
Pleural Effusion
Micelle Haydel
The visceral and parietal pleura are serous membranes that line the outer surface of the lung, mediastinum, diaphragm, and the inner surface of the thoracic wall, forming the right and left pleural spaces. Under normal homeostatic conditions, the parietal pleura secretes about 0.01 mL/kg/hr of pleural fluid which is continuously resorbed by the pleural lymphatics, maintaining a steady state of less than 10 mL in the pleural space (1). About 30% of healthy men have 3 to 5 mm of fluid visible on ultrasound, whereas 80% of women have up to 5 to 7 mm visible on MRI (2,3). A pleural effusion occurs when fluid formation increases beyond the capacity of lymphatic clearance, or when lymphatic clearance is impaired. Pleural fluid has a chemical composition similar to that of interstitial fluid, but is altered in the setting of inflammation, infection, malignancy, or trauma. Fluids that collect in the pleural space include transudative, exudative, hemorrhagic, and chylous.
CLINICAL PRESENTATION
The clinical presentation of pulmonary effusions ranges from incidental findings to life-threatening cardiopulmonary distress or sepsis. Patients with a pleural effusion often present with complaints related to the underlying disease process rather than to the pleural effusion itself. Pleural effusions are graded as small when up to 25% of the pleural cavity is involved, moderate when 25% to 50% is involved, and large when more than 50% is involved (4). Signs and symptoms in patients with pleural effusion vary based on the size and cause of the effusion, as well as associated underlying disease processes.
• Fever: A pleural effusion caused by infection is typically associated with fever.
• Pain: Inflammation of the parietal pleura causes referred pain to the overlying chest wall, whereas irritation of the diaphragmatic pleura causes referred pain to the ipsilateral shoulder. The visceral pleura is not innervated, therefore does not cause pain.
• Cough: Lung compression with bronchial irritation can cause a nonproductive cough.
• Dyspnea: Large pleural effusions can compromise pulmonary mechanics, impair gas exchange and cause dyspnea, tachypnea, and respiratory distress. A pulmonary embolism or infarct often will cause dyspnea that is out of proportion to the associated effusion.
• Tachycardia and hypotension: A large pleural effusion can cause cardiac collapse during diastole, physiologically mimicking cardiac tamponade.
• Weight loss: The review of systems often reveals unexplained weight loss in patients with tuberculosis, malignancy, and HIV.
• Ascites: Cirrhosis, ovarian cancer, and Meigs syndrome are associated with ascites.
• Size: The size of an effusion can suggest its etiology. Large or massive effusions are associated with malignancy, but can also be found in tuberculosis and bacterial parapneumonic effusions.
• Laterality: Most bilateral effusions are caused by a transudative process, such as heart failure, renal or hepatic failure, or low protein states. Bilateral effusions are rarely seen in malignancy, pulmonary embolism, and rheumatoid arthritis. When bilateral effusions are of unequal size, more than one etiology should be suspected.
DIFFERENTIAL DIAGNOSIS
Pleural effusions are quite common, diagnosed in over 1 million patients each year in the United States (5). Over 50 etiologies are known, and in the United States the most common causes are heart failure, pneumonia, malignancy, and pulmonary embolism (6). In children, pneumonia is the most common cause of pulmonary effusion. The medical history and symptoms (or lack thereof) can be very helpful in developing a differential diagnosis and management plan. The most common causes of pleural effusions include the following.
• Congestive heart failure: Over 80% of patients with decompensated CHF have some degree of bilateral or unilateral transudative pleural effusions due to elevated pulmonary capillary pressure (7,8).
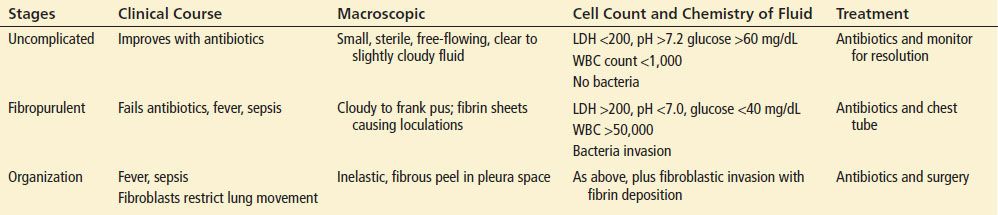
• Pneumonia: About 40% of patients with bacterial pneumonia have an exudative pleural effusion, known as a parapneumonic effusion. Most are uncomplicated and resolve with antibiotic therapy, but about 1% progress to an empyema with the potential for rind formation and constrictive pleuritis (9). Parapneumonic effusions are further classified in Table 75.1.
TABLE 75.1
Stages of Parapneumonic Effusion
• Malignancy: Patients with malignant effusions typically present with a complaint of dyspnea or chest pain. Malignant cells in a pleural effusion imply disseminated disease and a reduced life-expectancy. Malignant effusions tend to recur within a month of being drained, with lung and breast cancer accounting for ∼60% of malignant effusions (10). Paramalignant effusions are caused by lymphatic obstruction, superior vena cava syndrome, or postobstructive atelectasis; but do not involve pleural metastasis (11). Malignant effusions can be hemorrhagic or chylous (lymphoma).
• Pulmonary embolism: One-third to one-half of patients with pulmonary embolism have a small, unilateral, frequently hemorrhagic, exudative effusion (12). Dyspnea is typically out of proportion to the size of the effusion, and the presence of pleuritic pain and a pleural effusion is suggestive of pulmonary embolism (6,13).
Less common causes of pulmonary effusions are very diverse, but the past medical history and physical examination can offer important diagnostic clues and include the following.
• Tuberculosis: In the United States about 5% of patients with tuberculosis have plural effusions, but in countries with a higher prevalence of tuberculosis, TB is often the primary cause of pulmonary effusions (14).
• HIV: Pulmonary effusions are frequently found in hospitalized patients with HIV, most commonly due to infections (including tuberculosis) and malignancy (lymphoma and Kaposi) (15). Parapneumonic effusions in patients with HIV are caused by the bacteria encountered in the general population, as well as Mycobacterium, Pneumocystis, Cryptococcus, and Histoplasmosis.
• Cirrhosis, ascites, and peritoneal dialysis are all associated with transudative pleural effusions due to the imbalance of pleural oncotic and hydrostatic forces.
• Nephrotic syndrome can cause a transudative pleural effusion, but the associated hypercoagulable state also predisposes to pulmonary embolism.
• Trauma and postsurgical: While small left-sided pleural effusions are expected in the first week post-CABG, up to 10% of patients will develop moderate to large or persistent effusions (16). Large pleural effusions develop after a complete pneumonectomy. Potentially lethal causes of pleural effusions include hemothorax and ruptured esophagus.
• Disruption of the thoracic duct (due to trauma or malignancy) causes a chylous effusion due to fatty acids that give lymphatic fluid a milky appearance.
• Autoimmune diseases such as lupus, rheumatoid arthritis, and sarcoidosis are rare causes of pleural effusions.
• Drug induced: Numerous medications have been associated with a pleural effusion. Most resolve with cessation of the culprit drug, but some continue long after the medication has been stopped. The most common drugs associated with pleural effusion are methotrexate, phenytoin, nitrofurantoin, β-blockers, and amiodarone (6). Procainamide and hydralazine can cause lupus syndrome with effusions. Ovarian hyperstimulation syndrome secondary to infertility treatments can cause pulmonary effusions.
• Sympathetic effusion: Virtually any abdominal infection or inflammatory process can alter the surrounding capillary permeability leading to an effusion. Examples include pancreatitis, hepatitis, cholecystitis, hepatic amebiasis, splenic abscess, pyelonephritis, glomerulonephritis, peritonitis, pelvic inflammatory disease, and abdominal abscess.
ED EVALUATION
The physical examination of a patient with a pleural effusion can be benign or markedly abnormal, depending on the size of the effusion. As the pleural space fills with fluid, the involved cavity increases in total volume while the lung parenchymal volume decreases. The chest may be visibly asymmetrical with bulging or retraction of the intercostal spaces, and tracheal deviation. The cardiac apical pulse may be displaced due to a shift in the heart’s location due to fluid accumulation. Diminished breath sounds and/or a pleural rub may be appreciated. Dullness to percussion and tactile fremitus are the most useful physical examination signs of pulmonary effusion (17). The change in the sound of percussion can identify the upper limit of a pleural effusion.
Upright posteroanterior (PA) and lateral chest radiographs should be part of the initial evaluation of the patient with suspected pleural effusion. The subpulmonic space is the most dependent area of the diaphragm below the lungs where effusions initially collect. Easily mistaken for an elevated hemidiaphragm, a 25- to 50-mL subpulmonic effusion is seen as a shifting of the peak of the right diaphragm laterally (see arrow in Fig. 75.1) or an increased distance between gastric bubble and left lobe lung on upright PA chest film. Blunting of the costophrenic angles can be seen on the lateral film when more than 50 mL of fluid has collected, and can be seen on the PA film when more than 150 mL has collected. A meniscus can typically be seen on the PA film when 200 mL has collected, and when 500 mL has collected the diaphragm is obscured (18). Lateral decubitus films (Fig. 75.2) are useful to determine layering of the fluid, and a dependent fluid layer more than 10 mm thick is considered significant.

FIGURE 75.1 Subpulmonic effusion. Note (arrow) shifting of the peak of the diaphragm laterally. (From Crapo JD, MD, Glassroth J, MD, Karlinsky JB, MD, MBA, et al. Baum’s Textbook of Pulmonary Diseases. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.)









