Chapter 27 Ocular Emergencies
Determining Visual Acuity
• Determine visual acuity before manual eye examination because manipulation increases blurring and decreases visual acuity.
• Consider instilling a topical anesthetic agent before examination to facilitate obtaining visual acuity.
• Measure visual acuity with and without corrective lenses.
• If the patient is unable to see the Snellen chart, assess visual acuity by walking toward the patient holding up several fingers. Stop walking when the patient is able to tell how many fingers are being held up. Document the number of fingers and the distance from the patient (e.g., “three fingers at 15 feet”). Near-vision cards are also available for nonambulatory patients.
Conjunctivitis (Pink Eye)
Acute conjunctivitis is an infection of the conjunctiva, the membrane that lines the eyelid and sclera. Causes of conjunctivitis include bacterial, viral, and fungal infections and allergic and chemical irritation.1
Therapeutic Interventions
• Antibiotic ophthalmic drops or ointment for bacterial infections.
• Cool compresses and decongestants for allergic conjunctivitis.
• If conjunctivitis is gonococcal, consider that the patient may also have chlamydial conjunctivitis; systemic therapy and appropriate referrals will also be needed.
• Treat chemical conjunctivitis as a chemical burn with immediate eye irrigation.
Patient Education
• Bacterial and viral conjunctivitis are highly contagious; teach the following infection control measures:
• Warm soaks may help to gently remove crusted exudates from eyelids and lashes after sleep.
• Cool compresses can be applied to eyelids for comfort and to decrease swelling.
• Wear sunglasses to decrease photophobia.
• Do not wear contact lenses or eye makeup until symptoms have resolved.
• Follow up with health care provider or ophthalmologist in 2 to 3 days.
How to Instill Ophthalmic Medications
Ophthalmic Drops
1. Explain the procedure to the patient.
2. Pull the lower eyelid down.
4. Instill one or two drops of solution into the cul-de-sac (the center of the lower lid).
5. Have the patient blink gently to distribute the solution.
6. Instruct the patient not to squeeze the eyelids shut tightly; this will cause the solution to leak out.
Ophthalmic Ointment
Infections of the Eyelids and Cornea
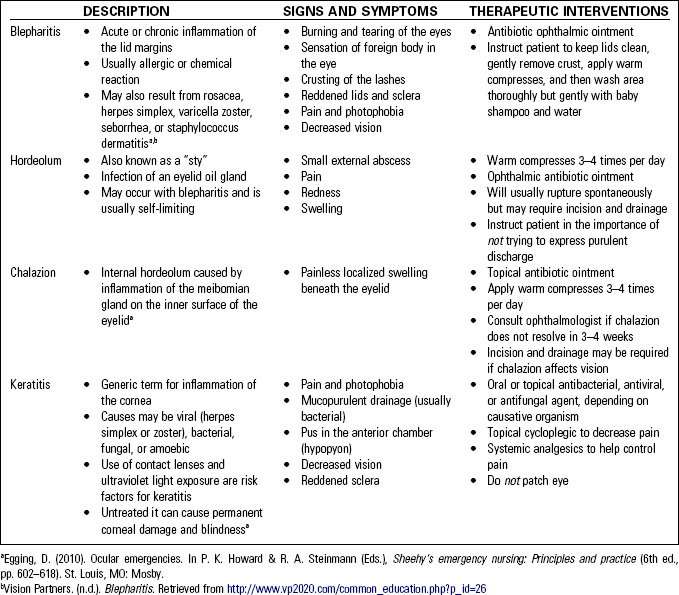
Infections of the eyelids (i.e., blepharitis, hordeolum, chalazion) or the cornea (keratitis) are not uncommon complaints of patients presenting to the emergency department. The most likely causative pathogen for these infections is Staphylococcus aureus. Table 27-1 summarizes the signs and symptoms and therapeutic interventions for these ocular infections.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree