HAND INFECTIONS
The most common pathogens causing hand infection are Staphylococcus aureus, Streptococcus species, and gram-negative species.1 Polymicrobial infections are common, especially with inoculation of mouth flora. In most U.S. cities, community-associated methicillin-resistant Staphylococcus aureus is the most common pathogen cultured from patients with skin and soft tissue infections in EDs,2 including 47% to 78% of hand infections.3,4,5,6,7,8
Injection drug users typically present with abscesses or deep space infections secondary to S. aureus and gram-negative organisms.9 These infections are most commonly caused by direct introduction, but hematogenous spread from bacterial endocarditis is a possibility (see chapter 296, “Injection Drug Users”).
Hand infections are also discussed in chapter 46, “Puncture Wounds and Bites.”
Paronychia and felons are caused by minor trauma like chewing fingernails or exposing minor injuries to saliva. Most of these infections are polymicrobial including anaerobic bacteria.
Infections caused by animal bites reflect the oral flora of the involved species. Bites introduce a broad range of bacteria, including gram-positive, anaerobic, and gram-negative organisms. Common pathogens include streptococci, staphylococci, Haemophilus, Eikenella, Fusobacterium, peptostreptococci, Prevotella, and Porphyromonas species.10 Cat and dog bites harbor Pasteurella multocida, which typically produces an aggressive, rapidly spreading cellulitis that becomes suppurative. (See chapter 46.)
Patients with diabetes or acquired immunodeficiency syndrome have common bacterial infection or develop atypical infections, including those caused by Mycobacterium or Candida albicans. Those who are immunocompromised or asplenic are at risk for rapid progression and require prompt source control and antibiotics.
Hand infections are most commonly introduced by an injury to the dermis. The infection initially may remain superficial and broader, termed cellulitis, or be localized as seen in a paronychia or felon. Left untreated, infections may spread along anatomic planes or to adjacent compartments in the hand. Deeper injuries may directly seed underlying structures, creating rapidly spreading infections such as those seen with closed fist injuries or cat bites.
Obtain a directed history to delineate a likely cause of the infection. The physical examination should note the anatomic limits of the infection. Look for skin, subcutaneous tissue, fascial space, tendon, joint, or bone involvement. If deep structures of the hand are involved, emergently consult a hand specialist because treatment likely will involve inpatient care and operative drainage.
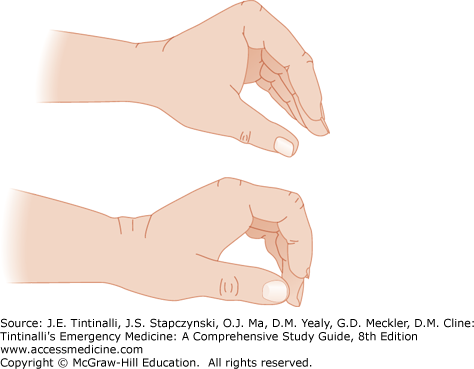
With the exception of superficial cellulitis, hand infections are managed using basic principles. First, incise and drain any collection of pus. Superficial and discrete infections, such as paronychia and felons, can be drained in the ED. Deep infections are better treated in the operating room by a hand surgeon. Second, immobilize and elevate the extremity. This will rest the hand, reduce inflammation, avoid secondary injury, and limit extension of the infection. Immobilize by applying a bulky hand dressing and splinting the hand in a position of function: the wrist at 15 to 30 degrees of extension, the metacarpophalangeal joints at 50 to 90 degrees of flexion, and the interphalangeal joints at 5 to 15 degrees of flexion (Figure 283-1). Elevate the hand on pillows or suspended using stockinet. Third, use broad-spectrum antibiotics initially targeting possible common and serious bacteria, altering only based on response and culture results (Table 283-1). Fourth, if the patient is not admitted to the hospital, ensure reexamination within 48 hours.
