CHAPTER 30
Percutaneous Facet Fusion
BACKGROUND
As surgical technology becomes less invasive, interventional pain physicians will play an increasing role in delivering this care. Facet mediated pain has historically been treated with medial branch blocks, intra-articular injections, and radiofrequency neurolysis. There has been an increased interest in treating facet mediated pain from a surgical standpoint. Since facet joints are synovial diarthrodial joints, surgical approaches have focused on joint immobilization or arthrodesis. One minimally invasive approach is percutaneous facet fusion (PFF) with allograft bone dowels.
INTRODUCTION
PFF has emerged as a standalone and augmentative procedure to help patients with facet mediated pain. The procedure addresses facet mediated pain due to degenerative facet arthrosis, mechanical loading, and minor instability.
The advantages of PFF are:
• Reduced invasiveness and morbidity
• Early recovery and discharge
• Motion preservation
PFF fits well within the continuum of spinal care, with a position between interventional (percutaneous) and reconstructive (surgical) spinal procedure.
PFF doesn’t “burn bridges.”
• The current patients will still have access to future advances in spinal surgery, eg, biologics.
• Technical feasibility, safety, and biomechanical stability have been demonstrated.
• Percutaneous facet fixation with screws and intra-articular facet joint spacers have demonstrated efficacy.
• Finally, less invasive fusions have comparable outcomes to more invasive fusions and patient selection continues to be subjective.
POTENTIAL INDICATIONS
• Isolated facet–based symptomatic back pain that is refractory to conservative measures
• Stabilization of the lumbar spine following decompressive procedures or where minor instability exists or presents postoperatively
• Minor instability (1-2 mm listhesis)
• Posterior supplemental fixation to interbody fusion
• Adjunct to motion limiting devices
CONTRAINDICATIONS (RELATIVE OR ABSOLUTE) AND INDICATIONS FOR PROCEDURE TERMINATION
• Trauma
• High-grade instability
• Tumors
• Spondylolysis (pars fracture)
• Grade 2 or greater spondylolisthesis
• Infection, systemic or localized
• Coagulopathy
• Distorted or complicated anatomy
• Progressive neurologic deficit
• Allergy to procedural drugs, eg, iodinated contrast
• Open wound or skin ulceration
• Poorly controlled diabetes
• Patient refusal or lack of health care proxy
• Inability to prone for the duration of the procedure
• Intraoperative recognition of foraminal trespass or epidural placement
• Severe nerve root pain during procedure
• Hypotension
RELEVANT ANATOMY
• The lumbar facet joint is a diarthrodial, synovial joint. These joints can undergo a process of degeneration leading to arthropathy.
• The facet joint represents an articulation between the inferior articular process of the cephalad vertebral body and the superior articular process of the caudal vertebral body.
• The inferior articular process is convex and the superior articular process is concave.
• The joint is oriented obliquely to the sagittal plane.
• The articular surfaces are lined with hyaline cartilage.
• The joint contains a synovial membrane and synovial fluid. The joint is encapsulated with a synovial sheath. This creates a superior articular recess that is anterior and an inferior articular recess that is posterior.
• Forward flexion opens up the inferior recess and the joint; whereas extension opens the superior recess.
• The joint receives a rich sensory innervation by the ipsilateral medial branches, at that level and the cephalad level.
• As the disc degeneration progresses, the facet joint may become lax and facilitate the degenerative cascade.
• Facet arthropathy or sclerosis can be diagnosed and rated, in terms of severity, via MRI and CT scanning. CT or MR imaging provides information about facet orientation and this helps with procedure planning.
• There is a well-established discordance between facet arthropathy and facet mediated pain; hence, the interventional pain community relies on comparative diagnostic blocks to diagnose facet mediated pain. This step may be essential as a prelude to neurolysis, but is not de rigueur for PFF.
• The surgical literature relies on imaging evidence of facet arthropathy and the presence of pain, when planning facet fusion procedures.
What is PFF?
• Percutaneous facet fusion involves the insertion of cortical bone allograft in the shape of a dowel to achieve arthrodesis.
• These dowels are FDA approved as a bone graft to provide stability for primary and secondary healing of bone.
• The dowels have different proprietary designs ranging from cylindrical, tapered, threaded, or rectangular with wings/flanges.
• Different shapes exist to facilitate intra-articular placement and to mitigate “back out” or dislodgement.
• The dowels separate joint surfaces and eventually, stabilize the joint. Surgical access is similar among different manufacturers.
PREOPERATIVE CONSIDERATIONS
• Patients should have constant pain >6/10 and functional limitations.
• Patients should have withheld coagulopathic medications for appropriate lengths of time as per ASRA recommendations.
• Diabetic patients may need blood sugar testing.
• Female patients of childbearing age should have urine pregnancy test or a serum pregnancy test.
• Intravenous access is advised, particularly for patients receiving cervical or thoracic procedures, and for patients who may need intravenous anxiolytics and/or analgesics.
• Cardiopulmonary safe guards and resuscitation equipment should be present within the procedure suite.
• Patients should sign witnessed informed consent, which includes an evidence-based discussion about indications, efficacy, and safety.
• Preprocedure site marking/initialing with an indelible marker site and site verification.
Positioning of the Patient
• Prone
• Pressure points should be padded
• Eye protection may be necessary
• Neck position should be neutral
• Reduce lumbar lordosis
Needles, Medications, and Equipment
• Scalpel, #11 or #15
• 22-gauge spinal needle, 6 in
• Steinman or guide pin ×2
• Cannulated facet distractor (spatula) or directional cannula with prongs ×2
• Drill guide
• Drill bit with electrically powered drill
• Bone dowel delivery device and bone dowels ×2
• Impaction pin ×2
INTRAOPERATIVE TECHNICAL STEPS
• Sterile patient preparation.
• Antibiotic prophylaxis.
• Fluoroscopy to visualize lucency of facet joint.
![]() Oblique angulation (30-50 degrees)—to visualize facet joint lucency.
Oblique angulation (30-50 degrees)—to visualize facet joint lucency.
![]() Angle of approach can be estimated via axial CT or MRI images.
Angle of approach can be estimated via axial CT or MRI images.
![]() Tip: facet joint may be curvilinear in shape—so obliquity of C-arm should accommodate dorsal limb of facet joint.
Tip: facet joint may be curvilinear in shape—so obliquity of C-arm should accommodate dorsal limb of facet joint.
• Under fluoroscopy, advance 22-gauge spinal needle is placed into facet joint.
• Make a stab incision with scalpel, adjacent to needle entry site.
• Advance guide (Steinman) pin into plane of facet joint (Figure 30-1).
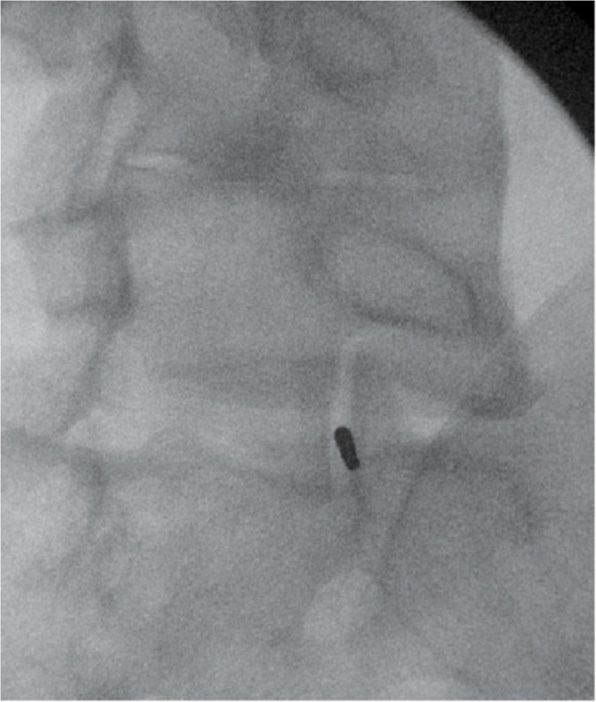
Figure 30-1. Steinman pin placement, right L5-S1 facet joint.
![]() Tip: use needle path to guide trajectory.
Tip: use needle path to guide trajectory.
• Once guide pin contacts dorsal surface of facet joint, advance 5 mm.
![]() Tip: the curvature of facet joint should reduce risk of foraminal trespass, but this is not applicable to patients with osteoporosis.
Tip: the curvature of facet joint should reduce risk of foraminal trespass, but this is not applicable to patients with osteoporosis.
• Advance cannulated facet distractor (Figure 30-2) over guide pin.
