Pharmacology of Procedural Sedation
Vince Teo
Choosing Medications for PSA
Procedural sedation has relied on a variety of pharmacological agents for the following:
Give sedation (sedatives).
Relieve pain (analgesics).
Cause a dissociative state (dissociative agents).
These agents, either alone or used in combination allow the patient to better tolerate any pain or discomfort associated with the procedure.
The ideal pharmacological agent for procedural sedation is able to produce:
Optimal sedation and analgesia rapidly.
Has a short duration of action to facilitate a quick recovery without recollection of procedure.
Does not cause any adverse events (such as respiratory depression).
Current classes of medication employed include:
Benzodiazepines (e.g., midazolam).
Opioids (e.g., fentanyl and morphine).
Propofol.
Etomidate.
Ketamine.
Agents for Use in Procedural Sedation (Table 3.1)
Midazolam
Benzodiazepines promote the binding of the inhibitory neurotransmitter, gamma-aminobutyric acid (GABA) to GABA receptors, enhancing their activity.
Midazolam is similar to other benzodiazepines exhibiting the following properties:
Sedation.
Amnesia.
Anxiolysis.
Anticonvulsant.
Muscle relaxant.
It has a rapid onset and short duration of action without active metabolites.
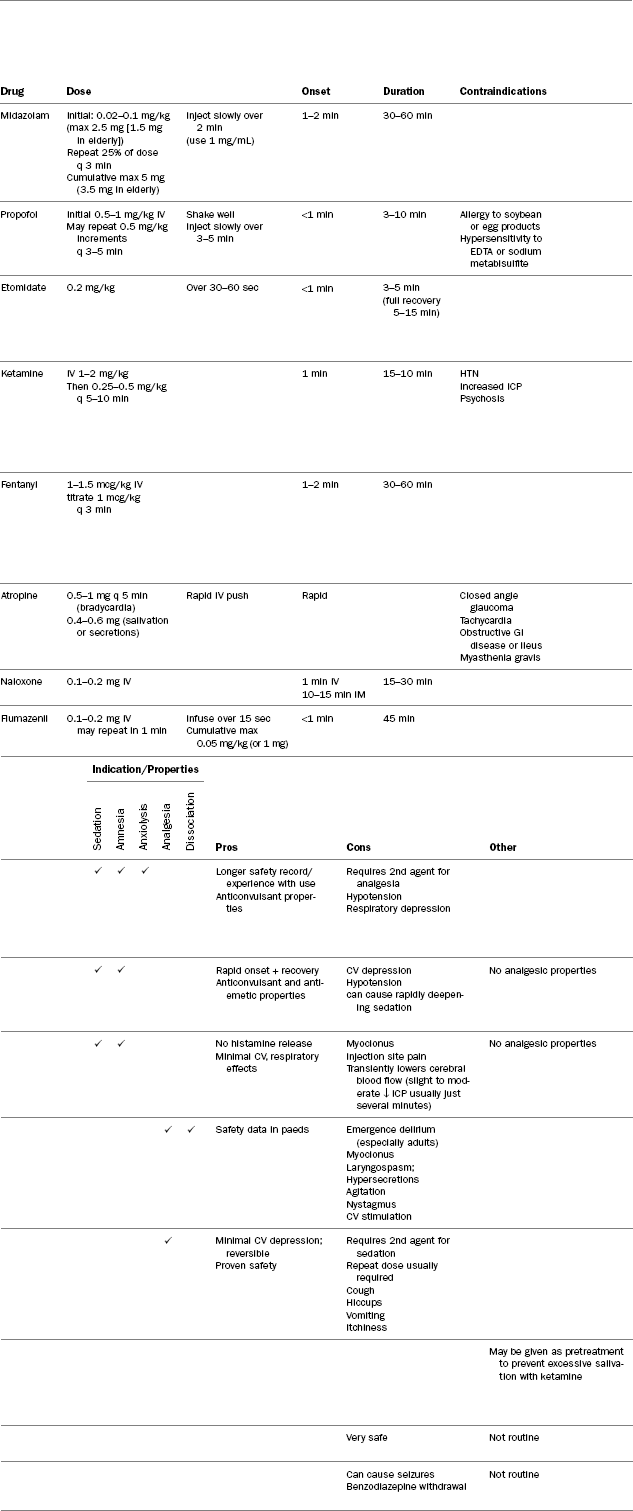
Table 3.1: Medications used for procedural sedation
Dosing:
Initial 0.02–0.1 mg/kg (maximum 2.5 mg [1.5 mg elderly]).
