![]() Occipital neuralgia is neuropathic pain that is classically described as a persistent dull pain at the base of the skull with intermittent, sudden shocklike pain or paresthesias radiating from the back of the head over the scalp to behind the eyes. The pain follows the distribution of the greater occipital nerve (GON) and the lesser occipital nerve (LON).1
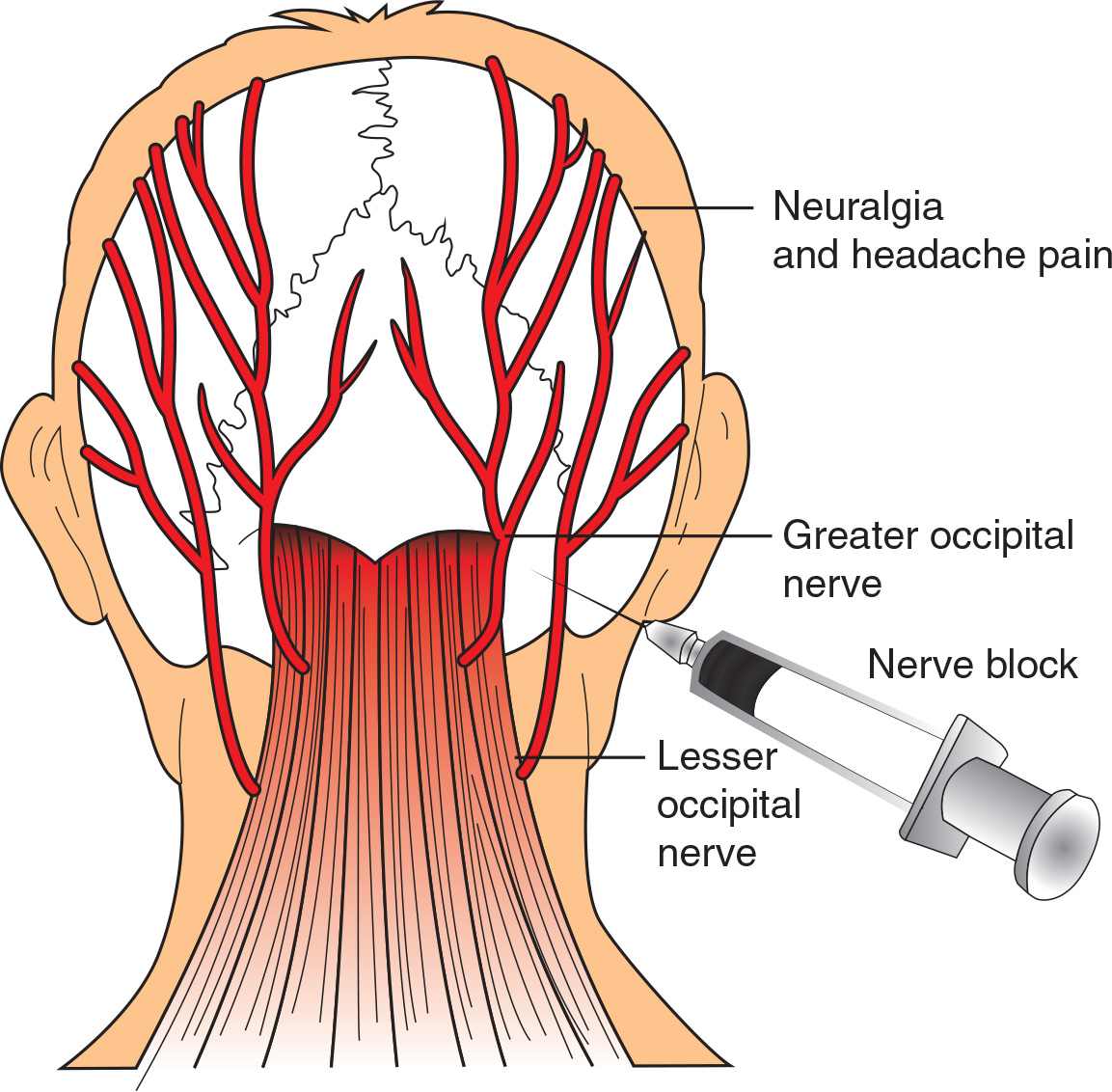
Occipital neuralgia is neuropathic pain that is classically described as a persistent dull pain at the base of the skull with intermittent, sudden shocklike pain or paresthesias radiating from the back of the head over the scalp to behind the eyes. The pain follows the distribution of the greater occipital nerve (GON) and the lesser occipital nerve (LON).1
![]() Thought to be from irritation or trauma to the GON and LON. Possible causes include muscle entrapment of the nerves, inflammation or repetitive microtrauma from hyperextension of the neck (i.e., computer monitors with a focal point too high).
Thought to be from irritation or trauma to the GON and LON. Possible causes include muscle entrapment of the nerves, inflammation or repetitive microtrauma from hyperextension of the neck (i.e., computer monitors with a focal point too high).
![]() Usually unilateral
Usually unilateral
![]() Tenderness over the nerve is associated with a positive response to occipital nerve block (ONB) injections2
Tenderness over the nerve is associated with a positive response to occipital nerve block (ONB) injections2
![]() Indicated only if a history and physical examination do not suggest potential intracranial processes
Indicated only if a history and physical examination do not suggest potential intracranial processes
INDICATIONS
![]() ONBs are traditionally used for the treatment of headache associated with occipital neuralgia3
ONBs are traditionally used for the treatment of headache associated with occipital neuralgia3
![]() Although not typically used as treatment in emergency medicine, studies have found ONBs to be effective in the treatment of migraine,4 cluster,5 and cervicogenic6 headaches
Although not typically used as treatment in emergency medicine, studies have found ONBs to be effective in the treatment of migraine,4 cluster,5 and cervicogenic6 headaches
CONTRAINDICATIONS
![]() Allergy to analgesic compounds or steroids
Allergy to analgesic compounds or steroids
![]() Lack of a clear-cut diagnosis
Lack of a clear-cut diagnosis
![]() Suspected intracranial process or focal neurologic deficits on examination
Suspected intracranial process or focal neurologic deficits on examination
LANDMARKS
![]() The GON arises from the C2 nerve root and becomes superficial medial to the palpated occipital artery at the level of the superior nuchal line. It runs laterally to the external occipital protuberance and medially to the mastoid process.
The GON arises from the C2 nerve root and becomes superficial medial to the palpated occipital artery at the level of the superior nuchal line. It runs laterally to the external occipital protuberance and medially to the mastoid process.
![]() The occipital artery can be palpated one-third of the way from the inion to the mastoid process
The occipital artery can be palpated one-third of the way from the inion to the mastoid process
![]() The LON arises from the cervical plexus. It becomes superficial at the inferior nuchal line.
The LON arises from the cervical plexus. It becomes superficial at the inferior nuchal line.
![]() The GON perforates the semispinalis capitis and trapezius muscles. One study found that the GON emerges from the semispinalis approximately 3.0 cm inferior to the occipital protuberance and 1.5 cm lateral to midline.7
The GON perforates the semispinalis capitis and trapezius muscles. One study found that the GON emerges from the semispinalis approximately 3.0 cm inferior to the occipital protuberance and 1.5 cm lateral to midline.7
SUPPLIES
![]() Antiseptic solution
Antiseptic solution
![]() Local anesthetic (i.e., 1% lidocaine, 4 mL, and 0.25% bupivacaine, 4 mL)
Local anesthetic (i.e., 1% lidocaine, 4 mL, and 0.25% bupivacaine, 4 mL)
![]() Injectable steroids (i.e., methylprednisolone, betamethasone, or triamcinolone)
Injectable steroids (i.e., methylprednisolone, betamethasone, or triamcinolone)
![]() 25- or 27-gauge 1.5-inch needle, 12-mL sterile syringe
25- or 27-gauge 1.5-inch needle, 12-mL sterile syringe
TECHNIQUE
![]() Preparation
Preparation
![]() In a 12-mL sterile syringe, draw up a total of 8 mL of local anesthetic and 80 mg of methylprednisolone for a first time block or 40 mg of methylprednisolone for a repeat block
In a 12-mL sterile syringe, draw up a total of 8 mL of local anesthetic and 80 mg of methylprednisolone for a first time block or 40 mg of methylprednisolone for a repeat block
![]() Commonly used anesthetic agents include a mixture of 4 mL of a quick-acting local anesthetic for immediate results, such as 1% lidocaine, with 4 mL of a longer-acting local anesthetic, such as 0.25% bupivacaine
Commonly used anesthetic agents include a mixture of 4 mL of a quick-acting local anesthetic for immediate results, such as 1% lidocaine, with 4 mL of a longer-acting local anesthetic, such as 0.25% bupivacaine
![]() Injectable steroids include methylprednisolone, triamcinolone, or betamethasone (FIGURE 48.1)
Injectable steroids include methylprednisolone, triamcinolone, or betamethasone (FIGURE 48.1)
![]() Place the patient in a sitting position, leaning forward, with the forehead resting on a padded bedside table with the neck in a flexed position
Place the patient in a sitting position, leaning forward, with the forehead resting on a padded bedside table with the neck in a flexed position
![]() Prepare the skin/hair with an antiseptic solution
Prepare the skin/hair with an antiseptic solution
![]() Anesthetize the superficial skin of the injection site with a small wheal of lidocaine
Anesthetize the superficial skin of the injection site with a small wheal of lidocaine
![]() Distal Injection Technique
Distal Injection Technique
![]() This classic technique injects the GON at the level of the superior nuchal line, a region with no muscle. This is the suggested approach.
This classic technique injects the GON at the level of the superior nuchal line, a region with no muscle. This is the suggested approach.
![]() Palpate the occipital artery one-third of the way from the inion to the mastoid process. Using a 25- or 27-gauge 1.5-inch needle, aim just medial to the occipital artery at the level of the superior nuchal line.
Palpate the occipital artery one-third of the way from the inion to the mastoid process. Using a 25- or 27-gauge 1.5-inch needle, aim just medial to the occipital artery at the level of the superior nuchal line.
![]() Advance the needle perpendicularly until the needle touches the skull or until a paresthesia is elicited (the patient should be warned of this prior to starting). Withdraw the needle approximately 2 to 4 mm and redirect superiorly.
Advance the needle perpendicularly until the needle touches the skull or until a paresthesia is elicited (the patient should be warned of this prior to starting). Withdraw the needle approximately 2 to 4 mm and redirect superiorly.
![]() After gentle aspiration to confirm that the needle is not in a vessel, 5 mL of the solution should be injected in a fanlike distribution. (Note: The solution should inject easily; resistance to injection is a sign of inappropriate needle positioning.)
After gentle aspiration to confirm that the needle is not in a vessel, 5 mL of the solution should be injected in a fanlike distribution. (Note: The solution should inject easily; resistance to injection is a sign of inappropriate needle positioning.)
![]() Further block of the LON and several superficial branches of the GON can be achieved by directing the needle laterally and slightly inferior with injection of an additional 4 mL of solution, after gentle aspiration
Further block of the LON and several superficial branches of the GON can be achieved by directing the needle laterally and slightly inferior with injection of an additional 4 mL of solution, after gentle aspiration
![]() Massage/compress the injected area to distribute the anesthetic and to minimize hematoma formation
Massage/compress the injected area to distribute the anesthetic and to minimize hematoma formation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree