PAIN: EARACHE
MARK D. JOFFE, MD
Ear pain or otalgia is a very common chief complaint in children seeking emergent or urgent care. In younger, preverbal children, ear pain is often inferred by parents from various child behaviors. While acute otitis media (AOM) may be the main parental concern, astute clinicians must consider a broader range of potential causes. Otalgia may result from diseases in all parts of the ear, and also from a variety of nonotogenic conditions. When ear pain is accompanied by neurologic signs and symptoms such as cranial nerve palsies, vertigo, or altered mental status, a more extensive evaluation is required.
DIFFERENTIAL DIAGNOSIS
Ear pain may be the presenting symptom of problems in external, middle, or inner ear (Fig. 53.1). Causes of external ear pain are often readily apparent. Trauma to the auricle is ascertained by history in most cases, and contusions, abrasions, hematomas, and lacerations are easily noted on physical examination. In younger children, and in particular in cases of inflicted injury, a history of ear trauma may be lacking. Swelling and/or bruising of the external ear, especially the medial aspect of the auricle, from forcible traction is a well-recognized manifestation of child abuse. Hematomas of the auricle are of particular concern because, interposed between the skin and underlying cartilage, the extravascular accumulation of blood disrupts the supply of nutrients to the cartilage. Necrosis of auricular cartilage leads to deformity and results in the characteristic “cauliflower ear.” Pressure dressings on injured external ears may prevent the accumulation of significant auricular hematomas. Larger auricular hematomas may need to be drained.
The popularity of body piercing, and in particular multiple piercings of the ear, has increased the number of patients requiring treatment for complications. Infections of the ear lobe or of the cartilaginous portions of the auricle after piercing should be treated with topical and sometimes systemic antibiotics. While Staphylococcus aureus is the most frequent pathogen, cartilaginous infection with Pseudomonas aeruginosa is well described and requires specific treatment. Drainage, debridement, and treatment with fluoroquinolone antibiotics may be necessary. Preauricular cysts or sinuses may become infected. A small pit just anterior to the helix is noted in the center of the surrounding tender, red swelling.
Frostbite of the helix presents as a painful, pale ear that usually becomes hyperemic and swollen over time. Vesicles may develop in the latter stages. Rapid rewarming and analgesia are recommended. Most authorities discourage debridement of vesicular or hemorrhagic lesions.
Cerumen impaction may cause ear pain, especially after attempts to remove accumulations push the ear wax up against the tympanic membrane (TM). Removal of cerumen with a curette is best accomplished under direct visualization. Dry cerumen may be tightly adherent to the skin of the external canal which, when removed with a curette, causes abrasion and bleeding. Saline irrigation of the canal or instillation of peroxide-containing ear drops or docusate liquid can remove, soften, or detach adherent wax and is recommended prior to attempting to remove dry cerumen with a curette.
Children may have ear pain from foreign bodies placed in the ear. If the foreign body is difficult to remove or is close to the TM, removal under sedation by an otolaryngologist is advisable. Occasionally, live insects are noted in the external canal and their movement causes great pain and distress. Instillation of mineral oil will asphyxiate the insect prior to removal. Viscous lidocaine may have the added benefit of paralyzing the insect, reducing painful movements more quickly than mineral oil.
Shingles of the ear, or herpes zoster oticus, presents with painful or pruritic vesicles of the external auditory meatus and may also involve the TM. Although more common in adults, associated facial nerve palsy (Ramsay Hunt syndrome), hearing loss, or vertigo have been reported in children. Antiviral agents and systemic corticosteroids may be helpful in the early stages of this illness.
Labyrinthitis usually presents with vertigo that may be associated with nausea and vomiting, balance disturbance, and tinnitus. It is usually caused by a viral or bacterial infection of the inner ear, but may also be associated with middle ear infection and ear pain.
OTITIS EXTERNA
Otitis externa is a common problem during childhood, especially during summer when children are swimming and humidity is high. Cerumen is produced by glands in the external ear to coat the canal with a water-resistant, acidic, antibacterial substance that prevents maceration. Swimmers ear develops when water in the ear disrupts the protective cerumen layer. Attempts to remove water in the canal or to relieve pruritus may cause injury to the skin, creating portals of entry for bacteria in the external ear. Ear pain and sometimes visible ear discharge are the usual symptoms of otitis externa. Examination reveals an erythematous, swollen external canal filled with debris or purulence. Traction on the auricle causes pain with otitis externa, a finding that can help distinguish it from otitis media with perforation. Gentle removal of debris, instillation of topical antibiotics, and systemic analgesia are the usual treatment. When swelling is so severe that topical antibiotics may not reach the more proximal portion of the canal, a wick may be inserted to facilitate antibiotic entry. Systemic antibiotics are indicated if there is extensive cellulitis spreading beyond the external canal. Otitis externa is usually polymicrobial, but S. aureus and P. aeruginosa are important pathogens to cover, and polymyxin/neomycin or fluoroquinolone otic drops are the preferred treatment. Otitis externa with P. aeruginosa can be fulminant and necrotizing. Recalcitrant cases of otitis externa, especially if pruritus is a prominent symptom, may require evaluation for fungal disease (otomycoses) or deeper infection.
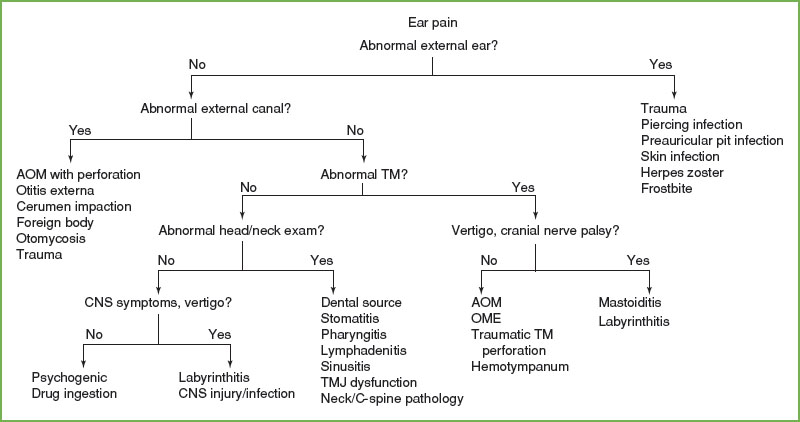
FIGURE 53.1 Ear pain algorithm. AOM, acute otitis media; CNS, central nervous system; TMJ, temporomandibular joint; OME, otitis media with effusion.
ACUTE OTITIS MEDIA
Otitis media is the most common illness prompting office visits and antimicrobial prescriptions in childhood, though both visits and prescriptions of OM have decreased. Clinical practice guidelines have encouraged a stricter diagnostic threshold for AOM, and immunization with PCV7 and influenza vaccines may have reduced the actual incidence of AOM.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