May repeat 25% of dose every 3 minutes (maximum of 5 mg cumulative dose [3.5 mg elderly]).
Availability and administration:
1 mg/mL – 10 mL vial containing 10 mg.
5 mg/mL – 1 mL vial containing 5 mg.
Direct Injection IV slowly over 2 minutes (1 mg/mL concentration should be used to help facilitate this).
Onset:
1–2 minutes.
Duration:
30–60 minutes.
Pharmacokinetics:
Midazolam has a rapid onset and short duration of action without active metabolites.
It is highly lipophilic, resulting in a relatively large volume of distribution (compared to other benzodiazepines).
Thus, its half-life increases significantly in obese patients.
It is metabolized in the liver, a substrate of the CYP3A4 isoenzyme, and is excreted primarily in the urine.
Contraindications:
Hypersensitivity to midazolam or any component of the formulation (benzyl alcohol).
Adverse effects:
Respiratory depression (dose and infusion rate dependent).
Apnea (dose and infusion rate dependent).
Hypotension.
Deep sedation.
Impaired coordination.
Diminished reflexes.
Monitoring:
See Chapter 6 on monitoring during procedural sedation.
Special considerations and pearls:
Wait at least 2 minutes to assess response before administering subsequent doses.
Midazolam does NOT have any analgesic properties.
For painful procedures, consider second agent for analgesia.
Patients premedicated with an opioid (e.g., fentanyl) should have dosages reduced by ∼25%.
Co-administration with other CNS depressants (benzodiazepines, barbiturates, opioids, other sedatives) will increase sedation and the risk of respiratory depression.
Concomitant use of CYP3A4 inhibitors (e.g., azole antifungals, erythromycin, clarithromycin, verapamil, propofol) may increase levels of midazolam.
Patients with hepatic dysfunction or severe CHF may have experienced prolonged effects.
When used in combination with fentanyl, respiratory depression may occur in up to 25% of patients.
Propofol
Propofol is an ultra-short-acting non-opioid, non-barbiturate sedative-hypnotic agent.
Its exact mechanism of action is unknown, but it is thought to enhance the binding of GABA to its receptor sites.
It has sedative, amnestic, anticonvulsant, and anti-emetic properties.
It does not have analgesic properties.
Main benefits are that it has a quick onset and short duration of action resulting in a rapid recovery.
However, due to its potency, there is a risk to the patient of quickly progressing to deep sedation.
Dosing:
Loading dose: 0.5–1 mg/kg IV.
May repeat 0.5 mg/kg IV every 3–5 minutes.
Availability and administration:
10 mg/mL – 20 mL, 50 mL, 100 mL vials available.
Propofol is available as an emulsion. Shake well prior to use.
Inject IV slowly over 3–5 minutes.
Onset:
<1 minute.
Duration of action:
5–10 minutes (full recovery within 10–15 min).
Pharmacokinetics:
Propofol is available in a soybean oil emulsion.
Although it achieves therapeutic concentrations in the CNS rapidly, it is rapidly redistributed to muscle and fat tissue, resulting in an effective duration of action (∼10 min) much shorter than its half-life (15–45 hr).
Contraindications:
Hypersensitivity to soybean oil or egg products. (Emulsifier in the formulation is derived from egg).
Hypersensitivity to EDTA or sodium metabisulfite (preparations of propofol contain either one of these agents as a preservative).
Adverse effects:
Hypotension (may occur in up to 30% of patients).
Bradycardia.
Respiratory depression/apnea (up to 25%).
Site injection pain (15–20%).
A rapid deepening of sedation.
Spontaneous musculoskeletal movements (twitching, jerking or hands, arms, feet and legs) (3–10%).
Monitoring:
See Chapter 6 on monitoring during procedural sedation.
Special considerations:
Strict aseptic technique is important when preparing and administering propofol since the lipid vehicle is capable of supporting bacterial growth.
Propofol does not have analgesic properties – always ensure that analgesic agent is also given to the patient for painful procedures.
If site injection pain is an issue, may pre-inject site with lidocaine.
Hepatic failure – may require lower dosage to be used, as patients may recover more slowly due to decreased elimination.
Monitor closely, as level of sedation can easily progress to deep sedation.
Etomidate
Etomidate is an ultra-short-acting non-barbiturate, non-opioid, non-benzodiazepine sedative-hypnotic.
It has a rapid onset of action, and short recovery time (comparable to propofol).
Furthermore, it does not promote histamine release and has minimal effects on the cardiovascular and respiratory systems, making it an appealing option for procedural sedation.
Dosing:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




