6 Ganna L. Breland and Dan Miulli All patients should be stabilized according to the “A, B, Cs” (A, airway; B, breathing; C, circulation). Most important in determining neurological injuries are the history and neurological examination. After the initial evaluation, the secondary survey includes lateral cervical spine x-rays. Some institutions have supplemented lateral cervical x-rays with CT scans with reconstructed views to rule out obvious fractures and malalignments. The quality of the lateral reconstructed cervical spine views depends on the thickness of the slice and their overlap; the smaller the thickness, the better the quality of reconstruction. Additional x-rays or films are taken as needed. Skull x-rays may show nontraumatic abnormalities, such as congenital skull defects, skull lesions, or even foreign bodies.1 Traumatic linear fractures must differentiate from vessel grooves and suture lines. Vessel grooves are thicker, and may curve and branch. Suture lines are wide and jagged and follow the course to meet other sutures.2 Traumatic linear fractures are often associated with epidural hematoma (EDH) or subdural hematoma (SDH).3
Neuroimaging and the Neurosurgical Intensive Care Unit Patient
 Plain Films
Plain Films
| Type | Characteristics |
| Linear | Differentiate from vessel grooves and suture lines; often associated with EDH or SDH |
| Depressed | Best evaluated by CT bone window; depression is greater than thickness of the skull or 8–10 mm |
| Diastatic | Widens the suture line |
| Growing | Wide fracture associated with dural tear; confirm with repeat imaging; rarely seen in pediatric patients and less so in adult population |
| Ping-pong fracture | Most likely seen in newborn; nonsurgical except for cosmetic purposes |
CT, computed tomography; EDH, epidural hematoma; SDH, subdural hematoma.
Traumatic depressed skull fractures are best evaluated by CT scan using bone windows. It is important to determine if there is trauma to underlying brain if the depression is greater than the thickness of the skull, or 8 to 10 mm.
The fracture may appear within the suture of the calvarium called diastasis, or widening of the suture line. On follow-up films, the fracture may grow if associated with dural tear. This is rarely seen in pediatric patients and less so in the adult population (Table 6–1).
Skull x-rays also demonstrate foreign bodies, postoperative changes, and extracranial material, such as reservoirs, plates, or screws, and intracranial material, such as shunt tubing, coils, or clips.
Spine x-rays may show nontraumatic abnormalities, such as congenital defects, degenerative processes, or pathological fractures.
Traumatic findings include fractures, dislocation, subluxation, and rotation. The completed cervical spine evaluation must be seen from the craniocervical junction through T1. If the entire view is not seen, then a swimmer’s view must be obtained with the arm above the head so that there is less tissue to shoot through. A consistent process must be adhered to every time a cervical spine x-ray is obtained. On a lateral x-ray, look for smooth contours of the anterior and posterior marginal line, as well as the alignment of the spinolaminar line. The alignment of the posterior spinous line is an approximation. When reviewing the posterior elements, attention should be paid to the fanning of the spinous processes. After the bone is inspected, the soft tissue should be reviewed. Prevertebral soft tissue swelling may be an indicator of damage as well. Approximations of normal width of the prevertebral tissue is 6 mm at C3 and 12 mm at C6.2 The lateral cervical spine x-ray should include measurement of the atlantodental interval as an indicator of atlantoaxial subluxation; it should be 2.5 to 3 mm in adults. Other areas of concern are the normal cervical lordotic curvature and loss of vertebral height, or fracture lines, or change in disk height. The same areas should be reviewed in the thoracic and lumbar spine. If there is a mechanism of injury that leads to cervical spine radiographs, then it is usually a good idea to x-ray the thoracic and lumbar spines (Table 6–2).
| X-ray view | Characteristics |
| Lateral cervical | Contours of anterior and posterior marginal line, spinolaminar line, and posterior spinous line Fanning of the spinous processes Prevertebral soft tissue swelling Atlantodental interval of 2.5–3 mm in adults Normal lordotic curvature Loss of vertebral height, fracture lines, disk height |
| Anteroposterior | Evidence of rotation and compression |
| Open mouth odontoid | Evaluation of odontoid fractures Occipitoatlantal joints Lateral masses overhang of C1 and C2 not more than 7 mm Atlantoaxial alignment |
| Oblique | Neural foramina, lamina, and pedicles |
| Anteroposterior and lateral | Measure angulation caused from compression or burst fractures |
| Oblique | Pedicles, lamina, facet joint, and pars interarticularis Useful to rule out spondylolysis |
X-rays in the neurosurgical intensive care unit (NICU) may be done after the application of a halo or tongs for traction to evaluate reduction after each addition of weights or each manipulation of the device. X-rays will look for postoperative instrumentation placement. Dynamic films, or flexion and extension films, evaluate motion. These are most often used for cervical spine clearance, but they are also used to evaluate subluxation with spondylolisthesis and compression fractures. For cervical spine clearance, the patient must be alert and cooperative. Dynamic films cannot be used if there is more than 3.5 mm subluxation seen on the lateral film or if the patient is not neurologically intact.