| Infection | Initial Antimicrobial Agent(s) | Likely Organisms | Comments |
|---|---|---|---|
| Cellulitis | For mild to moderate cellulitis: TMP-SMX double strength, 1–2 tablets twice per day PO for 7–10 d.* Plus/minus cephalexin, 500 milligrams PO four times per day for 7–10 d, or dicloxacillin, 500 milligrams PO four times daily for 7–10 d. For severe cellulitis: Vancomycin, 1 gram IV every 12 h. | Staphylococcus aureus (MRSA) Streptococcus pyogenes | Clindamycin is an option, but increasing MRSA resistance to clindamycin has been reported. Consider vancomycin for injection drug abusers. |
| Felon/paronychia | TMP-SMX double strength, 1–2 tablets twice per day PO for 7–10 d.* Plus/minus cephalexin, 500 milligrams PO four times per day for 7–10 d,*or dicloxacillin, 500 milligrams PO four times daily for 7–10 d.* Consider addition of clindamycin or amoxicillin-clavulanate to TMP-SMX (rather than cephalexin) if anaerobic bacteria are suspected. | S. aureus (MRSA), S. pyogenes, anaerobes, polymicrobial | Antibiotics indicated for infections with associated localized cellulitis, otherwise drainage alone may be sufficient, culture recommended by hand surgeons.4,5,6,7 |
| Flexor tenosynovitis | Ampicillin-sulbactam, 1.5 grams IV every 6 h, or cefoxitin, 2 grams IV every 8 h, or piperacillin-tazobactam, 3.375 grams IV every 6 h. Plus: vancomycin, 1 gram IV every 12 h, if MRSA is prevalent in community. | S. aureus, streptococci, anaerobes, gram negatives | Parenteral antibiotics are indicated; consider ceftriaxone for suspected Neisseria gonorrhoeae. |
| Deep space infection | Ampicillin-sulbactam, 1.5 grams IV every 6 h, or cefoxitin, 2 grams IV every 8 h, or piperacillin-tazobactam, 3.375 grams IV every 6 h. Plus: vancomycin, 1 gram IV every 12 h, if MRSA is prevalent in community. | S. aureus, streptococci, anaerobes, gram negatives | Inpatient management. |
| Animal bites (including human) | If no visible signs of infection: amoxicillin/clavulanate, 875/125 milligrams PO twice daily for 5 d. For signs of infection: ampicillin-sulbactam, 1.5 grams IV every 6 h, or cefoxitin, 2 grams IV every 8 h, or piperacillin-tazobactam, 3.375 grams every 6 h. For penicillin allergy, use clindamycin plus moxifloxacin or TMP-SMX and metronidazole. | S. aureus, streptococci, Eikenella corrodens (human), Pasteurella multocida (cat), anaerobes, and gram-negative bacteria | All animal bite wounds should receive prophylactic oral antibiotics. |
| Herpetic whitlow | Acyclovir, 400 milligrams PO three times daily for 10 d. | Herpes simplex | No surgical drainage is indicated. |
Empiric treatment for these infections is based on local antibiotic resistance patterns, using trimethoprim-sulfamethoxazole, doxycycline or minocycline (outpatient), or vancomycin or linezolid (inpatient) for methicillin-resistant S. aureus infections.11 In some communities, clindamycin is effective,11 whereas in other communities, fluoroquinolones are effective.6
Cellulitis is the most superficial of hand infections and is treated with oral antibiotics absent widespread or systemic signs. Diagnosis is made by documenting erythema, warmth, and edema in the affected portion of the hand without any involvement of deeper structures in the hand. Specifically, range of motion of the digits, hand, or wrist should not be painful, and palpation of the deeper structures of the hand should not produce any tenderness.
The most common offending organisms are S. aureus (predominately methicillin-resistant)1,2,3,4,5,6,7,8 and Streptococcus pyogenes. Initial treatment is in Table 283-1. Methicillin-resistant S. aureus infections are more common in patients with diabetes mellitus, immunocompromised patients, intravenous drug users, prisoners, and the homeless.3,4 Given the increasing rates of methicillin-resistant S. aureus and difficulty distinguishing among the types of S. aureus cellulitis, routine empiric treatment of methicillin-resistant S. aureus should be considered. In addition, choose an agent active against streptococci.10 Empiric monotherapy with trimethoprim-sulfamethoxazole or other methicillin-resistant S. aureus–targeted antibiotic is not recommended given the limited published efficacy data and concerns about effectiveness against streptococci.10,12 For more extensive involvement, start parenteral antibiotics, admit, and consult a hand surgeon. Consider admission for the immunocompromised, those with clinical toxicity, and those with rapidly spreading infections.
Hand infections following injuries from handling fish require different antibiotics and admission to the hospital. Infecting organisms include Vibrio vulnificus, Klebsiella pneumoniae, Streptococcus group A, S. aureus, and Enterobacter species.13 Antibiotic coverage with ceftazidime and doxycycline was successful in a large case series of patients.13
For all cases of cellulitis, immobilize the hand in a position of function, and make sure the patient keeps the hand elevated as much as possible. Remove digit rings and give tetanus prophylaxis as needed. Finally, for those discharged, arrange reexamination within 48 hours.
Flexor tenosynovitis is a surgical emergency. Failure to accurately diagnose and manage flexor tenosynovitis may result in adhesions, tendon vascular compromise and necrosis, or extension into adjoining deep spaces. This can lead to loss of function of the digit and eventually loss of function of the entire hand. The diagnosis is supported by the presence of the classic clinical signs described by Kanavel1; however, all four signs may not be present early in the course of infection (Table 283-2).
| Percussion tenderness | Tenderness over the entire length of the flexor tendon sheath |
| Uniform swelling | Symmetric finger swelling along the length of the tendon sheath |
| Intense pain | Intense pain with passive extension |
| Flexion posture | Flexed posture of the involved digit at rest to minimize pain |
The infection usually is associated with penetrating trauma of the affected area, although the patient may be unaware of injury. Staphylococcus is the most common bacterium isolated; however, infections often harbor anaerobes or are polymicrobial. Suspect disseminated Neisseria gonorrhoeae in a patient with a recent history consistent with a sexually transmitted infection (see chapter 149, “Sexually Transmitted Infections”).
Initiate treatment with parenteral antibiotics because the infection can spread rapidly through deep fascial spaces (Table 283-1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree