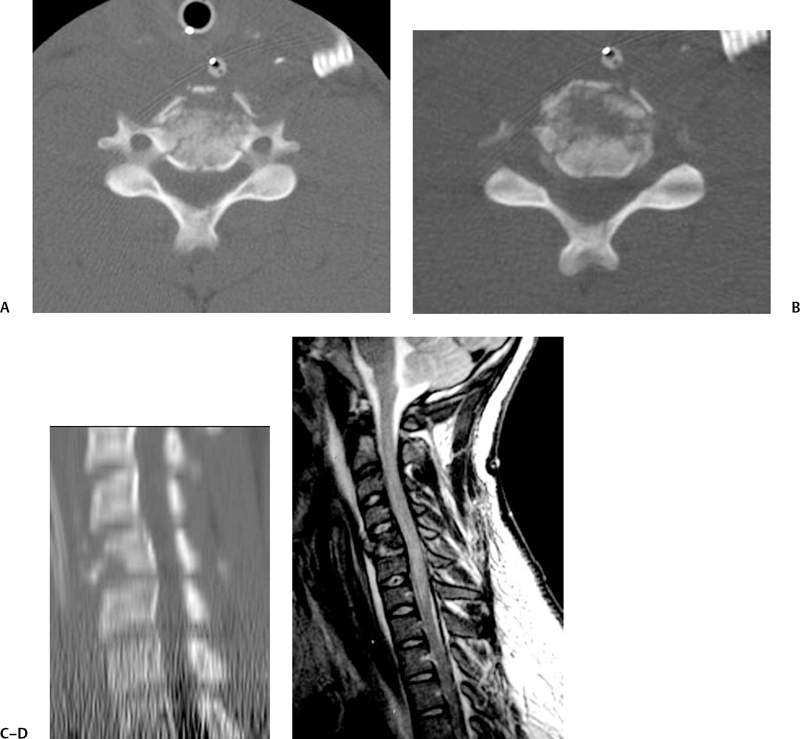
13 Pediatric Spinal Injuries William S. Anderson and George I. Jallo Understanding the differences in pediatric versus adult spinal trauma can begin with the development and growth of the spine in general (Table 13.1). The healthy development of the spine is governed by the proper segmentation and specialization of the different spinal elements under genetic control.1,2 Of interest in the cervical spine is the complexity of formation of the C1 and C2 elements. Most cases of os odontoideum are clearly linked with traumatic events (Fig. 13.1), but there are also well-described twin studies of patients with similar upper cervical defects resulting in congenital dens malformations.3 It has been hypothesized that a congenital weakness at the synchondrosis might also predispose certain patients to os formation caused by mild trauma.3 The axis itself is formed from four separate ossification centers: one for the dens, one for the body, and two for the posterior arch.4 The atlas is complex as well and forms from three ossification centers: one single center in the anterior body, and two paired centers forming the posterior ring. An unfused posterior ring between the two latter centers is frequently encountered during dissection around C1.4 The atlanto-dens interval is larger in children than in adults and can be as high as 4.5 mm on a normal radiograph.5 Fig. 13.1 Plain x-ray views of a young patient with os odontoideum. (A) Neutral view of the os odontoideum. (B) Flexion view of patient demonstrating the dens. (C) Extension view of the same patient. One particular development anomaly affecting the cervical spine and occipitocervical junction is the Klippel-Feil syndrome,6 which illustrates many features of incomplete spinal segmentation. There are three major subtypes of the malformation per the classification scheme of Nagib et al:6 type I involves multilevel cervical and thoracic vertebral fusion; type II affects patients with one or two interspace fusions, hemivertebrae, and occipitoatlantal fusion; and type III consists of patients with cervical and lower thoracic or lumbar level fusions. Several authors have identified specific fusion patterns that result in unstable cervical spine configurations, including a fused C2-C3 level with occipitalization of the axis, multilevel cervical fusion with a malformed occipitocervical level, and an unfused space between two long fused segments.7,8 Normal findings in the subaxial spine in children include pseudosubluxation of C2 on C3 by up to 3 mm,9 as well as in general more wedge-shaped vertebral bodies during ossification. An additional factor affecting spinal injury patterns in children is the orientation of the cervical facet joints, especially in the young child.10 The upper cervical spine facet joints start at a fairly horizontal angle of 30 degrees relative to the sagittal plane at birth, which increases to 60 to 70 degrees by the teenage years.10 Intersegmental stability is also not mature until after the ossification of the uncinate processes, which occurs after 7 years of age.10,11 Additionally, in the young child, the upper cervical spine segments drain via the lymphatic system into the deep cervical and nasopharyngeal lymph node chains, the same drainage as the nasopharynx itself, which can lead to Grisel syndrome and C1-C2 rotatory subluxation.12 It is conceivable that this form of instability can occur after surgical procedures performed in the pharynx as well.13 During the growth period between infancy and adolescence, the thoracic spine changes morphology enormously (Table 13.2). In a large longitudinal study of thoracic spine curvature following healthy children, the thoracic kyphosis increased by 6 degrees between the ages of 5–6 and 15–16 years. In the same time period, lumbar lordosis increased by 6 degrees.14 The thoracic spine mobility decreases a great deal during this time period, by as much as 27 degrees.14 The increase in magnitude of the thoracic kyphosis during growth is not linear, but seems to take off very quickly between the ages of 13 and 15.15 Just prior to this age range, during the time of the adolescent growth spurt, the amount of kyphosis actually decreases somewhat, with the anterior vertebral growth exceeding the posterior growth during the 10- to 12-year age range.15,16 There are also slightly different timings of these kyphotic changes as a function of sex. Table 13.2 Thoracic Spine Development
 Pediatric Spine Development and Anatomy
Pediatric Spine Development and Anatomy
Cervical Spine Development

Thoracic Spine Development
| Morphology | Changes drastically between infancy and adolescence: |
| • Thoracic kyphosis increases 6 degrees between 5-6 and 15-16 years of age | |
| • Lumbar kyphosis increases 6 degrees | |
| Mobility | Decreases by as much as 27 degrees during this period |
| Kyphotic changes | • Not linear; most change between ages 13 and 15 |
| • Actually decrease between ages 10 and 12 | |
| • Slight difference in timing of these changes between sexes |
Lumbar Spine Development
Similarly, developmental disorders of the lumbar spine can predispose the pediatric population to further risk from trauma (Table 13.3). Spondylolysis and slippage are not uncommon in the pediatric population and seem to be more prevalent during the growth spurt.17,18 The slippage itself, which occurs in association with spondylolysis, appears to be a problem of epiphyseal separation or epiphyseal plate injury due to the defect in the isthmus19,20 (Fig. 13.2). The growth plate of the vertebral body is exposed to enormous stresses due to the bilateral pars defects and can frequently shear apart, leading to the listhesis. This does not appear to be a degeneration of the disk itself.19
Additionally, there is a spectrum of caudal agenesis disorders that can affect growth of the sacral vertebral segments, as well as neural structures, and the spinal dysraphism disorders affecting the posterior bony elements.21 In severe cases of caudal agenesis, spinopelvic instability can be an issue requiring operative intervention, and frequently these children have scoliosis problems as well.21 Although not necessarily predisposing these children to additional traumatic injury, they are commonly enough encountered to complicate the surgical treatment of trauma in this group.

Fig. 13.2 A 13-year-old athletic boy with low back pain without radiation. The cone-down lateral x-ray clearly demonstrates the defect in the pars of the L4 vertebrae.
Table 13.3 Lumbar Spine Development
| Spondylolysis and slippage | • Most prevalent during growth spurt |
| • Slippage: problem of epiphyseal separation or epiphyseal injury due to isthmus defect | |
| • Listhesis: may occur due to shearing effects of bilateral pars defects on growth plate of vertebral bodies | |
| Caudal agenesis disorders | • Affects growth of sacrum and neural structures |
| • Spinal dysraphism affecting posterior bony elements | |
| • Spinopelvic instability requires operative treatment |
 Pediatric Spinal Injury Characteristics
Pediatric Spinal Injury Characteristics
Overview
In general, cervical spine injury patterns in children (Table 13.4) are different from those in adults because of the pediatric disproportionate head size, looser cervical spinal biomechanics, and immaturity of bone formation.22,23 Anthropometric growth data for children demonstrate vastly different growth rates for head circumference versus the more linearly related growth of other body structures, with this growth rate difference persisting to an age of 6 to 7 years.24 Children do seem to be safer than adults in falls from great heights (>15 feet); they survive in higher percentages, and have fewer internal organ injuries and fewer spinal fractures.25 Younger children who do sustain spine trauma tend to exhibit cord injury more frequently than older children and die more frequently,26,27 although as a group, the younger patients (<11 years) present less frequently.27 In one large series from the Mayo Clinic, the age- and sex-adjusted annual incidence rate for trauma-induced fracture and dislocation of the cervical spine was 7.41 per 100,000 population.27
Characteristic Injury Patterns in the Cervical Spine
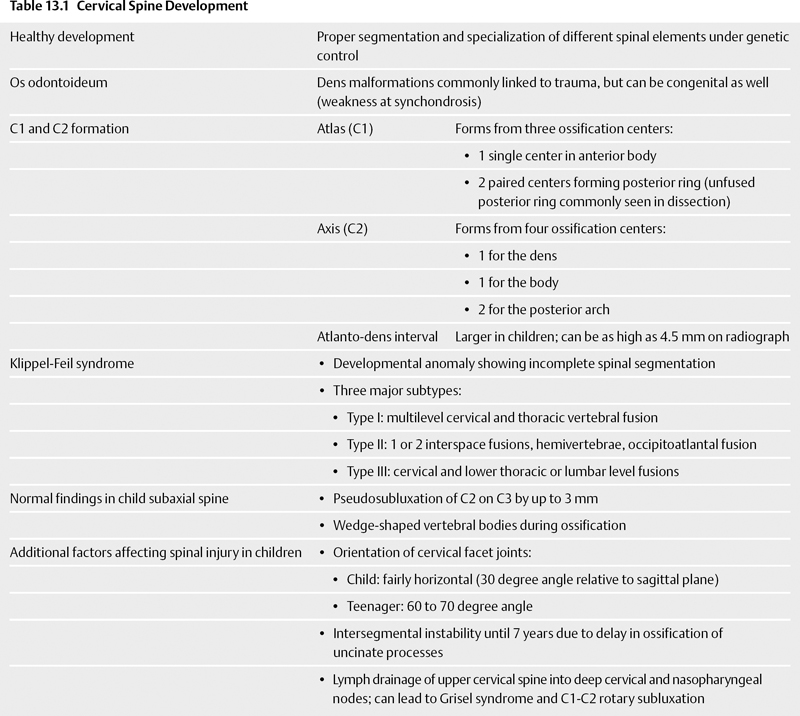
Pediatric cervical spine injuries frequently occur in association with motor vehicle accidents (60% in the Rancho Los Amigos series).28 Of interest, if the injured victim was a pedestrian, the victim’s age was most likely less than 11 years old. Another age division occurs in sports-derived cervical spine injuries, with most patients ranging from 12 to 16 years of age.28 Because of the large pediatric head size, the levels of greatest movement in the cervical spine are different from those in an adult (Table 13.5). In infants, it occurs at C2-C3, at 5 to 6 years it moves downward to C3-C4, and in adolescents and young adults it occurs at the C5-C6 level, as in maturity.29 This categorization also correlates with the predominant level of injury in the pediatric population. These patients are subject to the gross patterns of injury demonstrated in the adult population as well, including atlantoaxial subluxation via transverse ligament disruption, Jefferson-type fractures, hangman’s fractures, odontoid fractures, and atlantoaxial rotatory subluxation, as well as subaxial spine fractures (Fig. 13.3).4 Additionally, the phenomenon of spinal cord injury without radiographic abnormality (SCIWORA) is present in perhaps 10 to 20% of spine-injured children and may represent various forms of ischemic injury or cartilaginous failure.4,30
The criteria of Panjabi and White need to be relaxed somewhat when evaluating the pediatric spine due to the higher mobility and elasticity in the pediatric population.29,31 One set of criteria marking instability under the age of 8 years includes more than 4.5 mm of subluxation at the C2-C3 or C3-C4 levels, and more than 3.5 mm of subluxation at any level for patients older than 8 years. Furthermore, angulation of a deformity greater than 7 degrees can also be a sign of ligamentous injury.29 The younger population frequently suffers from traumainduced rotatory atlantoaxial subluxation as well (Fig. 13.4), and very rarely may have a pure component of strict atlantoaxial subluxation after tearing the transverse ligament.32 In children, this is much more likely due to Grisel inflammatory syndrome or from congenital problems. Other causes of atlantoaxial stability leading to problems after trauma include Down syndrome, juvenile rheumatoid arthritis, and the skeletal dysplasias.4 Birth injury as a cause of cervical spine fracture-dislocation is rare but does occur and needs to be included in the differential diagnosis of neonatal hypotonia. Many of these cases involve cervical hyperextension of the neck with the child in breech position.33
Table 13.4 Pediatric Cervical Spine Injury
| Patterns of injury differ compared with adults due to | • Disproportionate head size |
| • Loose cervical spine biomechanics | |
| • Immature bone formation | |
| Falls from heights >15 feet | Children actually safer than adults: |
| • Higher survival percentage | |
| • Fewer internal organ injuries | |
| • Fewer fractures | |
| Mayo Clinic study27 | Age- and sex-adjusted incidence of cervical spine fracture and dislocation due to trauma = 7.41 per 100,000 |
Table 13.5 Imaging Patterns in Pediatric Cervical Spine
| Associations | Motor vehicle accidents, sports injuries (12-16 years) |
| Levels of greatest movement | Correlate with predominant level of injury in pediatric population: |
| • Infants: C2-C3 | |
| • 5 to 6 years: C3-C4 | |
| • Adolescent/young adult: C5-C6 | |
| Gross injury patterns | • Atlantoaxial subluxation via transverse ligament disruption |
| • Jefferson-type fractures | |
| • Hangman’s fractures | |
| • Odontoid fractures | |
| • Atlantoaxial rotatory subluxation | |
| • Subaxial spine fractures | |
| SCIWORA | Spinal cord injury without radiographic abnormality: |
| • Present in 10 to 20% | |
| • May represent ischemic injury or cartilaginous failure | |
| Cervical spine instability | • Criteria: |
| • >4.5 mm subluxation at C2-C3 or C3-C4 under age of 8 | |
| • >3.5 mm subluxation at any level over age 8 | |
| • Angulation of deformity >7 degrees: sign of ligamentous injury | |
| • Trauma-induced rotatory atlantoaxial subluxation common | |
| • Strict atlantoaxial subluxation following transverse ligament tear is rare; more likely due to Grisel syndrome or congenital | |
| • Other causes of atlantoaxial instability: Down syndrome, juvenile rheumatoid arthritis, skeletal dysplasias | |
| • Birth injury rare but needs consideration, especially in diagnosis of neonatal hypotonia |
Characteristic Injury Patterns of the Thoracolumbar Spine
Thoracolumbar fractures (Table 13.6) in the pediatric population in the United States are most frequently caused by motor vehicle accidents, followed by falls, and pedestrian versus vehicle accidents.34 Simple physical exam of these patients has a relatively high sensitivity (87%) for diagnosing a fracture and can be used as a filter before imaging.34 Physical exam findings correlated with injury include midline spinal tenderness and ecchymosis.
The most common type of thoracic and thoracolumbar fracture in children is the compression fracture, and these fractures frequently are multiple.35 Fortunately, because of continued bone growth, these types of fractures are remodeled quickly, and persistent kyphotic deformities are unusual in children after compression fractures.35 Besides thoracic compression fractures occurring after motor vehicle accidents or falls, this age range also exhibits Chance-type multicolumnar fractures (Fig. 13.5), more often in the upper lumbar region. They have been reported in both restrained and unrestrained passengers.26 Burst-type fractures are more common in older children.26