(1)
Chennai Breast Centre, Chennai, India
Phyllodes tumor is a fibroepithelial neoplasm that histologically resembles a fibroadenoma and has potential to grow to a large size. The term cystosarcoma phyllodes was originally coined by Johannes Muller in 1838. The spectrum of phyllodes lesion varies from a lesion that resembles a fibroadenoma in their least aggressive form to a sarcomatous lesion with metastatic potential. Considering the lack of clarity in the terminology used, the World Health Organization (WHO) in 1982 recommended that these lesions be termed as phyllodes tumors, and this has been widely accepted in clinical practice.
Phyllodes tumors are rare. They constitute about 2–3 % of all fibroepithelial lesions, and cystosarcoma phyllodes constitutes 0.3–0.9 % of all breast tumors. They occur in women in their 40s, a decade later than the peak incidence of fibroadenoma. They may be benign, borderline, or malignant. Nearly two-thirds are benign, about 15 % are borderline, and 10 % are malignant. Both benign and malignant phyllodes tumors recur locally, and high-grade tumors have 25 % incidence of hematogenous metastasis. Differentiation between benign and malignant phyllodes can only be made with histology. The important clinical concern about phyllodes tumor is that there is no correlation between the histological findings and clinical presentation.
Clinical Features
Phyllodes tumors are usually single, unilateral, painless, palpable breast masses. On clinical examination the phyllodes tumors feel firm and well circumscribed like a fibroadenoma and may be large when first detected. It is impossible to differentiate smaller phyllodes tumor from fibroadenoma clinically. Features that alert a clinician to phyllodes include:
1.
Older age of the patient (patient in their 40s)
2.
Larger tumor size
3.
History of rapid growth
Phyllodes should certainly be considered as a possibility in a middle-aged woman presenting with a rapidly enlarging breast mass. The rapidity of growth may produce visible bulging when it expands quickly causing shiny, stretched skin with dilated veins over the mass as it pushes against the skin. The skin may ulcerate secondary to ischemia from pressure on the overlying skin. The nipple also may appear effaced but never inverted or retracted. The rapid growth by itself does not indicate malignant potential.
Mammographic Features
Most phyllodes tumors appear as circumscribed, lobulated, high-density masses (Fig. 20.1). Calcifications are not common, but when they are present, they are usually coarse and large. Smaller lesions are indistinguishable from other benign lesions on mammography. It is also not easy to differentiate a benign from malignant phyllodes on a mammogram. The size of the lesion is probably the best correlate to suggest malignancy. Lesions measuring 3 cm or more are statistically more likely to be malignant than those that are less than 3 cm in size (Figs. 20.2 and 20.3).
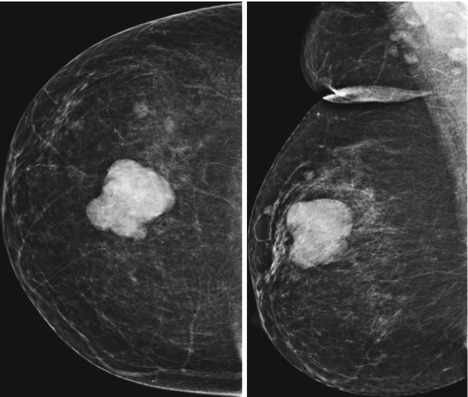

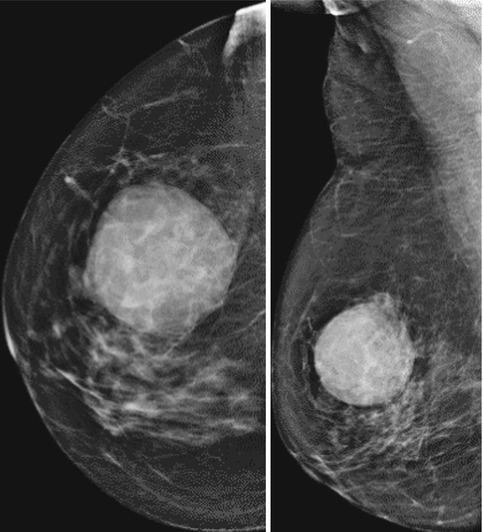
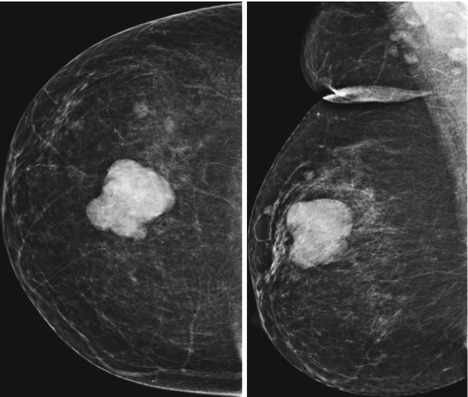
Fig. 20.1
Right breast CC and MLO views showing a dense mass with lobulated margins in the upper quadrant

