INTRODUCTION
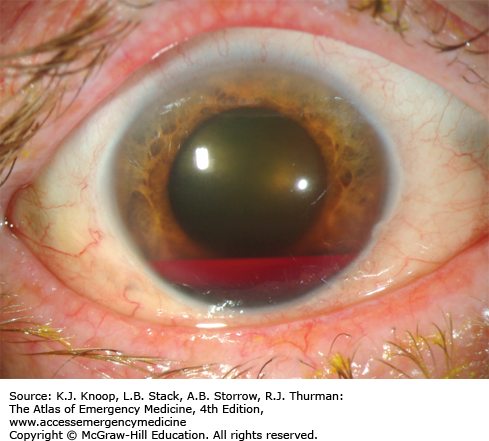
Corneal Perforation and Rust Ring. This patient was using a compressed air wire wheel brush when a wire came loose and lodged in the cornea. He was not wearing safety glasses. The wire was removed in the operating room where it was found to penetrate fully through the cornea and required one corneal suture. Interestingly, the rust ring had formed around the wire only about 3 hours after this injury occurred. (Used with permission from Brice Critser, CRA, The University of Iowa and EyeRounds.org.)
The authors acknowledge the special contributions of Dallas E. Peak and Carey D. Chisholm for contributions to prior editions.
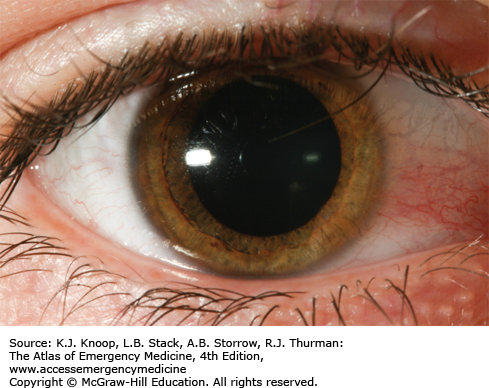
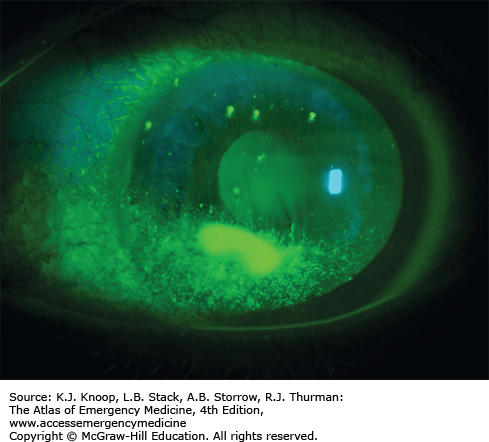
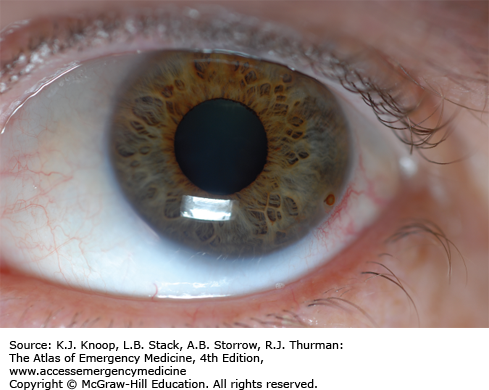
CORNEAL ABRASION
Corneal abrasions present with acute onset of eye discomfort, tearing, and often a foreign-body sensation. A “ciliary flush” (conjunctival injection hugging the limbus) may be seen. Large abrasions or those in the central visual axis may affect visual acuity. Photophobia and headache from ciliary muscle spasm may be present. Associated findings or complications include traumatic iritis, hypopyon, or a corneal ulcer. Fluorescein examination, preferably with a slit lamp, reveals the defect.
Instillation of topical anesthetic drops facilitates examination while relieving pain and blepharospasm. Consider using a short-acting cycloplegic (eg, cyclopentolate 1%, homatropine 5%) to reduce pain from ciliary spasm in patients who complain of headache or photophobia. Consider oral opioid analgesics for pain control. Nonsteroidal anti-inflammatory drug (NSAID) eye drops (eg, diclofenac or ketorolac) are equally effective and avoid risks of sedation. Neither treatment with topical antibiotics, nor patching, nor tetanus prophylaxis for uncomplicated corneal abrasions has scientific validation. Follow-up is advised for any patient with complications, or who is still symptomatic after 24 hours.
Mucus may simulate fluorescein uptake, but its position changes with blinking.
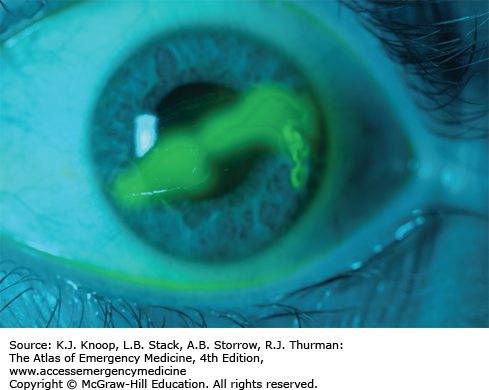
Multiple linear corneal abrasions, the “ice-rink sign,” may result from an embedded foreign body (FB) adhered to the upper lid. Always evert the lid to evaluate this.
Whenever the mechanism includes grinding or striking metal, or high-velocity injuries from mowers or string trimmers, maintain a high index of suspicion for penetrating injury. Fluorescein streaming away from an “abrasion” (Seidel test) may be an indication of a corneal perforation.
Routine prophylactic treatment with topical antibiotics remains controversial. When used, inexpensive, broad-spectrum antibiotic drops (sulfacetamide sodium or trimethoprim/polymyxin B) allow clearer vision than lubricating ointments, which may feel better, but blur vision. Avoid topical neomycin antibiotics because of a high risk of irritant allergy symptoms in many people.
An “abrasion” in a contact lens wearer should alert one to suspect a corneal ulcer. Consult ophthalmology while the patient is in the emergency department.
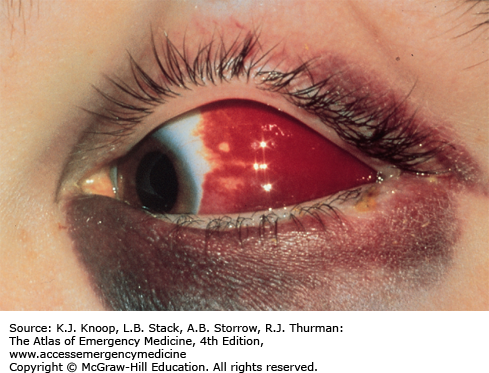
SUBCONJUNCTIVAL HEMORRHAGE
A subconjunctival hemorrhage or hematoma occurs with often trivial events such as a cough, sneeze, Valsalva maneuver, or minor blunt trauma. The patient may present with some degree of duress secondary to the appearance of the bloody eye. The blood is usually bright red and appears flat. It is limited to the bulbar conjunctiva and stops abruptly at the limbus. This appearance is important to differentiate the lesion from bloody chemosis, which can occur with scleral rupture or nontraumatic conditions. Aside from appearance, this condition does not cause the patient any pain or diminution in visual acuity.
No treatment is required. Instruct the patient to expect the blood to resorb in 2 to 3 weeks.
Subconjunctival hematoma differs from bloody chemosis with the flat appearance of the conjunctival membranes.
A subconjunctival hematoma involving the extreme lateral globe after blunt trauma is very suspicious for zygomatic arch fracture.
Evaluate patients with nontraumatic bloody chemosis for an underlying metabolic (coagulopathy) or structural (cavernous sinus thrombosis) disorder.
CORNEAL FOREIGN BODY
Patients typically report getting something in the eye or complain of FB sensation. FBs that overlie the cornea may affect vision. Tearing, conjunctival injection, headache, and photophobia may also be present. The most important consideration is the possibility of a penetrating globe injury. One must elicit a meticulous history about the mechanism of injury.
Topical anesthetic drops (eg, 0.5% proparacaine or tetracaine) facilitate examination and removal. If superficial, removal with saline flush may be attempted before using a sterile eye spud or small (25-gauge) needle. Consider topical antibiotic drops or ointment for the residual corneal abrasion. Tetanus prophylaxis is indicated. A “short-acting” cycloplegic (eg, cyclopentolate 1% or homatropine 5%) may benefit patients with headache or photophobia. FB or “rust ring” removal should be conducted using slit-lamp microscopy, only by a physician skilled in rust ring removal due to the risk of corneal perforation or scarring.
