13 Pediatric Resuscitation
• Correct positioning is imperative for successful management of the anterior and cephalad pediatric airway.
• Outside the newborn period, use of a cuffed endotracheal tube in a child is acceptable.
• Children in full cardiorespiratory arrest who have an advanced airway should not receive more than 8 to 10 breaths per minute during resuscitation.
• “Push hard, push fast” with minimal interruptions between compressions is the recommendation for cardiopulmonary resuscitation.
Basic Principles of Cardiopulmonary Resuscitation
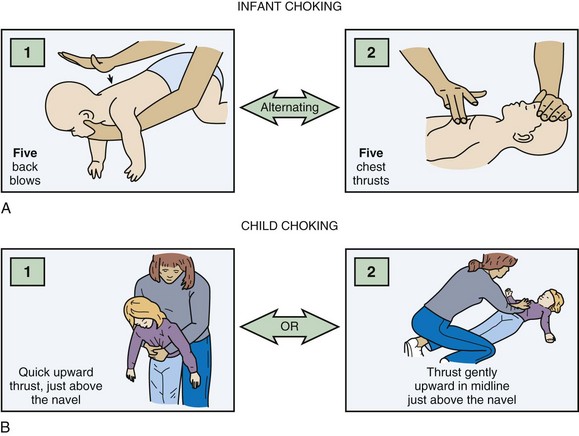
Foreign body removal maneuvers consist of a sequence of five back blows and five chest thrusts for infants and the Heimlich maneuver for children (Fig. 13.1). Blind finger sweeps should not be performed in children because a partial obstruction can be turned into a full obstruction if the foreign body is pushed further into the airway. Because of the pliability of the esophageal wall, foreign bodies in the esophagus can impinge on the trachea and result in airway obstruction. If the foreign body cannot be removed with basic life support maneuvers and the patient decompensates, the clinician can attempt to remove any visible foreign body with Magill forceps. Intubation may be required, and it may be possible to push the foreign body into a mainstem bronchus, most commonly on the right side. If this maneuver fails and the patient cannot be intubated, the last resort is either needle cricothyrotomy or a surgical airway. In a stable patient, bronchoscopy with maintenance of the patient’s position of comfort is the treatment of choice.
Airway Management
Airway management in children can be anxiety provoking; the same preparation guidelines outlined in Chapter 1 should be followed. Signs of respiratory failure include an increased or decreased respiratory rate, nasal flaring, grunting, retractions, cyanosis, apnea, or altered mental status. Hypoxia, compromised airway protection, altered mental status, and impending respiratory failure are common indications for pediatric airway intervention. Because most pediatric cardiac arrests are secondary to respiratory failure, early airway intervention is crucial.
Anatomy
The pediatric airway differs significantly from the adult airway (Box 13.1), and some special techniques are helpful when intubating a child. An oral or nasal airway can assist in maintaining airway patency. Because of the large occiput in a young child, typically those younger than 1 year, a towel roll placed beneath the patient’s shoulders often improves airway alignment. To visualize the very anterior pediatric airway, the operator must look up during intubation and may need to squat or raise the bed for adequate viewing. To see the glottic opening, a straight blade is recommended to lift up an infant’s floppy omega-shaped epiglottis. Because of infants’ small mouths, an assistant may need to pull the baby’s cheek to the side to allow passage of the laryngoscope and endotracheal tube.1,2
Box 13.1 Ways in Which a Child’s Airway Differs Anatomically from an Adult’s Airway
The prominent occiput can cause airway obstruction and impede glottic visualization during intubation; a 1-inch towel roll should be placed below the shoulders
Dependence on nasopharynx patency; nasal airways should be avoided in children younger than 1 year because their larger adenoidal tissue can bleed
The relatively larger tongues can obstruct the airway and often necessitate an oral or nasal airway
The epiglottis is omega (Ω) shaped and floppy; a straight laryngoscope blade is used to lift the epiglottis out of view
The larynx is more anterior and cephalad
The cricoid is the narrowest portion of the airway
Small tracheal diameter and distance between rings, which makes tracheostomy or cricothyrotomy more difficult; the American Heart Association recommends needle cricothyrotomy for difficult airways (see text discussion of this modality)
Much shorter tracheal length (newborn, 4 to 5 cm; 18-month-old child, 7 to 8 cm)
The endotracheal tube may easily be dislodged; frequently reassess position of the tube
Rapid-Sequence Intubation in Children
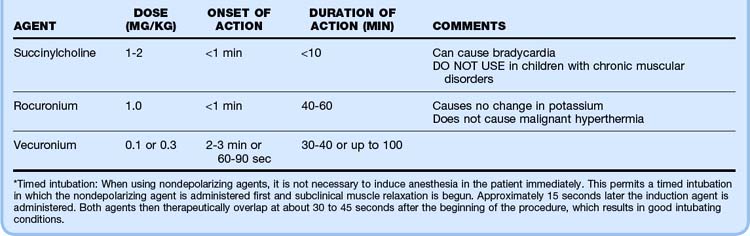
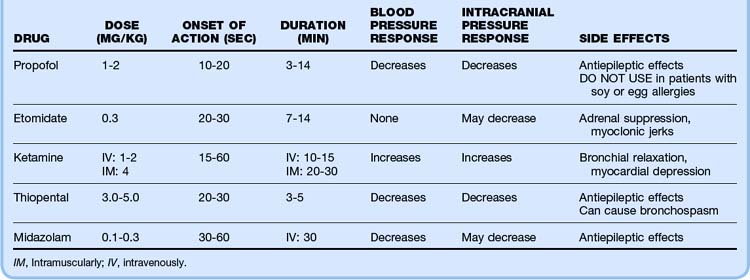
The intubating time line and drugs of choice are listed in Tables 13.1 and 13.2. Postintubation assessment includes confirmation that the endotracheal tube is in correct position. First listen over the stomach and then over the axillae for breath sounds. A confirmatory device such as an end-tidal carbon dioxide monitor, a carbon dioxide chart (e.g., Pedi-Cap, which should change from purple to yellow with proper tube placement), or an esophageal detector should be used.3,4 A nasogastric or orogastric tube should also be placed as soon as possible because any amount of gastric distention can make ventilation and oxygenation of a child difficult. A rough rule of thumb for nasogastric and orogastric tube size is two times the endotracheal tube size.
Pharmacologic Agents for Rapid-Sequence Intubation in Children
Potential combinations of agents for rapid-sequence intubation are listed in Table 13.3. Pretreatment with multiple agents is not recommended because placement of an advanced airway may be delayed. Atropine has recently been called into question for routine use in pediatric intubation, but it is recommended in infants younger than 1 year to avoid the bradycardia associated with airway manipulation in this population. The dose of atropine ranges from 0.01 to 0.02 mg/kg (minimum dose, 0.1 mg).
Table 13.3 Clinical Scenarios for Intubation and Recommended Induction Agents
| CLINICAL SCENARIO | INDUCTION AGENTS |
|---|---|
| Isolated head injury | |
| Status epilepticus | |
| Asthma | |
| Respiratory failure |
* Several intensive care unit studies have shown that in intubated patients, ketamine does not increase intracranial pressure and may help maintain cerebral perfusion pressure. However, no emergency department studies have been performed to date.
Adapted from a presentation by Sacchetti A. Boston: American College of Emergency Physicians Scientific Assembly; 2003.
Principles of Endotracheal Intubation
Recommended endotracheal tube sizes are listed in Box 13.2. With the advent of high-volume, low-pressure cuffed endotracheal tubes, the dictum of using only uncuffed endotracheal tubes in children younger than 8 years has changed. It is not only acceptable but at times preferable (high peak pressure) to use a cuffed endotracheal tube in children. For an approximate guide to tube size, use 4 + (age ÷ 4) for uncuffed tubes and 3.5 + (age ÷ 4) for cuffed tubes. Cuff inflation pressure should be kept less than 20 to 25 cm H2O. Cuffed endotracheal tubes are not recommended for use in neonates.5,6
Box 13.2 Ways of Choosing Endotracheal Tube Size
Table 13.4 summarizes the procedure for rapid-sequence intubation in children.
Table 13.4 Procedure for Rapid-Sequence Intubation in Children
| Time to intubation 5 min | Start preoxygenation |
| Time to intubation 3 min | Give any premedication (atropine, lidocaine) |
| Intubation time | Push induction and paralytic agents |
| After the patient is relaxed | Intubate: |
| Apply cricoid pressure | |
Use the BURP (b
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|