Chapter 25 Neurologic Emergencies
Neurologic Assessment
Some of these are discussed in more detail below.
Level of Consciousness
AEIOU-TIPS for Assessment of the Patient with Altered Level of Consciousness
• A—Alcohol (acute intoxication, withdrawal)
• E—Epilepsy (or any seizure), environmental conditions (hypothermia, heatstroke)
• I—Insulin (too much or too little)
• O—Oxygen (underdose or overdose)
• U—Uremia (or other metabolic disorders)
• T—Trauma, toxicity, tumors, thermoregulation
• S—Stroke, syncope (or other neurologic or cardiovascular cause)
Responsiveness
There are tools to help provide objectiveness in assessing a patient’s level of consciousness. A tool familiar to most health care providers is the Glasgow Coma Scale (GCS) (Table 25-1). Possible GCS scores range from 15 (best) to 3 (worst). A patient with a GCS score of 8 or less is considered severely altered (comatose). A score of 9 to 12 indicates moderate abnormality; those who score 13 to 15 are considered only mildly altered.1
| CATEGORY | SCORE | RESPONSE |
|---|---|---|
| Eye opening | 4 | Spontaneous: eyes open spontaneously without stimulation |
| 3 | To speech: eyes open with verbal stimulation but not necessarily to command | |
| 2 | To pain: eyes open with noxious stimuli | |
| 1 | None: no eye opening regardless of stimulation | |
| Verbal response | 5 | Oriented: accurate information about person, place, time, reason for hospitalization, and personal data |
| 4 | Confused: answers not appropriate to question but use of language is correct | |
| 3 | Inappropriate words: disorganized, random speech, no sustained conversation | |
| 2 | Incomprehensible sounds: moans, groans, and incomprehensible mumbles | |
| 1 | None: no verbalization despite stimulation | |
| Best motor response | 6 | Obeys commands: performs simple tasks on command; able to repeat performance |
| 5 | Localizes to pain: organized attempt to localize to remove painful stimuli | |
| 4 | Withdraws from pain: withdraws extremity from source of painful stimuli | |
| 3 | Abnormal flexion: decorticate posturing spontaneously or in response to noxious stimuli | |
| 2 | Extension: decerebrate posturing spontaneously or in response to noxious stimuli | |
| 1 | None: no response to noxious stimuli; flaccid |
Data from Urden, L. D., Stacy, K. M., & Lough, M. E. (2010). Critical care nursing: Diagnosis and management (6th ed.). St. Louis, MO: Mosby.
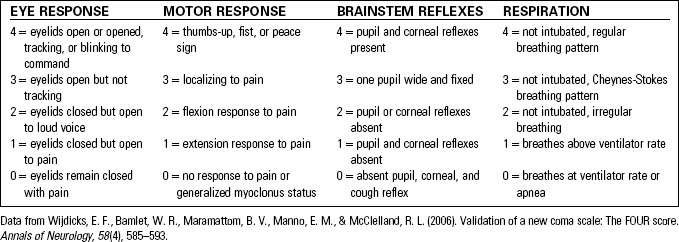
Another tool in assessing level of consciousness is the Full Outline of UnResponsiveness (FOUR) score of neurologic assessment.2,3 FOUR score (Table 25-2) was developed by neurologists at the Mayo Clinic as an alternative to the GCS in assessing and monitoring patients. Some practitioners believe that it is easier to use and provides more detailed information about the patient’s level of consciousness. FOUR score assesses eye, motor, brainstem, and respiratory function and assigns a score of 0 to 4 in each category. The lower the score, the more serious the patient’s condition. FOUR score does not assess a patient’s verbal abilities.
Mental Status Exam
Components of the Mini-Mental State Examination
• Orientation (order in which orientation is lost: time, then place, and finally person).
• Registration and memory: Name three unrelated items to the patient and ask him or her to state them back.
• Foundation of knowledge: Ask the patient what is on the national news.
• Attention span and calculation: For example, have the patient subtract backwards by 7 from 100.
• Naming: Show the patient an object and have him or her name it.
• Repetition: Have the patient repeat a statement.
• Comprehension: Give the patient simple directions to follow and see if he or she is able to follow the directions.
• Reading: Tell the patient to read a directive statement and then do what the statement says. For example, “Raise your hand.”
Cranial Nerve Assessment
Table 25-3 lists the cranial nerves and their functions. See Chapter 36, Head Trauma, for more information.
TABLE 25-3 CRANIAL NERVES AND THEIR FUNCTION
| NUMBER | NAME | FUNCTION |
|---|---|---|
| I | Olfactory | Smell |
| II | Optic | Vision |
| III | Oculomotor | Elevate upper lid, papillary constriction, most extraocular movements |
| IV | Trochlear | Downward, inward movement of the eye |
| V | Trigeminal | Chewing, clenching of the jaw, lateral jaw movement, corneal reflexes, face sensation |
| VI | Abducens | Lateral eye deviation |
| VII | Facial | Facial motor, taste, lacrimation, salivation |
| VIII | Vestibulocochlear | Equilibrium, hearing |
| IX | Glossopharyngeal | Swallowing, gag reflex, taste on posterior tongue |
| X | Vagus | Swallowing, gag reflex, abdominal viscera, phonation |
| XI | Spinal accessory | Head and shoulder movement |
| XII | Hypoglossal | Tongue movement |
Selected Emergencies
Unconsciousness
Unconsciousness is defined as a lack of awareness of self or of anything surrounding oneself, despite application of various stimuli. Assessment of the patient who is unconscious or who has an altered level of consciousness must be done concurrently with emergent interventions for airway, breathing, and circulation. Causes of unconsciousness can be categorized as structural, metabolic, toxic, or psychiatric (Table 25-4).
TABLE 25-4 DIFFERENTIAL DIAGNOSIS FOR COMA
| CATEGORY | DIFFERENTIAL DIAGNOSIS |
|---|---|
| Structural | Abscess, aneurysm, hematoma, hemorrhage, inflammation (i.e., meningitis, encephalitis), subarachnoid hemorrhage, stroke, trauma, tumor |
| Metabolic | Cardiopulmonary arrest, decreased cardiac output, elevated serum ammonia, fluid or electrolyte imbalance, hepatitis, hepatic dysfunction, hypoglycemia, hypothermia, hypothyroidism, seizure, vitamin deficiencies |
| Toxicity | Alcohol, anticholinergics, benzodiazepines, carbon monoxide, cyanide, opiates, salicylates, sedatives, tricyclic antidepressants, gamma hydroxybutyrate (GHB) |
| Psychiatric | Hysteria, malignant catatonia, psychogenic unresponsiveness |
Therapeutic Interventions
Therapeutic interventions for altered level of consciousness include the following:
• Support the patient’s airway, breathing, and circulation.
• Protect the patient from further deterioration.
• Identify and treat the underlying cause.
• Perform and document serial neurologic examination score and pupillary evaluations.