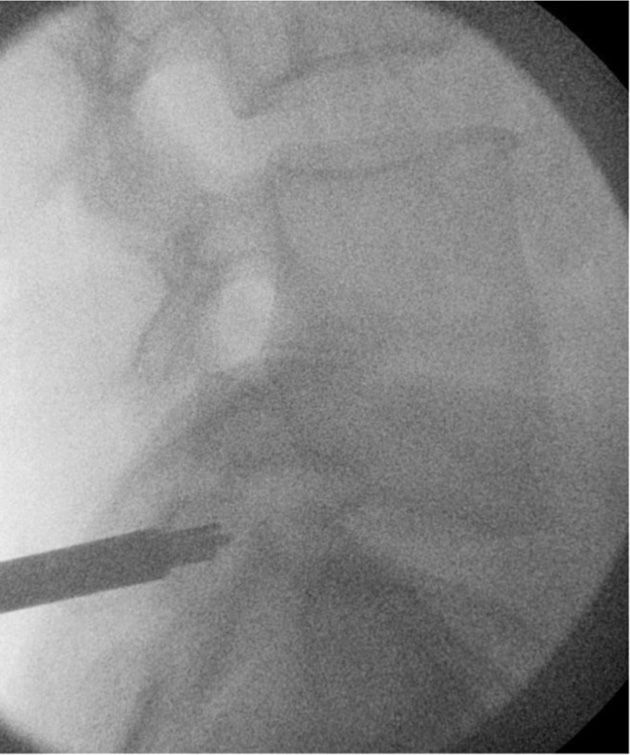
Figure 30-2. Cannulated facet distractor, right L5-S1 facet joint.
![]() Tip: anchor guide pin and facet distractor when it enters skin, do not move this aggressively, else it may dislodge out of facet joint.
Tip: anchor guide pin and facet distractor when it enters skin, do not move this aggressively, else it may dislodge out of facet joint.
• Tap facet distractor (spatula) (Figure 30-2) slightly into facet joint with mallet.
![]() Tapered tip facet distractor should stop at 5 mm depth.
Tapered tip facet distractor should stop at 5 mm depth.
![]() Tip: carefully monitor guide pin depth to avoid foraminal trespass.
Tip: carefully monitor guide pin depth to avoid foraminal trespass.
• Directional cannula should be threaded over facet distractor.
• Place tip of directional cannula (2 prongs) into plane of facet joint.
• Tap the directional cannula to fully seat the device.
• Hold directional cannula and slowly remove the facet distractor and guide pin.
• Advance drill guide into directional cannula.
• Advance drill bit into cannula/drill guide.
• Use drill to core out hole in facet joint.
![]() Tip: Trufuse uses a 1 step drill guide.
Tip: Trufuse uses a 1 step drill guide.
• Drill cores out superior and inferior facet joints simultaneously.
![]() Tip: Verteloc uses a 2-step drill guide.
Tip: Verteloc uses a 2-step drill guide.
• Drill cores out superior facet (lateral articulating surface).
• Rotate the drill guide 180 degrees.
• Reinsert drill and core out the inferior facet (medial articulating surface).
• The drill guide has a built in stop.
![]() Tip: saline irrigation reduces risk of thermal injury.
Tip: saline irrigation reduces risk of thermal injury.
![]() Tip: use lateral fluoroscopy to ensure no violation of foramen.
Tip: use lateral fluoroscopy to ensure no violation of foramen.
• Remove drill.
• Load implant holder with bone dowel or preformed dowel.
• Implant/dowel is a cortical allograft.
![]() Tip: verify with device manufacturer about safety and reliability of cortical allograft.
Tip: verify with device manufacturer about safety and reliability of cortical allograft.
![]() Tip: implant holder has different configurations depending on shape of bone dowel.
Tip: implant holder has different configurations depending on shape of bone dowel.
• Verteloc: rectangular dowel with “fins”—fins are parallel to joint and body is perpendicular.
• Trufuse: cylindrical bone dowel (Figures 30-3 and 30-4).

Figure 30-3. Bone dowel, left L5-S1 facet joint.

Figure 30-4. Bone dowel, right L5-S1 facet joint.
• Nufix: threaded bone dowel.
• Advance implant holder with implant into facet joint.
• Tamp dowel into place.
• Remove instruments.
• Suture skin with 2-0 and 3-0 nylon.
• Patient bracing with a lumbosacral orthosis, for 6 to 12 weeks.
MONITORING OF POTENTIAL POSTPROCEDURE COMPLICATIONS
• Assess for bleeding at skin entry site.
• Use lateral fluoroscopy to monitor for foraminal trespass.
• Use anteroposterior fluoroscopy to gauge anteromedial dowel placement.
