Peripheral Vascular Injuries
Louis J. Magnotti
John P. Sharpe
Timothy C. Fabian
I. Introduction
To optimize outcomes following peripheral vascular injuries, prompt recognition is crucial. This mandates accurate diagnosis of those injuries requiring operation. Delays in either the recognition or subsequent treatment of these injuries can contribute to preventable limb loss.
Mandatory operative exploration is no longer required for all potential vascular injuries. Reliance on the physical examination findings of “hard” signs (Table 32-1) coupled with the selective use of arteriography has become the mainstay to guide operative and other therapy. After recognition, the best outcomes emanate from timely reperfusion and avoiding the factors associated with limb loss (Table 32-2).
II. Etiology
Vascular trauma is classified according to the general mechanism of injury (blunt or penetrating); different mechanisms typically produce different types of injuries and injury patterns. In urban trauma centers, peripheral vascular injuries are most commonly (75% to 80%) caused by penetrating trauma. Approximately 50% of these injuries are caused by handguns, 30% from stab wounds, and 5% from shotgun wounds. In the past, most gunshot wounds were small-caliber low-velocity bullets, although currently those are largely replaced by semiautomatic and automatic large-caliber weapons discharging higher-velocity missiles. The resulting vascular injuries are more devastating and are often associated with substantial associated soft-tissue and skeletal injuries. Peripheral vascular injuries from blunt trauma to the extremities including fractures, dislocations, crush injuries, and traction account for 5% to 25% of vascular injuries.
Penetrating injuries can result in complete transection and may present as thrombosis from vessel spasm or bleeding. In contrast, partially transected vessels may contract and continue to bleed. Even if controlled initially, the injured vessel may re-bleed as the patient is resuscitated and the arterial pressure rises. In the majority of cases, the location of a presumed vascular injury is estimated by following the path of the penetrating object.
The mechanism is critical to determine the risk of vascular injury and potential for amputation. Stab wounds are unlikely to lead to amputation. However, high-velocity injuries with associated blast effect and tissue loss are at an elevated risk of vascular injury and limb loss.
Blunt trauma usually results in an avulsion type injury where the artery is stretched. This stretching disrupts either the tunica intima alone or the tunica intima and tunica media together; the highly thrombogenic tunica externa is left to maintain vessel continuity. Significant intimal damage leads to thrombosis and eventually complete occlusion of the vessel. Those injuries that do not occlude can instead produce intimal flaps, pseudoaneurysms, or arteriovenous (AV) fistulas. While blunt trauma represents the minority of peripheral vascular injuries, delays in diagnosis and revascularization are more common, and generally result in a higher amputation rate than penetrating mechanisms. For blunt trauma, it is important to recognize that specific vascular injuries are commonly associated with distinct orthopedic injures (Table 32-3). Those skeletal injuries should prompt the clinician toward early recognition of vascular injury.
Table 32-1 Hard Signs of Arterial Injury | |
|---|---|
|
III. Arterial Injuries
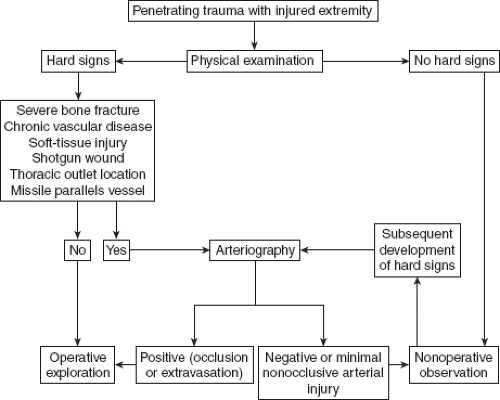
Diagnosis. Delays in diagnosis or therapy can be prevented through careful history and physical examination combined with the appropriate use of diagnostic modalities. The clinical manifestations of major peripheral vascular injuries (hard signs) must be recognized promptly and addressed early. A defined algorithm for management of penetrating vascular trauma should be utilized (Fig. 32-1).
