CHAPTER 22
Periorbital Ecchymosis
(Black Eye)
Presentation
The patient has suffered blunt trauma to the eye, most often resulting from a blow inflicted during a fistfight, a fall, a sports injury, or a car accident, and he is alarmed because of the swelling and discoloration. Family or friends may be more concerned than the patient about the appearance of the eye. There may be an associated subconjunctival hemorrhage, but the remainder of the eye examination should be normal, and there should be no palpable bony deformities, diplopia, or subcutaneous emphysema (Figure 22-1).
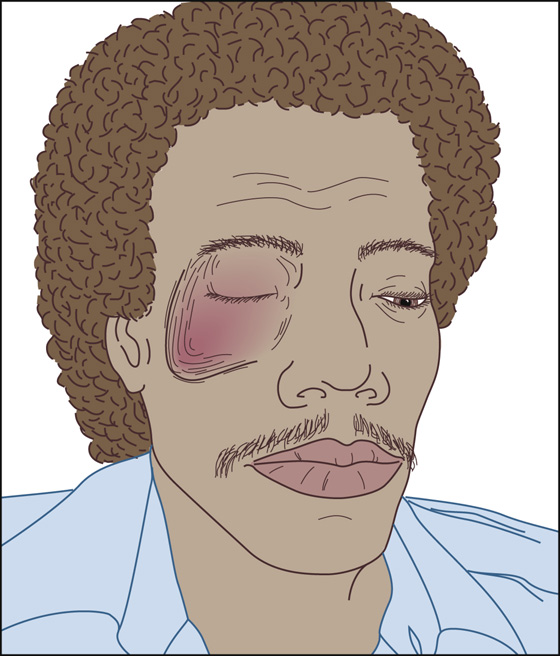
Figure 22-1 Blunt trauma to the eye.
What To Do:
 Determine, as well as possible, the specific mechanism of injury. A fist is much less likely than a line-drive baseball to cause serious injury.
Determine, as well as possible, the specific mechanism of injury. A fist is much less likely than a line-drive baseball to cause serious injury.
 Perform a complete eye examination, including a bright-light examination to rule out an early hyphema (blood in the anterior chamber) or an abnormal pupil; a funduscopic examination to rule out a retinal detachment, vitreous hemorrhage, or dislocated lens; and a fluorescein stain to rule out corneal abrasion. Best-corrected visual acuity testing should always be performed and, with an uncomplicated injury, is expected to be normal. All patients having contusions associated with visual loss, severe pain, proptosis, pupil irregularity, new visual “floaters,” loss of red reflex, or extensive subconjunctival hemorrhage should be referred to an ophthalmologist immediately.
Perform a complete eye examination, including a bright-light examination to rule out an early hyphema (blood in the anterior chamber) or an abnormal pupil; a funduscopic examination to rule out a retinal detachment, vitreous hemorrhage, or dislocated lens; and a fluorescein stain to rule out corneal abrasion. Best-corrected visual acuity testing should always be performed and, with an uncomplicated injury, is expected to be normal. All patients having contusions associated with visual loss, severe pain, proptosis, pupil irregularity, new visual “floaters,” loss of red reflex, or extensive subconjunctival hemorrhage should be referred to an ophthalmologist immediately.
 Special attention should be given to ruling out a blow-out fracture of the orbital floor or wall. Test extraocular eye movements, looking especially for restriction of eye movement or diplopia on upward gaze, and check sensation over the infraorbital nerve distribution. Paresthesia in the distribution of the infraorbital nerve suggests a fracture of the orbital floor. Enophthalmos usually is not observed, although it is part of the classic textbook triad associated with a blow-out fracture. Subcutaneous emphysema is a recognized complication of orbital wall fracture.
Special attention should be given to ruling out a blow-out fracture of the orbital floor or wall. Test extraocular eye movements, looking especially for restriction of eye movement or diplopia on upward gaze, and check sensation over the infraorbital nerve distribution. Paresthesia in the distribution of the infraorbital nerve suggests a fracture of the orbital floor. Enophthalmos usually is not observed, although it is part of the classic textbook triad associated with a blow-out fracture. Subcutaneous emphysema is a recognized complication of orbital wall fracture.

 Symmetrically palpate the supraorbital and infraorbital rims as well as the zygoma, feeling for the type of deformity that would be encountered with a displaced tripod fracture. A unilateral deformity will be obvious if your thumbs are fixed in a midline position while you use your index fingers to palpate the patient’s facial bones, both left and right, simultaneously (Figure 22-2).
Symmetrically palpate the supraorbital and infraorbital rims as well as the zygoma, feeling for the type of deformity that would be encountered with a displaced tripod fracture. A unilateral deformity will be obvious if your thumbs are fixed in a midline position while you use your index fingers to palpate the patient’s facial bones, both left and right, simultaneously (Figure 22-2).

Figure 22-2 Proper hand placement for symmetrically palpating the supraorbital and infraorbital rims.
 When there is a substantial mechanism of injury or if there is any clinical suspicion of an underlying fracture, obtain a CT scan of the orbit. CT scans are more sensitive than plain radiographs and allow visualization of subtle fractures of the orbit and small amounts of orbital air.
When there is a substantial mechanism of injury or if there is any clinical suspicion of an underlying fracture, obtain a CT scan of the orbit. CT scans are more sensitive than plain radiographs and allow visualization of subtle fractures of the orbit and small amounts of orbital air.
 If a significant injury is discovered, consult an ophthalmologist. For diplopia resulting from a blow-out fracture, immediate surgical intervention is not required, and follow-up may be delayed for 7 to 10 days, after the edema has subsided. However, a patient with a hyphema should see an ophthalmologist within 24 hours. The patient should be instructed to rest with his head elevated. A protective metal shield should be placed over the eye, and the patient should be instructed to refrain from taking aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs). Hospital admission is not required.
If a significant injury is discovered, consult an ophthalmologist. For diplopia resulting from a blow-out fracture, immediate surgical intervention is not required, and follow-up may be delayed for 7 to 10 days, after the edema has subsided. However, a patient with a hyphema should see an ophthalmologist within 24 hours. The patient should be instructed to rest with his head elevated. A protective metal shield should be placed over the eye, and the patient should be instructed to refrain from taking aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs). Hospital admission is not required.
 Consider the possibility of abuse; when suspected, obtain the appropriate consultations and make the appropriate referrals.
Consider the possibility of abuse; when suspected, obtain the appropriate consultations and make the appropriate referrals.
 When a significant injury has been ruled out, reassure the patient that the swelling will subside within 12 to 24 hours, with or without a cold pack, and that the discoloration will take 1 to 2 weeks to clear. Acetaminophen should be sufficient for analgesia.
When a significant injury has been ruled out, reassure the patient that the swelling will subside within 12 to 24 hours, with or without a cold pack, and that the discoloration will take 1 to 2 weeks to clear. Acetaminophen should be sufficient for analgesia.
 Instruct the patient to follow up with an ophthalmologist if there is any problem with vision or if pain develops after the first few days. Rarely, traumatic iritis, retinal tears, or vitreous hemorrhage may develop later, secondary to blunt injury.
Instruct the patient to follow up with an ophthalmologist if there is any problem with vision or if pain develops after the first few days. Rarely, traumatic iritis, retinal tears, or vitreous hemorrhage may develop later, secondary to blunt injury.
 With sports-related injuries, recommend protective eyewear made of polycarbonate. Polycarbonate lenses are available in prescription and nonprescription lenses in a sturdy sports frame.
With sports-related injuries, recommend protective eyewear made of polycarbonate. Polycarbonate lenses are available in prescription and nonprescription lenses in a sturdy sports frame.
What Not To Do:
 Do not order unnecessary radiographs. For minor injuries, if the eye examination is normal and there are no palpable deformities, radiographs and CT scans are unnecessary.
Do not order unnecessary radiographs. For minor injuries, if the eye examination is normal and there are no palpable deformities, radiographs and CT scans are unnecessary.
 Do not brush off bilateral deep periorbital ecchymoses (“raccoon eyes”), especially if caused by head trauma remote to the eye. This may be the only sign of a basilar skull fracture.
Do not brush off bilateral deep periorbital ecchymoses (“raccoon eyes”), especially if caused by head trauma remote to the eye. This may be the only sign of a basilar skull fracture.
Black eyes are usually nothing more than uncomplicated facial contusions. Patients become upset about them because they are so near to the eye, because they produce such noticeable facial disfigurement, and because the patient may seek retaliation against the person who hit him. Nonetheless, serious injury or abuse must always be considered and appropriately ruled out before the patient is discharged.
The extent of ocular damage depends on the size, hardness, and velocity of the blunt object causing the injury. A direct blow to the globe from a blunt object smaller than the eye’s orbital opening is more likely to cause injury to internal ocular structures (e.g., iris injury, ruptured globe, hyphema, retinal hemorrhage, retinal detachment, and vitreous hemorrhage). Injury by a blunt object larger than the orbital opening exerts force on the floor of the orbit or the medial wall, which is more likely to result in fractures of the thin bones (e.g., blow-out fracture).
Sudden orbital swelling or inflation immediately after nose blowing is caused by air being forced from a paranasal sinus (most often the maxillary) to the orbit through a fracture, which may act as a one-way valve, increasing the orbital pressure and potentially leading to a compressive optic neuropathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


