The pituitary.
Lesions of the pituitary
Mass lesions are usually primary adenomas of the anterior pituitary and stalk that may be secretory or non-secretory, and are either large enough to cause a mass effect, or small and only significant on account of their secretory activity. Patients with pituitary tumours may therefore have: hyposecretion of one of more hormones, disease resulting from isolated pituitary hormone over-secretion, hypersecretion of one hormone with deficient secretion of others, mass effect (compression of the optic chiasm), headache, possibly accompanied by hydrocephalus (rare), with or without hormonal pathology.
All anterior pituitary hormones except prolactin are under positive feedback control from the hypothalamus. Compression of the pituitary stalk may reduce dopamine transit to the anterior pituitary gland and results in mild hyperprolactinaemia (<2000 mIU/L).
Disruption of the posterior pituitary may result in diabetes insipidus, due to the lack of ADH and reduced water resorption in the distal tubule and collecting ducts, characterized by hypernatraemia, with inappropriately dilute urine.
Apoplexy (haemorrhagic infarction) is a rare event resulting from bleeding into the pituitary fossa, in the presence of a pre-existing adenoma, causing sudden onset of mass effect and hormonal dysfunction.
Classical presentation is with acute severe retro-orbital headache. Pituitary swelling can cause compression of adjacent structures, resulting in visual field lesions, opthalmoplegia and cerebral hypoperfusion. It is a serious condition and if left untreated may be fatal.
Risk factors include anticoagulation, coagulopathy, treatment with dopamine agonists (e.g. bromocriptine) and pregnancy. Differential diagnoses include: sub-arachnoid haemorrhage, acute ischaemic stroke (AIS), Sheehan’s syndrome or reversible cerebral vasoconstriction syndrome (RCVS), a rare condition presenting with recurrent severe headaches that can progress to intracranial haemorrhage or ischaemic stroke. It is more common post partum.
Investigation: CT Head is more easily organized in the emergency setting and requires the use of iodine-based contrast. MRI is more detailed than CT and requires the use of gadolinium contrast.
Treatment: Any patient with suspected apoplexy requires emergency neurosurgical referral and specialist endocrinology advice. Co-located obstetrics/neurosurgery care will be essential. Urgent hormonal replacement will be necessary (initially hydrocortisone).
Sheehan’s syndrome results from haemorrhage into the pituitary gland in the peripartum period. It may present with headache, but classically presents with insidious onset of panhypopituitarism some weeks following delivery. Mass effect is uncommon. It is more common in parturients with delivery blood loss >2000 mL. Incidence is reported as 1–2% following large postpartum haemorrhage.
Investigation and management: Brain imaging by CT/MR is necessary. Involvement of an endocrinologist is necessary when the diagnosis is suspected.
Lymphocytic hypophysitis is a benign self-limiting autoimmune inflammatory disease, usually related to pregnancy. Treatment (under the guidance of endocrinology) is usually with steroids alone.
Cerebrospinal fluid
Hydrocephalus
Hydrocephalus is due to an increase in CSF volume within the cranial ventricular system, resulting in ventriculomegaly and (usually) raised intracranial pressure (ICP). See Figure 22.2.
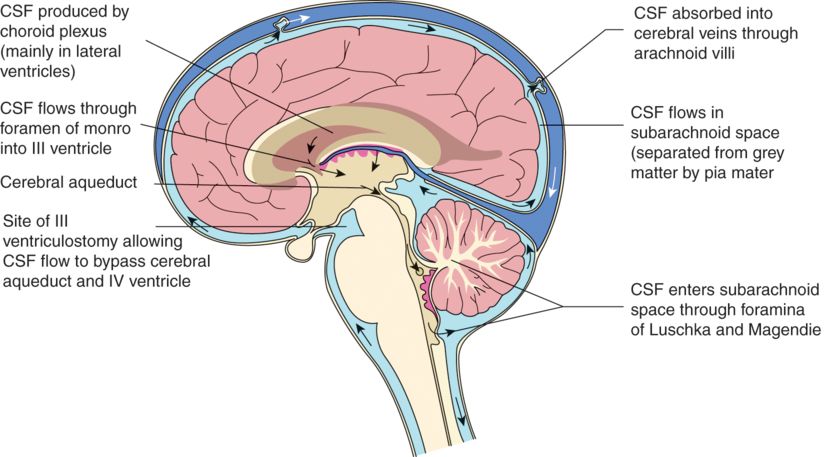
Cerebrospinal fluid production and flow.
Presentation is dependent upon the rate of CSF build up. Chronic impairment of flow results in headache, visual disturbance, confusion and ataxia with progression to decreased level of consciousness. Nausea and vomiting may exist. Acute cessation of CSF drainage results in rapid deterioration in conscious level. Those dependent upon non-anatomical drainage (shunts) are at risk of shunt blockage and acute hydrocephalus.
Non-communicating hydrocephalus occurs if CSF produced within the lateral ventricles fails to reach the sub-arachnoid space via drainage from the fourth ventricle. There is a CSFbrain:CSFspinal pressure gradient; lumbar drainage of CSF must be avoided as this can precipitate coning. Regional neuraxial anaesthesia is contraindicated. Causes include space-occupying lesions, haemorrhage (SAH, ICH) or CSF infection.
Communicating hydrocephalus occurs if CSF production exceeds reabsorption in the presence of normal anatomy. Causes include infection (meningitis, ventriculitis), haemorrhage, venous sinus thrombosis, following head injury or increased CSF protein content due to CNS tumour. Anatomically, neuraxial anaesthesia is not contraindicated.
Investigations
CT head confirms the diagnosis and may give indication as to the cause. See Figure 22.3. MRI will demonstrate increased ventricular size. T2-weighted images demonstrate periventricular oedema.
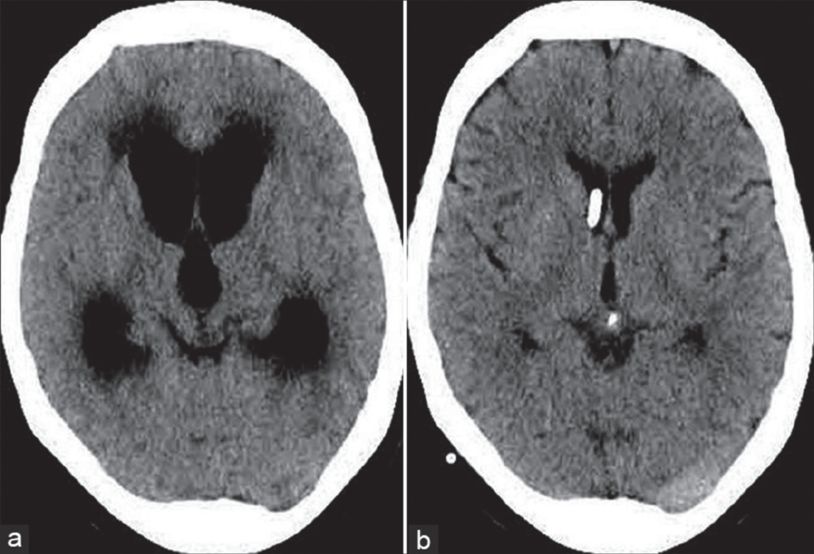
The two CT scan images demonstrate (a) dilated lateral venticles with a teardrop-shaped third ventricle and periventricular oedema. (b) An image of treated hydrocephalus with a ventricular drain in situ (this may be an EVD or ventriculo- shunt).
The presence of intracranial ventriculomegaly does not necessarily signify raised ICP; however, in symptomatic patients with headache and/or decreased level of consciousness, CSF flow obstruction must be assumed. Neurosurgical input is obligatory.
Treatment
Communicating hydrocephalus can be treated by CSF removal at lumbar puncture. For prolonged CSF pressure control, shunting of CSF is required (ventriculoperitoneal (VP)/atrial or lumboperitoneal (LP) shunt).
The standard emergency treatment of non-communicating hydrocephalus is with an externalized ventricular drain (EVD). Endoscopic third ventriculostomy (ETV) may be appropriate in some cases, with the aim to circumvent the aqueduct and VI ventricle by generating a fistula in the base of the III ventricle. See Figure 22.4. CSF flows directly to the basal cisterns. When successful, no additional CSF drainage procedure is necessary.
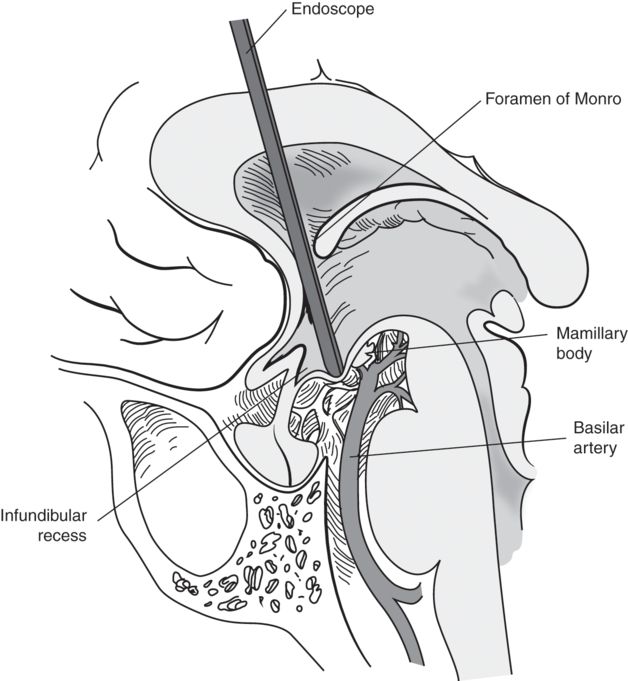
Endoscopic third ventriculostomy via a frontal burr hole through the base of the third ventricle.
Ventriculoperitoneal/atrial shunt creates a conduit from the ventricular system to either peritoneum or right atrium. The system contains a valve, both preventing back flow and also dictating the CSF drainage pressure. This provides a permanent artificial route for CSF drainage.
Key points regarding CSF shunts in pregnancy:
Parturients have a higher incidence of complicated pregnancy and worse fetal outcomes.
Shunt malfunction can occur during pregnancy, though is more likely in the peridelivery period.
Shunt blockage in a shunt-dependent parturient is a neurosurgical emergency.
CSF infection risk is increased. If suspected, neurosurgical guidance is necessary and investigation is classically diagnostic LP after CT head to confirm shunt function.
LP shunts are a relative contraindication for lumbar neuraxial blockade.
Parturients with functioning ETVs and no hydrocephalus can be treated as normal.
Benign intracranial hypertension (BIH)
BIH occurs mainly in women of childbearing age and is associated with raised BMI. It is thought to result from an abnormality in central venous sinus pressure. CSF pressure is raised, with normal-sized ventricles. It causes chronic headache and is associated with papilloedema. Acute deterioration may occur, threatening ocular function. Pregnancy and labour may precipitate deterioration. Signs and symptoms can mimic cerebral venous thrombosis (CVT). Exclusion of this diagnosis must be made in BIH patients with worsening headache or neurological signs.
Investigation
CT brain and orbit will demonstrate small ventricles. MR venogram is needed to exclude CVT. Visual fields need charting. CSF pressure monitoring is required (LP or parenchymal pressure monitor).
Treatment
Neurology/neurosurgery input is essential.
Therapeutic lumbar puncture can treat acute crises.
BIH is occasionally treated with lumboperitoneal shunt.
Labour and delivery have been successfully performed with epidural analgesia, lumbar puncture/sub-arachnoid anaesthesia. Specialist neurosurgical advice should be sought regarding anaesthetic management.
Combined ICP management and regional anaesthesia has been reported using a lumbar drain.
Chiari malformation
The (Arnold) Chiari (type 1) malformation (ACM) consists of descent of the cerebellar tonsils and medulla through the foramen magnum (with or without syringomyelia). It has an incidence of ~0.7% in females, being completely asymptomatic in many cases. Classical presentation is with headache and neck pain, both worse on coughing and on neck extension. Issues of co-ordination, with nausea and vomiting, may occur. In the presence of syringomyelia, the loss of function in the central cord region can result in upper limb weakness and dissociative sensory loss with characteristic loss of pain sensation.
Key points
Dural puncture in a symptomatic, untreated ACM may cause acute tonsillar descent and coning.
CSFBrain:CSFspinal gradient is unlikely in the asymptomatic patient. Patients who have had corrective surgery may still have abnormal CSF flow.
Surgical treatment is foramen magnum decompression, with the aim of improving CSF drainage. The full benefits of surgery may not be achieved for 12 months following surgery.
Successful surgery results in lack of strain-related, or neck extension-related headache.
Syringomyelia is associated with sensitivity to non-depolarizing muscle relaxants and hyperkalaemia with suxamethonium.
NAP3 did not identify any cases where neurological complications could have been attributed to undiagnosed ACM Type 1 or 2 in either the obstetric or general population.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






