or COPD is of low yield and can be limited to those with other signs of infection or heart failure. Computed tomography (CT) of the chest is more sensitive than plain radiography for detecting the presence of pulmonary consolidation, although the natural history of CT-positive, plain-radiograph–negative pneumonia is unclear.
Certain radiographic patterns tend to be associated with specific pathogens. In pyogenic bacterial pneumonias, radiographs usually show an area of segmental or subsegmental infiltration and air bronchograms. Lobar consolidation is present in a minority of cases of bacterial pneumonia and is often caused by pneumococcus or Klebsiella sp. Bronchopneumonia resulting from spread of infection along the intralobular airway causes fluffy or patchy infiltrates in the involved areas of the lung. Viruses and a wide variety of bacteria can cause this pattern, including C. pneumoniae, M. pneumoniae, Legionella sp. An interstitial pattern on the chest radiograph is typically caused by M. pneumoniae, viruses, or P. jirovecii. Tiny nodules disseminated throughout both lungs represent a miliary pattern typical of granulomatous pneumonias such as due to M. tuberculosis or fungal infection. The location of infiltrates can also give a clue to the etiology. Aspiration pneumonia occurs in dependent areas of the lung, most commonly the superior segments of the lower lobes or the posterior segments of the upper lobes. Pneumonia produced by hematogenous spread (such as due to staphylococci) tends to be multifocal and peripheral. Apical infiltrates suggest TB. An infiltrate associated with hilar or mediastinal adenopathy suggests the presence of TB or fungal disease or pneumonia associated with a neoplasm. Cavitation is most commonly present with infections caused by anaerobes, gram-negative organisms, fungi, or S. aureus: Cavitation can also be present in fungal disease or TB. Pneumatoceles or spontaneous pneumothorax can be seen in AIDS patients with PCP. Pleural effusions can be seen with a wide variety of organisms, including many types of pyogenic bacterial pneumonia, C. pneumoniae, Legionella sp, and TB. Anaerobic infections are especially prone to the development of empyema.
However, despite these characteristic associations, radiographic presentations vary greatly among patients with a specific infection etiology and are also modified by the host response. Immunocompromised patients are particularly likely to have atypical radiographic appearances. Occasionally, patients with a clinical picture strongly suggestive of pneumonia have a normal chest radiograph. The absence of findings on the chest radiograph should not preclude the use of antimicrobial therapy in patients thought to have pneumonia on clinical grounds.
Other Tests
Patients with respiratory complaints should be screened with pulse oximetry at triage because hypoxia may not be otherwise clinically suspected and its presence has therapeutic implications (6). Severe hypoxia is an indication for hospital admission.
Most laboratory studies available in the timeframe of ED care are of limited utility in establishing the diagnosis and specific etiology of pneumonia. Although an elevated peripheral white blood cell (WBC) count can increase the likelihood of a pyogenic bacterial etiology, this finding is of limited value in making decisions regarding therapy in an individual patient and must be considered in light of other clinical and epidemiologic features (i.e., the pretest probability of various etiologies). A WBC count may be helpful if it yields evidence of immunosuppression, such as neutropenia, or if it reveals lymphopenia that may indicate immunosuppression from HIV. Serum lactate dehydrogenase (LDH) can be helpful in evaluating possible PCP in patients at risk of AIDS. Rapid HIV tests are available that can be helpful in this situation. Serum chemistry studies can be helpful in identifying patients with metabolic acidosis or renal–hepatic dysfunction associated with sepsis or with underlying disease that predicts a complicated course and influence decisions regarding disposition, choice of antimicrobial agents, and dosages. In addition, elevated lactic acid levels, even in the absence of fluid-unresponsive hypotension, can indicate the need for early and aggressive hemodynamic resuscitation. These ancillary tests are not necessary in patients with mild illness. B-type natriuretic peptide (BNP) or echocardiography can be helpful in cases in which heart failure is a consideration.
Inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein have not been demonstrated to be helpful in clinical decision-making regarding pneumonia. Procalcitonin level has been suggested as a means to assess risk of a bacterial etiology, response to antimicrobial therapy, and prognosis in pneumonia. However, its utility in the ED, such as to assess need for hospitalization or ICU admission compared to other risk-stratification systems (see below) has not been established (7).
Although a Gram stain of the sputum is often recommended as a means to identify a bacterial pathogen, the use of the Gram stain as a basis for empiric therapy in the ED can be problematic due to difficulty obtaining an adequate sputum specimen and infection control hazards associated with sputum induction. Moreover, correlation between pneumococcal identification on Gram stain and by sputum culture is poor even with an adequate specimen, and Gram stain is even less likely to demonstrate gram-negative pathogens. If sputum Gram stain and culture are considered, they should be reserved for the subset of patients with more serious illness (e.g., admitted to the ICU), in whom the bacteriologic diagnosis is highly uncertain, and for whom it is felt that the outcome may be most dependent on optimal antimicrobial therapy. For example, in the ED, those patients with pneumonia and respiratory failure requiring intubation should have endotracheal suction specimens obtained. Patients with a pleural effusion should have a diagnostic thoracentesis performed, with fluid sent for cell count, differential, pH (pH <7.2 is predictive of a need for chest tube), Gram stain, and culture. Although it is preferred to obtain pleural fluid specimen as early as possible, because of time constraints it is not always possible to perform diagnostic thoracentesis in every patient with pleural effusion in the ED. For most patients, thoracentesis can be safely deferred until after hospital admission. However, patients in significant respiratory distress or with evidence of tension and mediastinal shift require emergent therapeutic thoracentesis.
The utility of routine blood cultures is questionable because studies of nonimmunocompromised adults with pneumonia have demonstrated a low prevalence of noncontaminant bacteremia, and management is rarely changed based on the results (8–10). The follow-up of false-positive blood cultures can be costly, labor intensive, and may lead to unnecessary use of antibiotics such as vancomycin or linezolid when results are initially reported as gram-positive cocci. Blood cultures should be obtained from immunocompromised patients, those with severe sepsis or shock, or those with risk factors for endovascular infection (e.g., prosthetic valves or IV drug use). When cultures are drawn, they should be obtained prior to the initiation of antibiotics (although antibiotics should not be delayed for this reason).
Serologic tests are available for the diagnosis of a number of organisms, including C. pneumoniae, Legionella sp, and fungi. Serologic tests to determine the etiology of pneumonia may be helpful retrospectively, but both acute and convalescent serum titers are usually required; therefore, they are of little use to the emergency physician. Urine-antigen tests for organisms such as S. pneumoniae and Legionella sp can give results quickly. Rapid diagnostic tests for viral antigens are available for several viruses, including RSV and influenza. These tests may be useful for infection-control decisions in hospitalized patients and may provide an indication for influenza therapy. In the future, rapid testing using technology such as the polymerase chain reaction may provide emergency physicians with a reliable method for determining the specific etiology of pneumonia.
KEY TESTING
• Chest radiograph
• Pulse oximetry
• For seriously ill patients:
• Blood culture
• Serum lactate level
• Complete blood count
• Chemistry profile
• Blood and sputum culture









