![]() Clinical suspicion
Clinical suspicion
![]() Swollen/red peritonsillar region causing uvular shift
Swollen/red peritonsillar region causing uvular shift
![]() Fluctuance of area
Fluctuance of area
![]() Interim treatment for peritonsillar closed space infection until tonsillectomy
Interim treatment for peritonsillar closed space infection until tonsillectomy
CONTRAINDICATIONS
![]() Extension into the deep neck tissue
Extension into the deep neck tissue
![]() Septicemia/toxic appearance
Septicemia/toxic appearance
![]() Airway obstruction
Airway obstruction
![]() Severe trismus
Severe trismus
![]() Coagulopathy
Coagulopathy
![]() General Basic Steps
General Basic Steps
![]() Patient preparation
Patient preparation
![]() Analgesia
Analgesia
![]() Visualization
Visualization
![]() Needle aspiration/incision and drainage (I&D)
Needle aspiration/incision and drainage (I&D)
LANDMARKS
![]() Superior lateral border of affected tonsil, or area of most fluctuance
Superior lateral border of affected tonsil, or area of most fluctuance
![]() Aspirate peritonsillar abscess’ (PTA’s) superior pole first, then middle pole, and finally the inferior pole (FIGURE 76.1)
Aspirate peritonsillar abscess’ (PTA’s) superior pole first, then middle pole, and finally the inferior pole (FIGURE 76.1)
TECHNIQUE
![]() Patient Preparation
Patient Preparation
![]() Cooperative patient sitting upright in a chair with occipital support
Cooperative patient sitting upright in a chair with occipital support
![]() Consider intravenous analgesia or sedation
Consider intravenous analgesia or sedation
![]() Digital exam key: Must feel abscess!
Digital exam key: Must feel abscess!
![]() Use ultrasound (endocavitary probe) to assess volume, location, and relationship to the carotid artery (FIGURE 76.2)
Use ultrasound (endocavitary probe) to assess volume, location, and relationship to the carotid artery (FIGURE 76.2)
![]() Needle Aspiration
Needle Aspiration
![]() Anesthetize with benzocaine spray or have patient gargle viscous lidocaine
Anesthetize with benzocaine spray or have patient gargle viscous lidocaine
![]() Have patient depress own tongue by holding laryngoscope, insert as you would for intubation. Patient will be less likely to trigger own gag reflex while pulling down on blade (FIGURE 76.3)
Have patient depress own tongue by holding laryngoscope, insert as you would for intubation. Patient will be less likely to trigger own gag reflex while pulling down on blade (FIGURE 76.3)
![]() Anesthetize locally with 1 to 2 mL of 1% lidocaine via 27-gauge needle
Anesthetize locally with 1 to 2 mL of 1% lidocaine via 27-gauge needle
![]() Use a long spinal needle so visualization is not obscured by syringe
Use a long spinal needle so visualization is not obscured by syringe
![]() Cut the distal 1 cm off of the needle cover and recap the needle, thereby preventing the needle from penetrating >1 cm (FIGURE 76.4)
Cut the distal 1 cm off of the needle cover and recap the needle, thereby preventing the needle from penetrating >1 cm (FIGURE 76.4)
![]() Insert spinal needle at area of greatest fluctuance (usually the superior pole) and aspirate the pus
Insert spinal needle at area of greatest fluctuance (usually the superior pole) and aspirate the pus
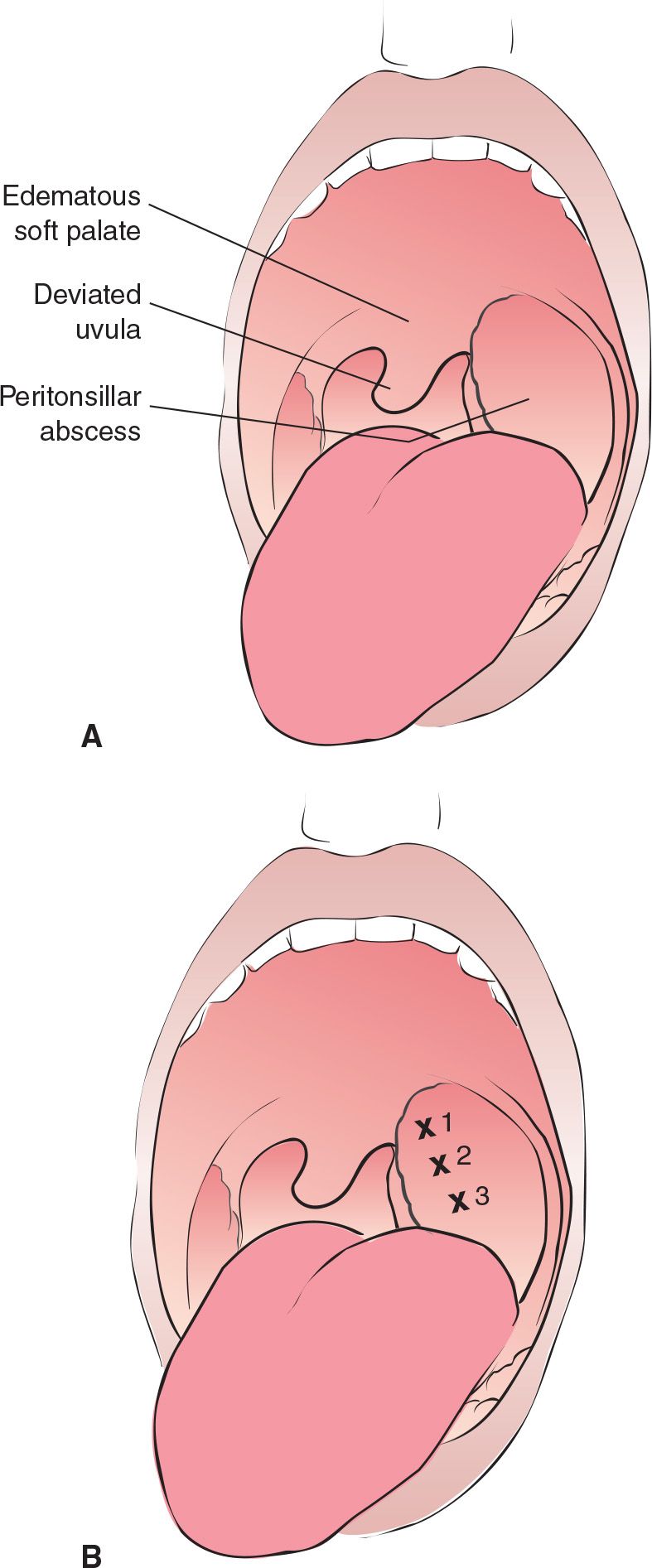
FIGURE 76.1 A: Peritonsillar abscess. The tonsil is displaced forward and inferomedial, the uvula is deviated toward the unaffected tonsil, and the soft palate is edematous and ruborous. B: Recommended sites for three-point needle aspiration of a peritonsillar abscess. (From Saladino RA. Pharyngeal procedures. In: Henretig FM, King C, eds. Textbook of Pediatric Emergency Procedures. Philadelphia, PA: Williams & Wilkins; 1997:692, 696, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


