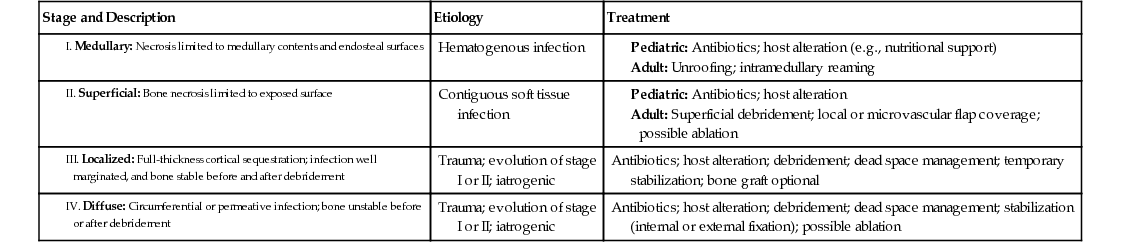
Ruta M. Shah Osteomyelitis is inflammation of the bone caused by infection. It is one of the most difficult-to-treat infectious diseases. It can lead to progressive destruction of bone and formation of sequestra, making it difficult to cure in many cases. Infection of bone has been classically divided into three groups: (1) hematogenous osteomyelitis, seeded from bacteremia; (2) osteomyelitis associated with a contiguous focus, such as a puncture wound, foreign body, or adjoining soft tissue infection; and (3) osteomyelitis associated with peripheral vascular disease, such as diabetic foot infections or other vascular insufficiency.1 These groups may be further divided into acute and chronic varieties. Acute osteomyelitis is generally defined as infection before the development of bone necrosis; chronic osteomyelitis indicates the presence of osteonecrosis, and its removal often requires surgical debridement.1 Clinically, acute disease can manifest as the sudden onset of inflammation, warmth, redness, and edema. Hematogenous osteomyelitis in the young is most likely to be seen acutely, usually with a single organism seeding the medullary cavity, and a good prognosis can be predicted. This entity is most commonly seen in children (50% of cases occur in children younger than 5 years), with a second peak occurring in older adults. In contrast to acute disease, chronic osteomyelitis develops during long periods, often months or longer.1 Osteomyelitis with vascular insufficiency in older adults is an example of these more indolent infections. In this situation, an external focus erodes into the superficial periosteum. Formation of sinus tracts is also a potential feature. The flora is usually mixed, and the prognosis varies greatly with factors such as the extent of bone involvement, the presence of sequestra, areas of denuded dead bone, the type of organism, and host conditions. Acute osteomyelitis that is not diagnosed or that is inadequately treated may advance to chronic osteomyelitis, resulting in a more complicated clinical picture.2 Two major classification schemes exist for osteomyelitis. The Waldvogel classification system is based on the cause of the infection (hematogenous versus a contiguous focus of infection) and duration of illness (acute versus chronic) but does not provide information about specific therapeutics.2 The classification scheme by Cierny and colleagues takes into consideration the extent of anatomic involvement (anatomic stage) and host factors (physiologic class), providing a guide to determination of the prognosis, extent of surgical intervention, and antibiotic treatment required.3 Depending on the anatomic stage, further surgical resection, revascularization, muscle flaps, skin grafts, management of dead space, and bone grafts may be required (Table 185-1). Physiologic class is divided by characteristics of hosts classified as A, B, or C (Box 185-1).4 A favorable prognosis accompanies A hosts, who have normal vasculature and metabolic factors and a normal immune system. B hosts carry a worse prognosis by virtue of local or systemic compromise. Systemic factors, such as diabetes, smoking, malnutrition, hypoxia, immunosuppression, or immunodeficiency, and local factors, such as lymphedema, venous stasis, arterial insufficiency, or sensory deficits, may require attention during treatment. C hosts represent a group for which treatment of the osteomyelitis may be worse than the disease itself. The Cierny-Mader staging system is important to medical and surgical management but also guides prognosis and education. Pathogenesis of osteomyelitis is affected by the organism and its virulence, age of the patient, immunocompromise and comorbidities, and type of bone affected. In children, hematogenous spread is the most common route of infection, most commonly affecting the long bones. This may also extend into the joint space, causing septic arthritis. Acute inflammation contributes to destruction of bone. This inflammation then compromises blood flow and leads to further bone destruction and the formation of sequestra. Antibiotics penetrate these areas poorly, often leading to an inadequate response to treatment with antibiotics alone. The periosteum can thicken and surround this area of dead bone, forming an enclosed capsule (involucrum). Surgical intervention is often needed to debride necrotic tissue.2 In children, Brodie’s abscess is an example of this type of enclosed infection commonly found in the metaphysis. Infecting organisms also differ according to the patient’s age and condition and whether the focus is contiguous or hematogenous. Staphylococcus aureus is the most commonly isolated pathogen overall (isolated in 70% of culture-positive cases), and there has been a significant increase in methicillin-resistant Staphylococcus aureus (MRSA) infection.5,6 A single organism is the norm for hematogenous osteomyelitis. Infants most often harbor S. aureus, Streptococcus pyogenes, and gram-negative enteric organisms. With the advent of Haemophilus influenzae type b (Hib) conjugate vaccine, H. influenzae is now uncommon in children older than 1 year. Salmonella can cause infection in patients with sickle cell disease.7 Patients with sickle cell disease are a unique subset of patients, and microbiologic data are essential to determining the appropriate antibiotic regimen. In adults, S. aureus is also the dominant pathogen in both hematogenous and contiguous osteomyelitis. However, practitioners should be aware that in patients with chronic ulceration and vascular insufficiency, mixed infection is more commonly present. Organisms such as S. aureus, streptococci, anaerobes, and gram-negative bacilli are involved.8 Again, the prevalence of MRSA, including community-acquired strains, continues to be on the rise. This pathogen must therefore be considered in all patients with osteomyelitis, not only those with health care exposures.7 Some of these MRSA isolates harbor the Panton-Valentine leukocidin (PVL) gene, which has been associated with more aggressive soft tissue and multifocal infection, as well as protracted fever and bacteremia. The need for surgical drainage is also more common in these patients.7 Osteomyelitis is largely a clinical diagnosis with supportive data from imaging and cultures. Patients can have a variety of symptoms. In children, symptoms may include fever, decreased range of motion, and pain and may evolve during a few days to weeks. However, the onset can be insidious, which may delay diagnosis.6 Chronic osteomyelitis can develop after inadequately treated osteomyelitis and can manifest in the patient with a history of osteomyelitis as recurrence of pain, swelling, and a draining sinus.1 In adults, acute osteomyelitis is less commonly hematogenous, and when it is, it usually affects the vertebrae. Osteomyelitis can also occur by direct inoculation from trauma or surgery or in diabetic patients with vascular insufficiency and skin ulceration. Patients can manifest local symptoms such as fever, pain, erythema, and swelling. However, more commonly, patients may have a subacute presentation, with nonspecific pain and vague symptoms being the norm. Chronic osteomyelitis may manifest with a draining sinus tract. Adjacent ulcer and soft tissue cellulitis may mask bone tenderness.9 In such a situation, the diagnosis of chronic osteomyelitis can be difficult. Large diabetic foot ulcerations and exposed bone or probing to the bone predict a high likelihood of osteomyelitis. Chronic osteomyelitis is seldom associated with fever or leukocytosis, and inflammation markers can also be normal. Subacute presentation of osteomyelitis may challenge health care providers caring for patients with fever of unknown origin. Physical examination may elicit bone tenderness. Ulcers with visible bone or sinus tracts that probe to bone are usually diagnostic of osteomyelitis.10 In these circumstances, specific diagnostic imaging tests may not be necessary. Special situations and clinical syndromes are important to recognize and are briefly discussed here. Low back pain is a common problem for which a precise source may not be discovered in a large number of patients. Health care providers should be aware of warning signs that should lead to further investigation (Box 185-2). Back pain is the most common initial symptom for vertebral osteomyelitis. Fever and leukocytosis are absent in 50% of cases, and tenderness of the spine to palpation is also not invariably present.11 Therefore, diagnosis is often delayed, and a high level of clinical suspicion must be maintained. Pyogenic vertebral osteomyelitis is usually hematogenous and therefore commonly a complication of initial primary infection. This primary source is elucidated in about 50% of cases.12 An example is infective endocarditis. A high rate of infectious endocarditis and spontaneous vertebral osteomyelitis has been reported (27% to 31%).12 Early diagnosis of infectious endocarditis in patients with a diagnosis of vertebral osteomyelitis is critical because surgical or other specific interventions may be required. Clinical features that may raise concern for infectious endocarditis in a patient with vertebral osteomyelitis include a predisposing cardiac condition or valve replacement, bacteremia with a gram-positive organism (e.g., Streptococcus, Enterococcus, and Staphylococcus species) as opposed to a gram-negative organism, and poorer prognosis.12 Osteomyelitis may be recognized by a radiologic process that involves both sides of the vertebral disk and adjacent vertebrae symmetrically. Malignant disease does not cross the disk to involve adjacent vertebrae.13 Early recognition is important because posterior extension causes epidural abscess and cord compression. Severe and lancinating back pain may be suggestive of epidural abscess.14 Collapsed vertebrae may also threaten the spinal cord. The course may be complicated by paravertebral, epidural, and psoas abscesses, all of which must be drained.15 Pyogenic vertebral osteomyelitis is primarily a disease of adults and is usually hematogenous and insidious in onset. Pain evolves gradually during weeks to months. Fever and leukocytosis are absent in 50% of cases. Although S. aureus is the predominant organism, gram-negative organisms can also cause vertebral osteomyelitis. The most common sources are urinary (32%) and abdominal (25%). In a significant percent, the source remains occult.15 In young patients with injection drug use, organisms such as Pseudomonas aeruginosa, Candida species, and S. aureus (including MRSA) must be considered. A patient history for potential environmental exposures, which may suggest exposure to a particular endemic pathogen, should also be obtained. The possibility of unusual pathogens, such as Candida species, other fungi,16 mycobacteria, and gram-negative organisms, emphasizes the need to make a causative diagnosis whenever possible if treatment is to be successful.
Osteomyelitis
Definition and Epidemiology
Pathophysiology
Clinical Presentation
Physical Examination
Vertebral Osteomyelitis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Osteomyelitis
Chapter 185