History. Assessment of the injured extremity begins with a detailed history in conjunction with the physical examination. Pertinent information includes the estimation of blood loss at the scene (including pulsatile blood loss), time of injury, mechanism of injury, type of projectile, and the vital signs during the pre-hospital period. These details can provide important clues in identification of major vascular injury. Primary survey and stabilization of life-threatening injuries takes precedence over evaluation of the extremity; active hemorrhage from an injured extremity is addressed in the primary survey.
Physical examination. Detailed vascular, neurologic, soft-tissue, and skeletal examinations will determine the potential for vascular injury and the risk for limb loss.
A careful extremity evaluation provides information on the location and severity of the vascular injury.
Vascular examination. The presence of any hard signs (see Table 32-1) should prompt immediate search for a vascular injury.
All pulses proximal and distal to the area of potential injury should be palpated and documented. The injured extremity should be compared to the contralateral, uninjured extremity and any pulse differences noted.
For uncomplicated penetrating extremity trauma, the presence of any hard sign should trigger immediate surgical exploration. In general, evaluating such patients with further diagnostic modalities is unnecessary and delays definitive therapy; nearly all of these patients will have injuries requiring operative repair.
When a patient presents with hard signs of vascular injury in the face of multilevel trauma to the extremity, it can be difficult to determine the level of arterial injury. In this situation, arteriography is indicated,
preferably intra-operative angiography, to minimize delay in repairing the injury and facilitate intra-operative decision-making.
Table 32-2 Factors Associated with Higher Rates of Limb Loss in Vascular Trauma
Treatment delay—6 h
Blunt mechanism of injury
Lower extremity injuries, especially of the popliteal artery
Associated injuries: Nerve, vein, bone, soft-tissue loss
High-velocity gunshot wounds and close-range shotgun wounds
Preexisting chronic peripheral vascular disease and other comorbidities
Failure or delay in performing fasciotomy
Clinical presentation in shock or obvious limb ischemia
Table 32-3 Vascular Injuries Associated with Specific Orthopedic Injuries
Orthopedic injury
Associated vascular injury
Knee dislocation
Popliteal artery
Femur fracture
Superficial femoral artery
Supracondylar humerus fracture
Brachial artery
Clavicle fracture
Subclavian artery
Shoulder dislocation
Axillary artery
The absence of hard signs in an injured extremity virtually excludes the presence of a major vascular injury as reliably as arteriography or any other imaging modality.
Soft signs of vascular injury include a history of severe hemorrhage at the scene, unexplained hypotension, a stable, small hematoma that is not expanding or pulsatile, diminished or unequal pulses, a neurologic deficit, or a wound in proximity to vascular structures. Such findings may require diagnostic modalities beyond physical examination.
Neurologic evaluation. Motor and sensory examination of the affected extremity should be performed, documented, and compared to the uninjured extremity. It is important to remember that vascular injury may initially manifest sensory, “stocking or glove anesthesia,” and motor deficits secondary to
peripheral nerve ischemia. A nerve injury can only be diagnosed once vascular perfusion is restored or a nerve injury is directly visualized.
Non-invasive tests. These tests are not required for the evaluation of patients with hard signs of arterial injury. Such modalities can be helpful for the intra-operative or post-operative evaluation of vessel patency. They do not have advantages over physical examination in the initial diagnostic evaluation of injured extremities for vascular injury. Moreover, the information non-invasive tests yield in this setting can be misleading and falsely exclude a vascular injury on the basis of flow signals.
Ankle–brachial index (ABI). The ABI is obtained by placing a blood pressure cuff on the supine patient proximal to the ankle or wrist of the injured limb. The systolic blood pressure is determined with a Doppler probe at the respective posterior tibial and dorsalis pedis arteries or at the ulnar and radial arteries. The ratio of the highest systolic pressure obtained in the affected extremity to the systolic pressure in the unaffected extremity (most often the brachial artery) comprises the ABI. An ABI lower than 0.90 has a sensitivity and specificity of 87% and 97%, respectively for arterial injury. It is important to remember that there are certain clinical situations in which a vascular injury may not result in an abnormal ABI. For example, a non-axial injury, a lesion that does not disrupt arterial flow (intimal flap or transected artery with pseudoaneurysm), or an AV fistula may not lower the ABI and thus be missed.
Duplex imaging can aid intra-operative and post-operative evaluation of vessel patency. However, this modality is operator dependent and not routinely available.
Conventional contrast arteriography. Diagnostic angiography has a sensitivity of 95% to 100% and a specificity of 90% and 98%; it remains the diagnostic standard for evaluation or confirmation of arterial injury. With extremity trauma, non-selective angiography is not cost effective. It is often overly sensitive, detecting minimal injuries that do not require further management. Arteriography can be time consuming, delay definitive treatment, and lead to complications, including renal contrast toxicity and pseudoaneurysm formation.
There is little reason to perform angiography in a patient with hard signs of injury, unless an intra-operative angiogram is necessary to delineate anatomy. Operative intervention should never be delayed for arteriography in patients with hard vascular failure signs.
Also, unstable patients should not be sent from the trauma bay, operating room, or ICU for diagnostic arteriography. For these patients, arteriography may be performed in the primary setting, although the operating room is best when this constellation exists. The technique for lower extremity angiography is as follows:
Access the contralateral (unaffected) common femoral artery percutaneously with an 18 gauge arterial entry needle.
Insert a 5 french introducer sheath.
Pass a 260 cm 0.035 in guidewire through the introducer sheath.
Using fluoroscopy, pass an angiographic catheter, over the guidewire from the unaffected limb navigating the aortic bifurcation to the affected limb.
Hand inject full strength contrast while imaging (under fluoroscopy) defined segments of the affected limb. Then, observe for evidence and location of occlusion or gross extravasation of contrast.
Computed Tomographic Angiography (CTA). In recent years, CTA has shown levels of accuracy, resolution, and cost comparable to conventional arteriography. Rapid data acquisition facilitates the diagnostic work-up in critically injured patients who will require imaging for injuries to structures in which the vessel traverses, avoiding the delay for formal angiography. The three-dimensional reconstructions of CTA may be superior to conventional angiography. CTA represents a viable challenge to conventional angiography.
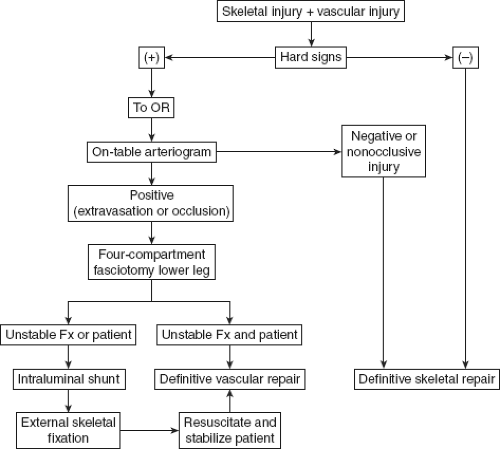
Blunt and complex vascular injury involves combined injuries to extremity vessels, bone, soft tissue, and nerves, and are associated with high amputation rates.
These injuries can result from blunt or destructive penetrating (shotgun and high-velocity firearm wounds) mechanisms. Application of a defined management algorithm for combined arterial and skeletal trauma is advantageous (Fig. 32-2).
Obtain as complete a history as possible from the pre-hospital providers (field blood loss, joint dislocation). Examine the extremity, being sure to document any change in the examination over time.
Delay in the treatment of complex extremity vascular injury represents the most common cause of limb loss, especially in the setting of the multiply injured trauma patient. Re-establishment of arterial flow should be the first priority after life-threatening injuries have been stabilized to maximize limb salvage. Skeletal, nerve, or soft-tissue trauma should be addressed only after revascularization has been accomplished.
Comminuted fractures or joint dislocation can temporarily obstruct arterial flow. A careful vascular examination should be performed before and after fracture reduction/realignment or splinting and relocation of dislocated joints with care to document pulses pre- and post-intervention.
The presence of hard signs mandates immediate vascular evaluation by arteriography, as many hard signs are due to findings from associated injuries in the setting of blunt trauma (high false positive rate of physical examination). Adhering to this practice helps avoid a high rate of negative limb exploration which may complicate associated injuries. To avoid potential delays in therapy, perform arteriography in the OR in conjunction with orthopedic management.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree