19 Pediatric Cardiac Disorders
• Congenital heart disease is typically diagnosed in utero or before discharge from the newborn nursery, but delayed manifestations usually occur within the first 2 weeks of life when the ductus arteriosus closes.
• Congenital heart disease should be considered in a neonate who is in shock or has congestive heart failure or cyanosis.
• Subtle signs of cardiac disease in children include sweating, irritability, and poor feeding.
• Echocardiography is used for the diagnosis of structural congenital heart disease.
• Prostaglandin E1 can be lifesaving in cases of ductal-dependent congenital heart disease.
Epidemiology
Structural CHD occurs in approximately 8 in 1000 live births.1 Most congenital lesions are diagnosed in utero or in the newborn nursery, but a significant proportion may not be manifested until 1 to 2 weeks of life, when the ductus arteriosus closes. In fact, a significant proportion of cases of CHD are diagnosed after hospital discharge. Normal findings on newborn evaluation does not rule out potentially significant and lethal lesions, and a high index of suspicion is critical to ensure timely diagnosis.2 Many risk factors for the development of CHD have been identified (Box 19.1), including a family history of CHD, maternal diabetes (associated with ventricular septal defect [VSD], hypertrophic cardiomyopathy, and transposition of the great arteries [TGA]), and fetal drug exposure (e.g., Ebstein anomaly with maternal lithium therapy). Pediatric cardiac disease may be challenging because it may mimic more common illnesses, such as sepsis.
Box 19.1 Risk Factors for the Development of Congenital Heart Disease
Risk for congenital heart disease is increased with one affected parent or sibling and is three times greater if two close relatives have such disease.
Maternal diabetes is associated with hypertrophic cardiomyopathy, ventricular septal defect, and transposition of the great arteries.
Maternal phenytoin use is associated with aortic stenosis and pulmonic stenosis.
Maternal lithium use is associated with Ebstein anomaly.
Fetal alcohol syndrome is associated with atrial septal defect and ventricular septal defect.
Rhythm disturbances are also important causes of pediatric cardiac disease and can occur in children with structural heart disease or in those with structurally normal hearts. SVT is the most common pediatric cardiac arrhythmia and includes atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT), and preexcitation conditions such as Wolf-Parkinson-White syndrome. Congenital complete heart block is associated with maternal connective tissue disease and the presence of anti-Ro/SSA and anti–La-SSB antibodies. Long QTc syndrome may be congenital or acquired; the congenital form is estimated to occur in 1 in 7000 to 10,000 live births.3 Congenital long QTc syndrome may occur in an autosomal dominant form (Romano-Ward syndrome) or in an autosomal recessive form (Jervell and Lange-Nielsen syndrome) associated with sensorineural hearing loss.
Pathophysiology
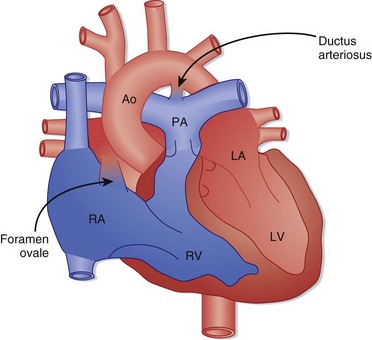
Fetal circulatory anatomy is designed to transport oxygenated blood from the placenta to the systemic circulation while bypassing the lungs (Fig. 19.1). Fetal oxygenation occurs at the placenta, and blood is returned to the right atrium through the ductus venosus after bypassing the liver. Most of the oxygen-rich blood is shunted across the foramen ovale into the left atrium and is then delivered to the systemic circulation via the aorta. Some flow travels from the right atrium into the right ventricle and enters the pulmonary arteries. The pulmonary vasculature is constricted, and flow is shunted through the ductus arteriosus and mixes with blood in the aorta to supply the systemic circulation.
Birth results in a complex series of changes induced by expansion and oxygenation of the lungs. Oxygenation of the lungs leads to a marked decrease in pulmonary vascular resistance and a subsequent increase in pulmonary blood flow. Increasing pulmonary blood flow results in greater return of blood to the left atrium, which functionally closes the foramen ovale (the foramen may remain “probe patent” into adulthood). The decrease in pulmonary vascular resistance is coupled with an increase in systemic vascular resistance, and ductal flow reverses to become left to right. The blood traversing the ductus arteriosus is now highly oxygenated, a change that typically stimulates closure by 48 hours of life. In certain cases, the ductus arteriosus does not close until 1 to 2 weeks of life, and so-called ductal-dependent cardiac lesions may be manifested at this time (Box 19.2). The increased pressure and volume demands on the left ventricle stimulate growth of the left ventricle, and the decreased load on the right ventricle from decreased pulmonary vascular resistance results in a reduction in right ventricular mass.
Presenting Signs and Symptoms
Infants with previously undiagnosed structural CHD are typically initially seen in the emergency department (ED) with shock, congestive heart failure (CHF), cyanosis, or a combination of these symptoms. Left-sided obstructive lesions such as hypoplastic left heart syndrome and coarctation of the aorta are manifested as shock as the ductus arteriosus closes and the blood supply to the systemic circulation dwindles. Shock can also be the initial sign of total anomalous pulmonary venous return (TAPVR) with obstruction. Evidence of poor perfusion, such as lethargy, mottled extremities, tachycardia, and tachypnea, is typically present. Sepsis and other noncardiac conditions (e.g., salt-wasting crisis in congenital adrenal hyperplasia) can cause similar findings. Shock may also be the manifestation of SVT or complete heart block that has become decompensated (Table 19.1).
Table 19.1 Differential Diagnosis of Shock in Infants
| TYPE OF SHOCK | POSSIBLE CAUSES |
|---|---|
| Hypovolemic | |
| Cardiogenic | |
| Distributive |
CHF is a common manifestation of both structural heart disease and congenital rhythm disturbances. Although respiratory distress, tachypnea, and rales may be present, subtler signs such as poor feeding and hepatomegaly may be the only manifestations of CHF. Assessment of the liver’s edge is a critical portion of the physical examination in these infants. Peripheral edema as a manifestation of CHF is rare in infants. Acyanotic heart diseases with large left-to-right shunts, such as congenital aortic stenosis, interrupted aortic arch, and coarctation of the aorta, are manifested as CHF because blood preferentially flows into the low-resistance pulmonary bed (Box 19.3). TAPVR and VSD can also be manifested as CHF as a result of volume overload of the right ventricle. Rhythm abnormalities such as sustained SVT and congenital complete heart block can likewise be manifested as CHF as a result of poor forward flow.
Cyanosis can be the first manifestation of CHD in infants, and severe lesions are typically diagnosed in utero or in the newborn nursery. Some lesions may escape detection, however, and first be recognized later in the neonatal period. Central cyanosis affecting the lips, mucous membranes, and trunk is due to decreased arterial oxygen saturation and is always pathologic. The differential diagnosis of central cyanosis is presented in Table 19.2. Peripheral cyanosis limited to the extremities or circumoral region is a normal newborn finding but can also be due to non-CHD causes such as sepsis, exposure to cold, and poor cardiac output.
Table 19.2 Differential Diagnosis of Central Cyanosis in Infants
| Cardiac Causes | |
| Right-to-left shunting | |
| Pulmonary Causes | |
| Right-to-left shunting | |
| Ventilation-perfusion mismatch | |
| Hypoventilation | |
| Hematologic Causes | |
| Hemoglobinopathies | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree