CHAPTER 21
Periorbital and Conjunctival Edema
Presentation
The patient is frightened by facial distortion and itching that appeared either spontaneously or up to 24 hours after being bitten by a bug or coming in contact with some irritant. One or both eyes may be involved. The patient may have been rubbing her eyes; however, an allergen or chemical irritant may cause periorbital edema long before a reaction, if any, is evident on the skin of the hand. There may be minimal to marked generalized conjunctival swelling (chemosis), giving the sensation of fullness under the eyelid, but there is little injection (Figure 21-1). In extreme cases, this chemosis may appear as a large, watery bubble (“watch-glass chemosis”), which may be frightening to the patient but is actually quite harmless. Tenderness and pain should be minimal or absent, but pruritus may at times be intense. There should be little or no erythema of the skin and no photophobia or fever. Visual acuity should be normal, there should be no fluorescein uptake over the cornea, and the anterior chamber should be clear.
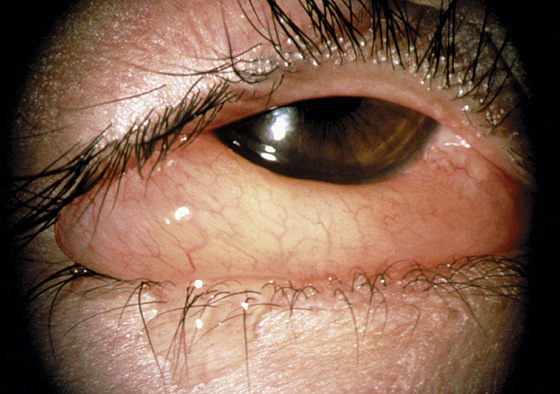
Figure 21-1 Spontaneous swelling and itching are common symptoms of periorbital and conjunctival edema. This represents an allergic conjunctivitis with chemosis secondary to an airborne allergen. (Adapted from Palay DH, Krachmer JH: Primary Care Ophthalmology, ed 2. St Louis, 2005, Mosby.)
What To Do:
 Inquire about possible causes, including allergies and chemical irritants. Pollen, animal dander, neomycin-containing eye drops, insect protein (a gnat flying into the eye), cosmetics, hair sprays, and contact lens solutions, as well as the usual causes of contact dermatitis, are sources for these reactions (see Chapter 160).
Inquire about possible causes, including allergies and chemical irritants. Pollen, animal dander, neomycin-containing eye drops, insect protein (a gnat flying into the eye), cosmetics, hair sprays, and contact lens solutions, as well as the usual causes of contact dermatitis, are sources for these reactions (see Chapter 160).
 After completing a full eye examination, reassure the patient that this condition is not as serious as it looks.
After completing a full eye examination, reassure the patient that this condition is not as serious as it looks.
 Prescribe hydroxyzine (Atarax), 25 to 50 mg q6h, for mild to moderate periorbital swelling and a 3- to 5-day course of steroids (prednisone, 20 to 40 mg qd) for more severe cases.
Prescribe hydroxyzine (Atarax), 25 to 50 mg q6h, for mild to moderate periorbital swelling and a 3- to 5-day course of steroids (prednisone, 20 to 40 mg qd) for more severe cases.
 Ophthalmic drops are soothing and reduce swelling when the conjunctiva is involved. Prescribe olopatadine 0.1% (Patanol), ketotifen fumarate 0.025% (Zaditor) [now over the counter], or azelastine hydrochloride 0.05% (Optivar), 1 drop bid. These are H1 antihistamines and mast-cell stabilizers and should be prescribed for 1 week, then prn thereafter.
Ophthalmic drops are soothing and reduce swelling when the conjunctiva is involved. Prescribe olopatadine 0.1% (Patanol), ketotifen fumarate 0.025% (Zaditor) [now over the counter], or azelastine hydrochloride 0.05% (Optivar), 1 drop bid. These are H1 antihistamines and mast-cell stabilizers and should be prescribed for 1 week, then prn thereafter.
 A short course of a topical steroid agent (loteprednol 0.02% [Alrex] or 0.05% [Lotemax], 1 drop qid) should be reserved for the more severe cases. This may be used for up to 1 week.
A short course of a topical steroid agent (loteprednol 0.02% [Alrex] or 0.05% [Lotemax], 1 drop qid) should be reserved for the more severe cases. This may be used for up to 1 week.
 Instruct the patient to apply cool compresses to reduce swelling and discomfort.
Instruct the patient to apply cool compresses to reduce swelling and discomfort.
 Warn the patient about the potential signs of infection.
Warn the patient about the potential signs of infection.
What Not To Do:
 Do not apply heat; heat causes an increase in swelling and pruritus.
Do not apply heat; heat causes an increase in swelling and pruritus.
 Do not confuse this condition with orbital or periorbital cellulitis, which are serious infections manifested by pain, heat, and fever. Orbital cellulitis is more posterior, involves the ocular muscles (which causes painful extraocular movements), and calls for IV antibiotic therapy and hospital admission.
Do not confuse this condition with orbital or periorbital cellulitis, which are serious infections manifested by pain, heat, and fever. Orbital cellulitis is more posterior, involves the ocular muscles (which causes painful extraocular movements), and calls for IV antibiotic therapy and hospital admission.
Discussion
The dramatic swelling that often brings a patient to the ED or the family doctor occurs because there is loose connective tissue surrounding the orbit. Fluid quickly accumulates when a local allergic response leads to release of histamine from mast cells, which causes increased capillary permeability, resulting in dramatic eyelid and periorbital swelling. The insect envenomation, allergen, or irritant responsible may actually be located some distance away from the affected eye, on the scalp or face, but the loose periorbital tissue is the first to swell. If the swelling is due to contact dermatitis (e.g., poison ivy) and the allergen is bound to the skin, oral steroids should be continued for 10 to 14 days, until the skin renews itself (see Chapters 160 and 182).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