Fig. 20.2
Mammogram showing a large dense mass with lobulated margins
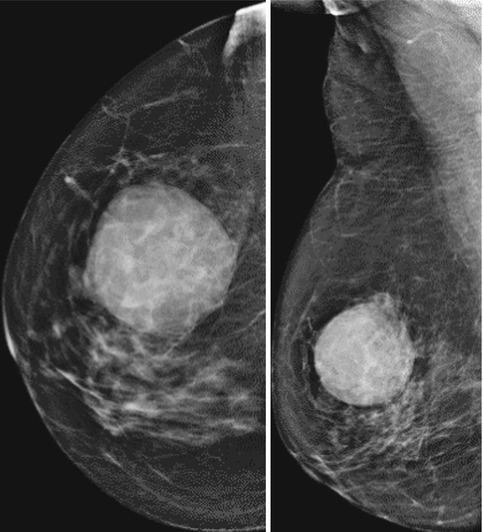
Fig. 20.3
Right breast CC and MLO views showing a large dense rounded mass lesion with partly indistinct margins
Ultrasound Features
Sonographic features of phyllodes tumors are again mostly indistinguishable from fibroadenoma (Fig. 20.4). In most cases they are mild to moderately hypoechoic with well-circumscribed, thin echogenic capsule. The high stromal cellularity of phyllodes tumor results in acoustic enhancement rather than shadowing on ultrasound. There are slit-like spaces seen within the lesion which are due to cystic necrosis (Fig. 20.5). The distinction between malignant and benign phyllodes is also rather difficult. Larger lesions, angular margins, and large cystic spaces are indicative of hemorrhagic cystic necrosis and also indicate the possibility of malignant phyllodes tumor. Color Doppler usually shows marginal and intralesional vascularity (Fig. 20.6).
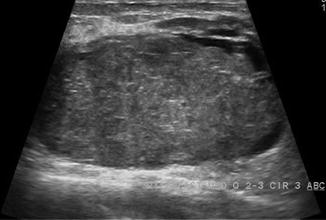
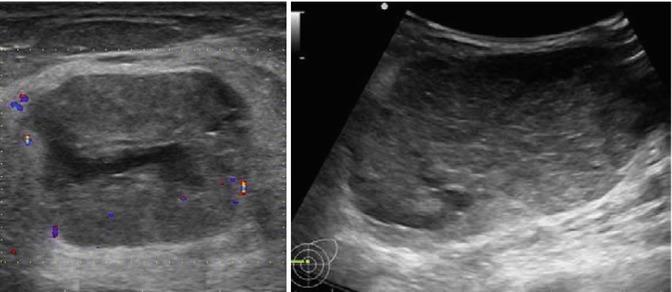
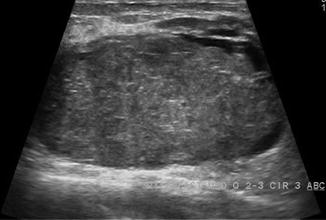
Fig. 20.4
A large well-circumscribed ovoid hypoechoic lesion. Cleft-like cystic spaces noted along the periphery of the lesion
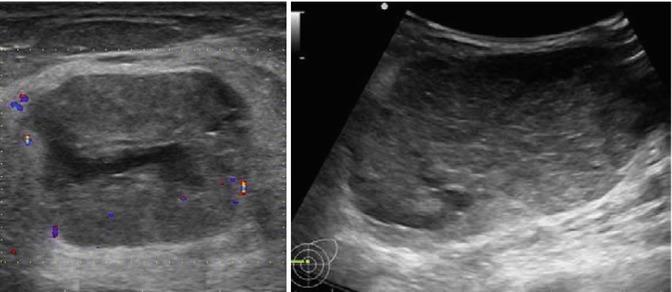
Fig. 20.5




Ultrasound shows a large well-circumscribed ovoid heterogeneous hypoechoic lesion with cystic cleft-like space
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







