Pediatric Pain Management
Suzan Schneeweiss
Introduction
There is a lack of recognition and treatment of pain in children.
Pain relief for adult patients in the emergency department (ED) is 73% versus 53% for children.
Younger preverbal children generally receive less analgesics than older children.
Medical procedures in the ED are often painful, unexpected, and heightened by stress and anxiety.
Use of analgesic agents allows child to be more comfortable and improves cooperation during diagnostic evaluation.
Appropriate management of pain reduces negative long-term effects of pain which include:
Conditioned anxiety response.
Increased response to pain with subsequent procedures.
Diminished analgesic response at subsequent visit.
“Blood-injection-injury phobia,” which affects up to 25% of adult population.
Pain Assessment
See Chapter 13.
Need to consider the following with a careful pain assessment:
Age of child.
Developmental level.
Cognitive and communication skills.
Previous pain experiences.
Associated beliefs.
Pain history: location, intensity, quality, duration, frequency, duration, and aggravating and relieving factors.
Pain assessment and documentation improves administration of analgesics.
Three Main Methods Are Currently Used to Measure Pain Intensity
Self-report – considered gold standard.
Behavioral measures
Crying, facial expressions, body postures, and movements.
Generally used with neonates, infants, and younger children where communication is difficult.
Physiologic measures
Heart rate, blood pressure, respiration, oxygen saturation, palmer sweating, and sometimes neuroendocrine responses.
Similar physiological responses occur during stress, which result in difficulty distinguishing stress versus pain responses.
Developmental Issues
Children have pain words by 18–24 months (e.g., “hurt,” “ow,” “ouch”).
Word “pain” appears much later in children’s vocabularies.
Children can report degree of pain by 3–4 years.
Children >6 years can provide detailed descriptions of pain intensity, quality, and location.
Pain Scales (See Chapter 13)
FLACC (Face, Legs, Activity, Cry, Consolability)
For infants and children ages 2 months–7 years and cognitively impaired.
See Table 22.1.
Table 22.1: FLACC scale for pain assessment | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
Pain Word Scale
For children ages 3–7 years and older children unable to use numerical rating scale.
“None,” “a little,” “medium,” and “a lot.”
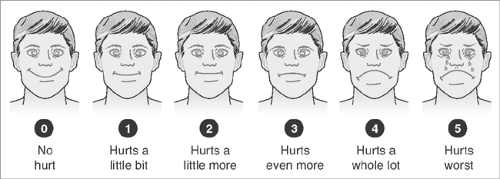
Faces Pain Scale-Revised (FPS-R)
For ages 5–12 years (Figure 22.1).
Point to the face that shows how much you hurt. Score the chosen face 0, 2, 4, 6, 8, or 10, so “0” = no pain and “10” = very much pain.
Numerical Rating Scale
For children >7 years.
Numerical scales from 0–10 or 0–100.
Nonpharmacologic Measures for Pain Management
See Chapter 13.
Neonates and Infants:
Nonnutritive sucking.
Skin to skin contact with the mother (kangaroo care).
Rocking and holding the infant.
Swaddling the infant.
Toddlers and preschoolers
Active distraction: blowing bubbles, providing toys with lots of colors or toys that light up, distracting conservations.
Passive distraction: reading age-appropriate book to child, singing songs, and practicing “blowing out birthday candles.”
Child
Active techniques: blowing bubbles, singing songs, using squeeze balls, relaxation breathing, and playing with electronic devices.
Passive distraction: watching videos, listening to music on headphones, reading a book to the child, or telling them a story.
Adolescent
Ensure private setting.
Allow to choose method of distraction, presence of friends/family.
Active distraction: striking conversation, using squeeze balls, and playing with electronic devices.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree