Chapter 54 Pediatric Neurocritical Care
Historical Context
Advances in medical care have either emerged as a result of tectonic shifts of the mantle of the health care system or by incremental shifts of the landscape. As an example, military conflicts have contributed to cataclysmic changes in health care, from the development of life-saving trauma surgical techniques (from the U.S. Civil War to current conflicts) to the development of effective triage systems for evacuating and treating wounded soldiers (culminating in improved systems developed during World War II through the Korean and Vietnam conflicts).1 As a specialty, Critical Care Medicine was a product of yet another seismic blast to the health care system—the polio epidemics that raged throughout Europe and the United States in the late 1940s and early 1950s. Advances in ventilation allowed patients to survive this debilitating affliction, culminating in the organization of the first intensive care unit (ICU) at the Baltimore City Hospital in 1961 that was staffed by in-house physicians.2 The director of this first multidisciplinary ICU was Dr. Peter Safar, a founding father of cerebral protection from cardiac arrest who advanced the field of neuroprotection during his long, storied career.
The subspecialty of neurological critical care has evolved in a more gradual fashion compared with the overall specialty. Dr. D.W. Dandy is credited with developing the first three-bed neurosurgical ICU at the Johns Hopkins Hospital in Baltimore in 1929, while the first fully staffed, large-scale neurocritical care unit was formed in 1969 at the University of Colorado by Dr. Michael Earnest.3 Gradually, similar neurological critical care units were established in many universities and tertiary care centers, paralleling the development of other subspecialty ICUs for coronary, cardiovascular, surgical, pulmonary, and other conditions. Currently neurological critical care units can be further subdivided in many centers into neurotrauma, neurovascular, neurosurgical, and others. In 2002, several dozen practicing neurointensivists formed the Neurocritical Care Society (with membership now numbering greater than 800) and held its first annual meeting in February 2003. And in 2007, the United Council on Neurological Subspecialties offered the first examination in neurocritical care and accredited fellowship programs across the United States.
For pediatrics, caring for neurologically injured children was always at the forefront in establishing critical care programs. In their landmark paper from 1975, Downes and Raphaely4 begin by writing, “The major objective of intensive care is to provide maximum surveillance and support of vital systems in patients with acute, but reversible life-threatening disease. In pediatric patients, the reversal of life threatening conditions and preservation of essential functions, especially those of the brain, may result in many years of useful life.” During this time, Reye’s syndrome epidemics were commonly afflicting previously healthy children and intensive neuroprotective measures were used with increasing success to restore full neurologic function.5
These early years of pediatric critical care led to many advances, including: (1) management of respiratory failure (e.g., the advent of exogenous surfactant for respiratory distress syndrome,6,7 high-frequency oscillatory ventilation,8 permissive hypercapnia, inhaled nitric oxide,9 and extracorporeal membrane oxygenation10); (2) surgical correction of congenital heart diseases (e.g., palliative surgery—Blalock-Taussig shunts,11 the Norwood procedure,12 definitive repair—arterial switch procedure for Transposition of the Great Vessels, the Fontan procedure,14 supportive care—cardiopulmonary bypass,15,16 and ventricular-assist devices17,18); (3) therapies for sepsis (e.g., goal-directed resuscitation therapy19 and development of new antibiotics); and (4) supportive therapies for failing organs (e.g., hemofiltration, hemodialysis, continuous renal replacement therapy, plasmapheresis/plasma exchange, and organ transplantation). The culmination of these and many other clinical advances have led to decreases in mortality rates in most pediatric critical care units to between 3% to 5%.
With this impressive reduction in mortality, the necessary next step in improving clinical care for critically ill children is to minimize morbidity. It is in this context that pediatric neurocritical care has emerged, because neurologic morbidity was seen as one of the greatest challenges to future advancement of the field. In 2000, Robert Tasker20 was among the first to write about a conceptual framework of multiple neurologic conditions that might benefit from particular expertise within pediatric neurocritical care when he provided an evidence-based summary of three important neurologic conditions of critically ill children: the management of severe head injury, use of benzodiazepines to treat status epilepticus, and the emergence of new forms of encephalopathies in children. In the intervening years, various groups have argued for the introduction of pediatric neurocritical care within the specialty of pediatric critical care medicine. The remainder of this chapter will examine the various rationales for advancing pediatric neurocritical care programs and possible future directions for this effort.