• Postoperative neurologic assessment
![]() If patient sedated, test withdrawal response on plantar surface of foot
If patient sedated, test withdrawal response on plantar surface of foot
![]() Assess sensorimotor and reflex integrity
Assess sensorimotor and reflex integrity
![]() Voiding and ambulation status on discharge
Voiding and ambulation status on discharge
![]() CT scan in selected patients (Figures 30-5 through 30-7)
CT scan in selected patients (Figures 30-5 through 30-7)

Figure 30-5. Axial CT scan; seated dowels at L5-S1.
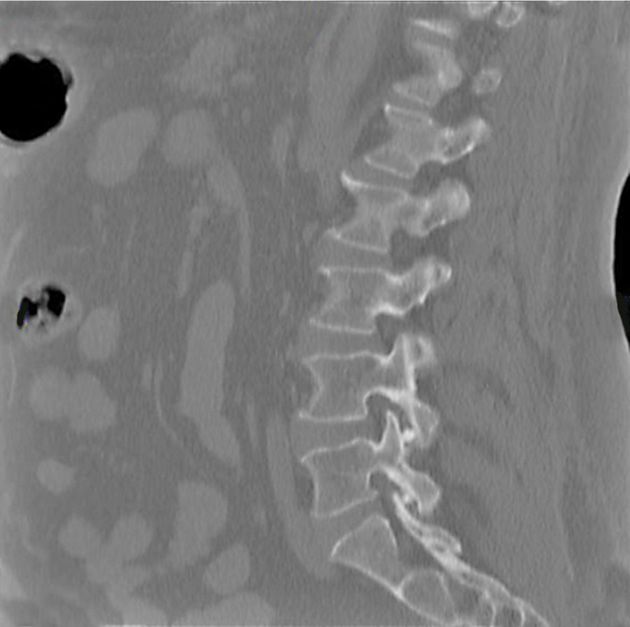
Figure 30-6. Sagittal CT scan: seated dowels at L4-5 and L5-S1.
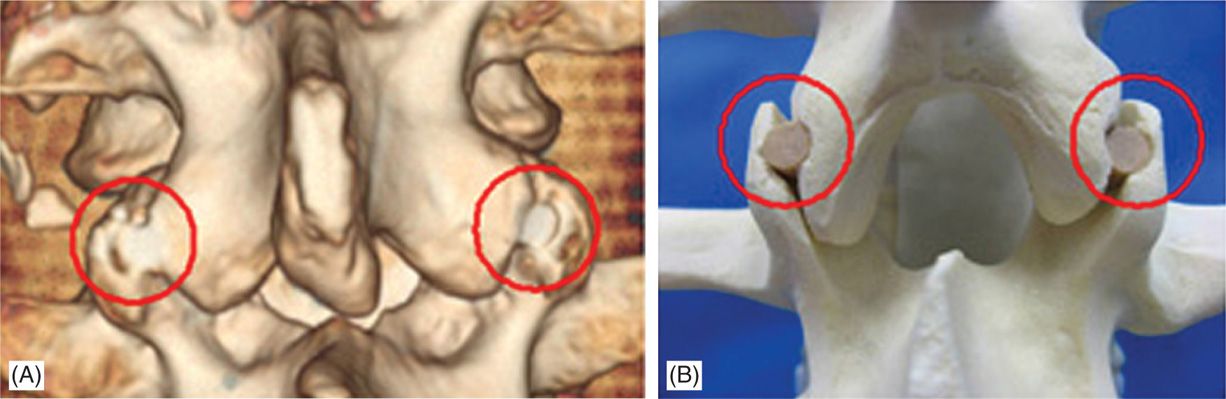
Figure 30-7. (A) 3D CT Scan of TruFUSE, (B) TruFUSE® Implanted in a sawbone. (Reproduced with permission from Contempo Medical, LLC.)
OUTCOMES
In an abstract presentation, Trangco-Evans demonstrated that 3 out of 8 patients did well and that 5 patients did improve. The latter 5 patients had evidence of dowel back out and poor compliance with postoperative brace utilization. Advances in dowel configuration and improving patient compliance with brace utilization are reasonable goals to improve efficacy.
Patient safety should be monitored in the early postoperative period. Physician vigilance over infection, pain, bleeding, dowel back out, brace compliance, nerve protection, and fall prevention are important.
ACRONYMS
CLBP chronic or nonspecific low back pain
CT computed tomography scan
MRI magnetic resonance imaging
PFF percutaneous facet fusion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






