AIRWAY/DENTAL COMPLICATIONS
Airway Complications
Incidence
• Unknown owing to varying significance/detection of injuries
• Minor trauma to larynx & pharynx may be as common as 6%
• Damage typically ↑ in relation to duration of intubation (many injuries result from placement of endotracheal tube)
• Many injuries occur during routine, “easy” intubations
• Delayed, chronic complications often present weeks to even months after extubation, particularly with prolonged intubations (>5 d)
Risk Factors for Intubation Trauma
• Difficult, traumatic, multiple attempts at intubation
• Laryngeal abnormalities (past trauma, inflammatory conditions, infection)
• Movement of endotracheal tube (tube manipulation/surgical repositioning, coughing/bucking)
• Impaired clearance of secretions
• Gastroesophageal reflux
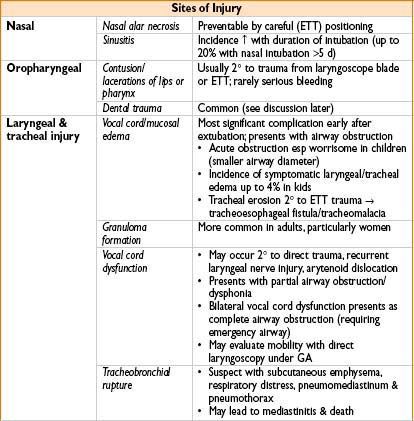
Prevention
• Use small ETTs with lowest possible cuff pressures (leak <30 cm in pediatric pts)
• Limit use of adjuncts (such as intubating stylets)
• Wean ventilator to minimize duration of intubation
• Treat airway infections aggressively & early
• Minimize aspiration risk (when risk factors present)
• Perform detailed assessment to prevent unanticipated airway difficulty (to ↓ chance of otherwise preventable airway injury)
• Prepare alternative plans if intubation fails
• Discuss risk of airway injury with pts preop (shown to ↓ litigation)
Management
• Acute airway edema/stridor: Nebulized racemic epinephrine; dexamethasone controversial
• Prolonged intubation (>5 d): Consider laryngeal evaluation to evaluate for injury
• Chronic injury from repeated/prolonged intubation: Surgical correction may be required
• Tracheobronchial rupture: Emergent surgical correction
Obtain follow-up if concerned about airway trauma
• Inform pts if airway management was difficult/nonstandard
Dental Injuries
• Dental trauma: Most common permanent airway injury & leading source of malpractice claims (30–40%)
• Injuries: Fractured teeth, displaced restorations, subluxation, & avulsion (upper incisors most commonly affected secondary to use as fulcrum for laryngoscope)
Deciduous tooth loss → can result in problems with permanent teeth
• Adverse outcomes → related to aspiration of teeth/restorations
Incidence
• Overall incidence: Reports range from 0.02–12% (75% of injuries occur during intubation)
• Injuries can occur during maintenance (poorly positioned airway, bite block, masseter spasm during wakeup)
Risk Factors
• Tracheal intubation; poor dentition/periodontal disease; difficult airway characteristics; past dental restoration/endodontic treatment; elderly pts; brittle enamel; loose deciduous teeth; inexperienced laryngoscopist
Prevention
• Detailed preop history & examination:
→ Caries/loose teeth, prostheses, past dental work
→ Assess mouth opening
→ Evaluate dentition, evidence of periodontal disease, tooth hypermobility
→ Document preexisting conditions (reduces litigation if damage occurs)
• Consider tooth protection
→ Protectors (prefabricated rubber/custom-made by dentist)
Management
• Loosened tooth
Return to original position promptly; splint with tape/suture
• Displaced fragment of tooth/restoration:
Locate & recover all pieces; consider radiographs (chest, lateral head & neck) to exclude passage through glottis
• Avulsed tooth
Immediately replace tooth to original position
Avoid wiping or drying root surface
Splint temporarily with tape/suture
If aspiration concern prevents immediate reimplantation
→ carefully place tooth in suitable medium (saline/milk)
Immediate dental referral, injury documentation & discussion with pt important
• Most hospitals require filing an incident report
• Reimbursement responsibility depends on hospital policy
Burns
Intraoperative burns are rare; can be devastating/fatal
Surgical Fire
• 200 surgical fires per year in the United States
• Fire requires O2, flammable materials, & ignition source
→ O2 commonly administered in OR (endotracheal, nasal cannula)
→ Flammable materials = surgical drapes, alcohol prep solutions, plastic ETTs
→ Ignition sources = laser, electrosurgical units (ESUs), cautery
• Head & neck surgeries represent most cases involving fire in OR
→ Higher risk since nasal cannulas + laser/electrocautery → combustion
→ ETT carrying enriched O2 can also ignite, leading to a “blowtorch” effect during positive-pressure ventilation
Airway Fire
• Prevention: Decrease FiO2 during lasering; Use heliox; Use fire resistant ETTs; Wrap ETT in metal tape; Fill ETT cuff with saline, not air
• Management: Remove ETT/stop ventilation, discontinue O2, douse fire with saline/water, mask-ventilate pt; Perform bronchoscopy to assess airway damage
Electrocautery/Electrosurgical Unit
• Current path: Electrosurgical pencil → through pt → out grounding pad
• Current density dissipated over large surface area → limits risk of burn (because of low impedance return electrode)
• ESU-associated burns:
→ Improper placement of return electrode (↓ contact surface area)
→ Fluids (blood, irrigation, skin prep) cause improper electrode contact
→ Avoid placement of return electrode over bony prominences
→ ESUs can serve as ignition source (esp if ↑ O2 conc in use)
Magnetic Resonance Imaging
• Complications usually involve metallic objects flying into magnetic field & burns
• MRI radio frequency can cause heating of current conducting materials:
→ ECG cables & electrodes
Remove excess cables & avoid cable contact with skin
Do not loop cables, ensure that ECG electrodes are firmly attached
→ Medicated patches
Some contain aluminized backing (can heat in MRI)
Avoid testosterone, nitro, nicotine, scopolamine, clonidine patches
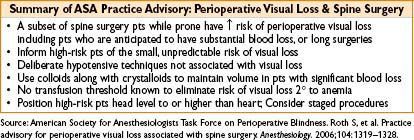
Perioperative Blindness
< div class='tao-gold-member'>