Always evert the upper lid and search carefully for an FB. An FB adherent to the upper lid abrades the cornea, producing the “ice-rink” sign, caused from multiple linear abrasions.
Vigorous attempts to remove the entire rust ring are not warranted. This may await emergency department or ophthalmology follow-up in 24 hours.
Use of cotton-tipped applicators to attempt FB removal should be discouraged (large surface area and potential to cause a larger corneal defect).
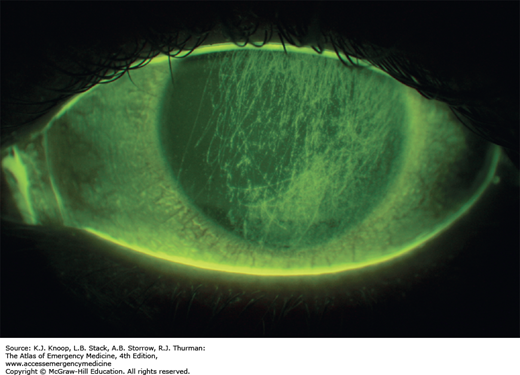
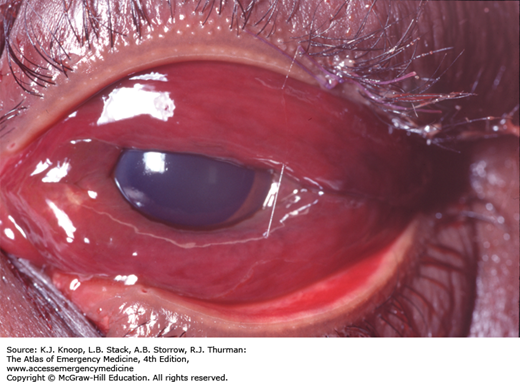
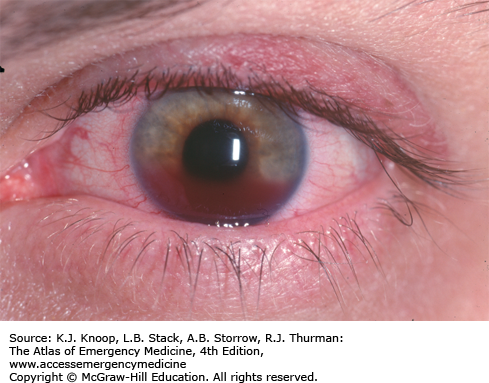
HYPHEMA
Injury to the anterior chamber that disrupts the vasculature supporting the iris or ciliary body results in a hyphema. The blood tends to layer with time, and if left undisturbed, gravity will form a visible meniscus. Symptoms can include pain, photophobia, and possibly blurred vision secondary to obstructing blood cells. Nausea and vomiting may signal a rise in intraocular pressure (glaucoma) caused by blood cells clogging the trabecular meshwork.
Prevention of further hemorrhage is the foremost treatment goal. Most rebleeding occurs within the first 72 hours and is usually more extensive than the initial event. Keep the patient at rest in the supine position with the head elevated slightly. Use a hard eye shield to prevent further trauma from manipulation. Avoid oral or parenteral pain medication and sedatives with antiplatelet activity such as NSAIDs. Use antiemetics if the patient has nausea. Further treatment at the discretion of specialty consultants may include topical and oral steroids, antifibrinolytics such as aminocaproic acid, or surgery. Measure intraocular pressure (IOP) unless there is a suspicion of penetrating injury to the globe. Treat elevated IOP with appropriate agents, including topical β-blockers, pilocarpine, and, if needed, osmotic agents (mannitol, sorbitol) and acetazolamide. Ophthalmologic consultation is warranted to determine local admission practices.
Instruct patients specifically not to read or watch television, as these activities result in greater than usual ocular activity.
Rebleeding may occur in 10% to 20% of patients, most commonly in the first 2 to 5 days when the blood clots start to retract.
An “eight-ball” or total hyphema often leads to elevated IOP and corneal bloodstaining, and typically requires surgical evacuation.
Patients with sickle cell and other hemoglobinopathies are at risk for sickling of blood inside the anterior chamber. This can cause a rise in IOP caused by obstruction of the trabecular meshwork even if only a small hyphema is present.
An abnormally low IOP should prompt consideration for presence of penetrating globe injury.
Evaluate supine trauma patients for slight differences in iris color to determine the presence of a hyphema.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree