PAIN: JOINTS
RICHARD J. SCARFONE, MD AND AARON CHEN, MD
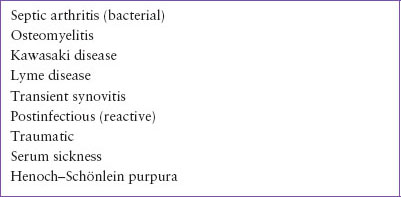
Arthritis and arthralgia are common reasons for children to seek care in the emergency department (ED). Arthritis is joint inflammation marked by swelling, warmth, and limitation of motion; arthralgia is joint pain without inflammation. Establishing a diagnosis for the child with joint pain is challenging because the differential diagnosis is lengthy (Table 55.1), clinical and laboratory findings are rarely specific for a particular disease, and disease patterns for many of the etiologies are often highly variable among different patients. Among the most common causes of joint pain in children are infections, trauma, and postinfectious conditions (Table 55.2), whereas those most likely to be life-threatening are due to systemic disease and malignancy (Table 55.3). This chapter serves as a guide to the approach to the child with arthritis or arthralgia, with an emphasis on historical points and physical examination findings that can serve to narrow the diagnostic possibilities.
DIFFERENTIAL DIAGNOSIS
The initial differential diagnosis usually focuses on the most common or potentially serious etiologies (Tables 55.2 and 55.3). Children from 6 to 24 months of age have the highest incidence of nongonococcal bacterial (septic) arthritis, which results primarily from the hematogenous dissemination of an organism. The diagnosis of septic arthritis of the hip should not be delayed because pressure in the joint space will compromise the vascular supply to the femoral head, leading to necrosis (see Chapter 102 Infectious Disease Emergencies).
Osteomyelitis involving the distal end of long bones may manifest as arthralgia with or without objective signs of joint inflammation. Children with sickle cell anemia and Type 1 diabetes mellitus are at higher risk. Onset of symptoms is typically more indolent compared to septic arthritis.
In the first 10 days of illness, children with Kawasaki disease may have arthritis or arthralgia, often involving smaller joints in the hand. Beyond that time, involvement of larger joints of the lower extremities is more common. If an arthrocentesis is performed, the synovial fluid analysis resembles that seen with septic arthritis with 100,000 to 300,000 white blood cells (WBCs) per cubic millimeter (see Chapter 109 Rheumatologic Emergencies).
In the absence of a clear history of a tick bite, arthralgia secondary to early, localized Lyme disease may be a challenging diagnosis to establish because only about 40% to 70% of children have the characteristic erythema migrans rash, constitutional symptoms may be mild, and serologic tests will be normal in the early stages of disease. However, serologic testing will be confirmatory in patients with Lyme arthritis secondary to disseminated disease. Among those with monoarticular arthritis, it may be difficult to distinguish septic arthritis from arthritis associated with Lyme disease on clinical grounds alone, with or without analysis of synovial fluid. There are clinical features that favor the diagnosis of Lyme disease such as knee involvement, absence of recent fever, and lower inflammatory markers, but these characteristics may be shared with a subset of patients who have septic arthritis. Complicating this further is that synovial fluid analysis may not be definitive. There is a wide range of synovial WBC counts in children with Lyme disease and although median values are lower than those typically seen in patients with septic arthritis, there is considerable overlap. Given the difficulties of distinguishing Lyme disease from septic arthritis among children presenting with monoarticular arthritis, management of cases where suspicion for septic joint is significant may require an approach that includes analyzing synovial fluid and performing Lyme serology testing, especially if one practices in a region where Lyme disease is not endemic.
Transient (also called toxic) synovitis is a poorly understood inflammation of large joints, afflicting children 3 to 6 years of age. The diagnosis is typically made on clinical grounds, and this self-limited disease does not result in joint destruction. When the hip is involved, the challenge for clinicians is to distinguish transient synovitis from Lyme (in endemic areas) or septic arthritis.
Reactive, or postinfectious, arthritis is probably more common than septic arthritis. Arthritis following various enteric infections is not rare in children, and joint complaints after parvovirus B19 infection are seen among adolescents. Chlamydia trachomatis infection of the genitourinary tract should be considered in any sexually active adolescent with new-onset arthritis. With postinfectious arthritis, antimicrobial treatment does not modify the disease course.
Traumatic injuries to a joint may cause periarticular swelling or an effusion indicative of a hemarthrosis. In addition, ligamentous or tendon injuries will result in joint pain and impaired range of motion. Serum sickness and Henoch–Schönlein purpura (HSP) are marked by characteristic rashes.
EVALUATION AND DECISION
Figure 55.1 depicts an algorithm for the diagnostic approach to the child with joint pain. The evaluation should include inquiries about the specific joint(s) involved, symptom duration, and history of trauma, fever, rash, tick bites, sexual risk factors, intravenous drug use, and recent illnesses. The child’s past medical and family histories should be reviewed. A family history of systemic lupus erythematosus (SLE), inflammatory bowel disease, or rheumatoid arthritis increases the child’s risk for these diseases.
A comprehensive physical examination should be performed with particular attention paid to a search for rashes, heart murmurs, and abdominal abnormalities. Assessment of the affected joint(s) should determine if it is warm, swollen, or tender as well as its range of motion.
TABLE 55.1
JOINT PAIN—DIFFERENTIAL DIAGNOSIS
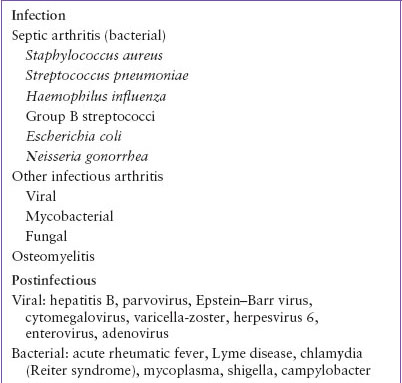
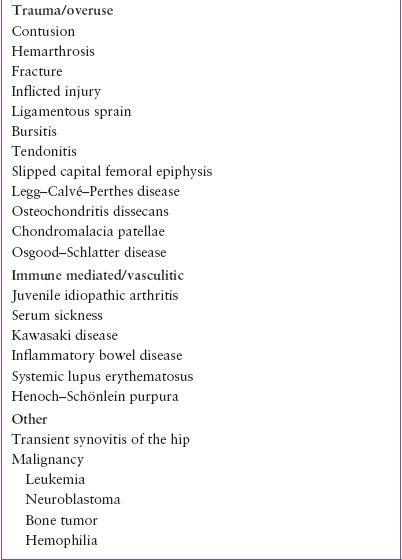
TABLE 55.2
COMMON CAUSES OF JOINT PAIN
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







