ORAL LESIONS
MARISSA A. HENDRICKSON, MD AND MARK G. ROBACK, MD
Children of all ages experience oral lesions, representing a wide range of illnesses. Lesions range from benign and self-resolving to indicative of life-threatening diseases. Many oral lesions, both congenital and acquired, are localized. However, lesions associated with systemic disease must also be considered (Fig. 47.1 and Table 47.1). Most often, patients with isolated complaints (e.g., a mouth sore or mass, drooling, pain, fever) are found to have common, self-limited conditions (Table 47.2). However, a complete history and physical examination is essential for all patients with oral lesions to rule out systemic and potentially life-threatening diseases (Table 47.3) that may present initially with isolated mouth findings.
PATHOPHYSIOLOGY
Oral lesions may result from localized or systemic pathophysiologic processes. Localized causes include congenital masses and cysts, infectious diseases, and oral tumors. Systemic illnesses with prominent oral involvement include a number of infectious, inflammatory, and toxin-mediated conditions. Given the broad spectrum of illnesses presenting with oral lesions, it is convenient to discuss individual causes under specific headings within the differential diagnosis. Several conditions with typical oral lesions exist that do not comfortably fit under any of these headings; these are discussed in the section on miscellaneous oral lesions.
DIFFERENTIAL DIAGNOSIS
Congenital Oral Lesions
Most oral lesions present at birth or in early infancy represent benign findings. Patients are largely asymptomatic, and the lesions resolve spontaneously.
Epstein pearls occur in more than 60% of newborns as small, white milia in the midline of the hard palate. These epithelial inclusion cysts are often found in clusters and resolve over the first few months of life. Epithelial pearls are similar to Epstein pearls and appear as shiny, small, white, self-limited lesions that occur on the gums.
Bohn nodules are also self-limited cysts that appear on the mandibular or maxillary dental ridges. Dental lamina cysts occur on the alveolar ridge of newborns and stem from trapped remnants of the dental lamina.
Natal teeth are prematurely erupted primary teeth present at birth; teeth erupting within the first month of life are termed neonatal teeth. These teeth are either supernumerary or true deciduous teeth and are usually found in the lower incisor region. Natal teeth may lead to ulcerations of the underside of the tongue, called Riga–Fede disease.
Patients with ankyloglossia may be referred to as “tongue tied” because of congenital shortening of the lingual frenum, which limits their ability to fully extend the tongue. Surgical correction is considered for patients when speech or feeding is affected.
Epulis is a congenital, fibrous, sarcomatous tumor that arises from the periosteum of the mandible or maxilla. The mass is firm and pedunculated and may regress spontaneously. Excision is required if the epulis interferes with feeding or breathing, or for cosmetic reasons.
Lymphangioma is a benign congenital tumor of lymphatic vessels that can appear on the tongue, lips, or buccal mucosa at birth or in early infancy. Hemangiomas are benign vascular malformations present at birth that may become more apparent as the patient grows. Oral hemangiomas are typically accompanied by vascular lesions internally and on the patient’s skin.
White sponge nevus is an autosomal-dominant condition presenting with white, raised, folded-appearing tissue most commonly found on buccal mucosa. It may be mistaken for candidiasis.
Infectious Oral Lesions
Infectious oral lesions are most commonly viral in origin but may be caused by bacterial or fungal infections as well (see Chapter 102 Infectious Disease Emergencies).
Candidiasis, or thrush, is white plaque on the buccal mucosa, gingivae, and palate that cannot be removed with gentle scraping. Caused by Candida albicans, thrush is common in neonates and infants. Thrush outside of infancy should prompt consideration of the patient’s immune status, as it is more common in patients infected with human immunodeficiency virus (HIV) or those who are otherwise immunosuppressed.
The typical lesions of herpes simplex virus (HSV) are groups of vesicles and erosions on erythematous bases in and around the mouth. Herpes gingivostomatitis, most commonly caused by HSV type 1 (HSV-1), represents primary infection and typically occurs in young children and infants. These patients have pain, fever, and drooling. Recurrent disease commonly manifests as herpes labialis or “cold sores.” This consists of painful lesions that occur on the lips, most often the lower lip. Herpes labialis may be triggered by an acute febrile illness, sun exposure, or stress.
Hand, foot, and mouth disease is characterized by discrete shallow erosions in the mouth, especially on the soft palate, erythematous papulovesicular lesions on the hands and feet, and often high fevers. It is generally caused by enteroviruses, particularly coxsackievirus, and is self-limited. Herpangina is a similar infection, commonly caused by group A coxsackievirus. It is characterized by pharyngeal vesicles as well as fever, muscle aches, and malaise. Treatment in both cases is supportive, with antipyretics, topical and systemic analgesics, and attention to hydration.
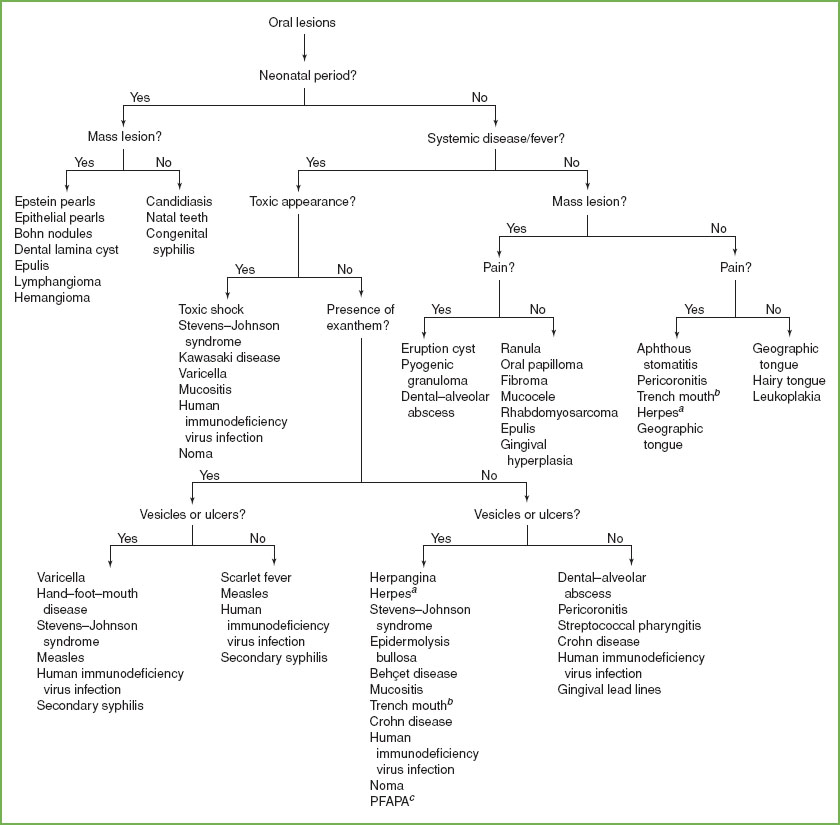
FIGURE 47.1 Oral lesions. aHerpes gingivostomatitis or labialis. bTrench mouth, acute necrotizing ulcerative gingivitis. cPFAPA, periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis syndrome.
Group A streptococcal pharyngitis can present with a characteristic “strawberry tongue,” the result of hypertrophic red papillae on a thick white coat. Posterior pharyngeal findings include tonsillar hyperemia, hypertrophy, and exudate, as well as palatal petechiae (Fig. 47.2). If a “sandpaper” papular rash on a blanching erythematous base is present, most commonly on the trunk, the condition is termed scarlet fever.
Koplik spots are pinpoint white macules on markedly erythematous mucous membranes, occurring during the prodrome of measles, which includes cough, coryza, conjunctivitis, and fever. They generally resolve before the characteristic rash occurs.
Varicella lesions occurring in the mouth result in painful vesicles, which may become unroofed, on an erythematous base. Patients may be reluctant to swallow because of pain. Unless secondary bacterial infection occurs, these lesions are self-limited.
Oral lesions will be the initial presenting sign in approximately half of children with perinatally acquired HIV infection. Common lesions include oral candidiasis, parotid enlargement, herpes simplex vesicles or erosions, hairy leukoplakia, aphthous ulcers, linear gingival erythema, and necrotizing ulcerative gingivitis. Blue, purple, or red macules, papules, or nodules on the palate suggest oral Kaposi sarcoma, whereas diffuse swelling, discrete nodules, or ulcers of any oral mucosal surface may indicate non-Hodgkin lymphoma, although both are rare in children. Highly active antiviral therapy decreases the prevalence of oral lesions; increasing lesions may indicate low CD4 percentage and advancing disease.
TABLE 47.1
DIFFERENTIAL DIAGNOSIS OF ORAL LESIONS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