Rationales for Development of Pediatric Neurocritical Care
Rationale 1
An important question for the development of pediatric neurocritical care programs involves an assessment of whether there are enough patients to justify the formation of this type of clinical service. As stated earlier, adult neurocritical care units and programs have been in existence for years and have therefore answered this question in the affirmative. During their early period, Bleck and colleagues21 surveyed admissions to their 14-bed general medical ICU and found that only 92 of 1850 admissions were related directly to neurologic conditions, mostly stroke and intracerebral hemorrhages. However, they found that 217 patients experienced neurologic complications during the admission, including hypoxic/ischemic encephalopathy, seizures, metabolic encephalopathy, and stroke. A more recent analysis demonstrated that brain tumors, strokes, and subarachnoid hemorrhages accounted for more than 50% of admissions to neurocritical care units22 but failed to provide an absolute number of admissions. In the intervening years, thrombolytic therapy for ischemic stroke, neurovascular procedures for aneurysmal subarachnoid hemorrhage, and the advent of comprehensive traumatic brain injury and stroke teams have increased the need for intensive care for adults. The evidence that adult neurocritical care is a viable program in many centers largely rests with its widespread implementation. Although the absolute number of neurocritical care units has not been collated, the United Council of Neurological Subspecialties has certified 25 programs in the United States and 215 diplomates in Neurocritical Care (see http://www neurocriticalcare.org/files/public/NCS. neurocriticalcare.org/files/public/NCS Volume4Number4).
The only pediatric experience in subspecialty critical care program development comes from pediatric cardiac intensive care programs. Large pediatric institutions—for example, Children’s Hospital of Boston, Children’s Hospital of Philadelphia, and The Hospital for Sick Children in Toronto—have long histories of cardiac intensive care programs.23 These programs are based on the philosophy that a multidisciplinary team of cardiac intensivists, cardiologists, cardiac surgeons, anesthesiologists, neonatologists, and specially trained nursing and ancillary staffs can most effectively treat the unique pathophysiology encountered in correction of congenital heart disease. The viability of these programs is generally related to the volume of congenital heart surgery cases referred to the institution, and patients admitted to the hospital on this service generally are located in a unique space outside of the general pediatric intensive care unit (PICU). As of 2004, there were 132 pediatric cardiac intensive care programs and 250 members of the Pediatric Cardiac Intensive Care Society (http://www.pcics.org/), indicating that these types of programs have certainly been viable for many institutions.
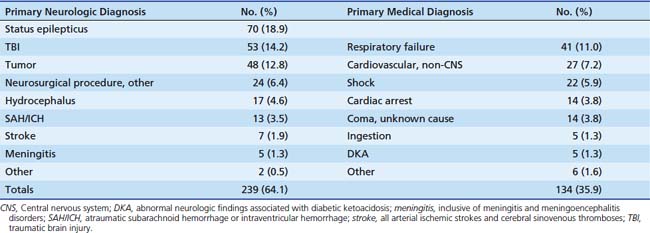
At the time of this writing, limited information exists regarding the number of patients receiving care in pediatric neurocritical care programs. LaRovere and Riviello24 summarized their experience in developing a pediatric neurocritical care service at Children’s Hospital of Boston. They reported that 557 neurocritical care consultations were obtained over a multiyear period. Because little information is provided about the disorders treated and the role of the pediatric neurocritical care team in patient management, it is difficult to discern the precise difference between this effort and an active neurologic consulting service. At Children’s National Medical Center, a neurocritical care consulting service consisting of an intensivist, two neurologists, and neurosurgical staff was formed within the framework of the PICU.25 This service was designed to improve collaboration between the services and implement evidence-based guidelines for care of children with traumatic brain injury, stroke, status epilepticus, and other neurologic disorders. In a 14-month period, 373 neurocritical care consults were obtained from 1423 patient admissions. Approximately two thirds of the consultations were obtained in children with primary neurological diagnoses at PICU admission, but a substantial portion (34.1%) of the consultations were obtained among children admitted with other medical/surgical conditions (Table 54-1). The wide variety of diagnoses observed argued strongly that at least the three main specialties (intensivist, neurologist, and neurosurgeon) were required to make a comprehensive clinical team. Weaknesses of this study included the inability to determine if the consulting service led to improved outcomes for patients and lack of analysis on the financial viability of this model of care. Most recently, a fully independent primary pediatric neurocritical care service staffed by intensivists with extensive neurological experience has begun at the Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center. This service has seen 297 patients in the first 9 months, and a full description of the patient composition and viability of the program is currently under review. Other pediatric neurocritical care programs are currently active at several institutions, including at Children’s Memorial Hospital (Northwestern University), St. Louis Children’s Hospital (Washington University in St. Louis), and Weill-Cornell Medical Center.
Table 54–1 Admission Diagnoses for Children Who Had a Pediatric Neurocritical Care Medicine Consultation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