 CT Scan of the Brain
CT Scan of the Brain
CT scan is the best imaging tool for studying bone or other calcific structures. It is based on attenuation of the electron density of the material in the path of the x-ray beam. It is good for the initial assessment of head injury and neurological deficits, as well as for patients who cannot have magnetic resonance imaging (MRI). However, CT scan is prone to artifact from the densest material and cannot differentiate between soft tissues of similar densities; therefore, it is less advantageous for posterior fossa evaluation. It is contraindicated with contrast enhancement if the patient is in renal failure and blood urea nitrogen (BUN) > 2.0, or if there is a first-trimester pregnancy. CT scans can be completed with or without contrast. If you suspect a bleed inside the skull, do not use contrast on initial exam. Noncontrasted CT scans can also be utilized to evaluate hardware placement and function with deep brain stimulators, intracranial pressure (ICP) monitors and drains, external ventricular drain, and subdural catheters and as follow-up for residual or reaccumulation of hemorrhage. Contrasted CT scans are helpful when evaluating residual tumor or abscess, when MRI is not accessible or tolerated by the patient.
The CT scan measures exposures in Hounsfield units from – 1000 to 4000, progressing from dark (hypodense) to bright (hyperdense), for example, air→fat→water→CSF→brain tissue→subacute blood→liquid blood→clotted blood→bone→contrast→metals.4
CT scans can demonstrate deleterious changes for the neurological patient. This is useful when the neurological exam is compromised by sedation or overmedication. Some CT scan signs of increased intracranial pressure are the following:5
- Loss of sulci
- Compressed ventricles, loss of fourth ventricle
- Loss of cisterns
- Midline shift
As the condition worsens, the patient may progress to herniation (Table 6–3).
Brain CT scans are useful for the evaluation of neurological deficits, both new onset and progressive, and for following the progression of known pathology, such as hydrocephalus, infarction, edema, and intra- and extra-axial hemorrhage. Contrasted CT scans evaluate neurological deficits when there is a suspected mass or infection.
| Type of herniation | Characteristics |
| Subfalcine | Cingulated gyrus shifts under the falx |
| Central transtentorial | Diencephalon is forced through the incisura; obliteration of the quadrigeminal and perimesencephalic cisterns |
| Uncal | Uncus and hippocampal gyrus forced over the edge of the tentorium; decrease in suprasellar cistern followed by parasellar and interpeduncular cisterns |
| Upward | Cerebellar vermis ascends above tentorium; may cause hydrocephalus by compression of sylvian aqueduct and quadrigeminal cistern |
| Tonsillar | Cerebellar tonsils descend through foramen magnum (more likely seen on sagittal section of MRI) |
MRI, magnetic resonance imaging.
Some characteristic CT scan findings for bleeds are:6
- Epidural hematoma Biconvex or lentiform appearance, often underlying fractures, located between skull and dura; may be limited by suture lines; usually seen in acute phase when lesion is hyperdense; areas of hypodensity indicate active bleeding
- Subdural hematoma Crescent shaped, between brain and dura; may be acute (hyperdense), subacute (nearly isodense), or chronic (hypodense); areas of hypodensity indicate active bleeding in an acute SDH; may see areas of calcification in chronic SDH
- Subarachnoid hemorrhage (SAH) Seen within the cisterns and sulci
- Intracerebral hemorrhage (ICH) Seen in putamen, caudate, cerebellum, and brainstem where hypertensive hemorrhages are likely to occur spontaneously
EDHs are seen less frequently than SDHs and are usually the result of bleeding from the lacerated middle meningeal artery or the dural venous sinus.
SDH is usually the result of bleeding from bridging cortical veins.
SAH should be suspected before or after an accident or in association with the worst headache of the patient’s life. Most CT scans should be repeated in 12 to 24 hours. ICHs tend to reoccur after 6 to 12 hours.
CT Scan of the Spine
When used by itself, a CT scan of the spine provides limited data. It is useful for the evaluation of the bone and its alignment, such as when considering canal stenosis, degeneration, spontaneous hemorrhage, bony lesions, pathological fractures, traumatic fractures, or subluxation, or when planning for the surgical approach and instrumentation. When suspecting a fracture, obtain sagittal and coronal reconstructions for maximum benefit. There are also three-dimensional reconstructions that assist even further with fracture and malalignment identification.
A CT scan of the spine provides only limited data about soft tissue. When done after myelography, it becomes extremely useful, particularly when instrumentation obscures the view with MRI, the patient cannot tolerate MRI, or the patient has a history of multiple back surgeries. However, when concerned about changes within the spinal canal, other than stenosis, consider using MRI as the first advanced test. Contrasted CT scans can help identify osteomyelitis and tumor.
Other Types of CT Scans
CT scan information can be formatted in newer ways that have proven to be extremely beneficial, such as CT angiography (CTA). CTA is a less invasive test than conventional angiogram and offers comparable results for many clinical situations. It aids with the diagnosis of arterial dissections, acute stroke, and aneurysms.
 MRI
MRI
MRI is based on the relaxation characteristics of protons in different chemical states. For the optimal scan, the patient must not have any ferromagnetic material in the area to be scanned and must remain immobile in a narrow, loud scanning tube for 20 to 40 minutes; if not, the image will be severely degraded. The MRI is quite different from the CT scan in that different information can be sought based on the radiofrequency pulsations and magnetic gradients programmed prior to scanning. MRI does not use ionizing radiation, unlike CT scan. In the past, MRI has been more expensive, because it was a newer technology. Now the costs of MRI and CT are comparable, so the initial advanced test after the history and physical exam should be an MRI when appropriate. It is not cost-effective to use CT first.
MRI Protocols
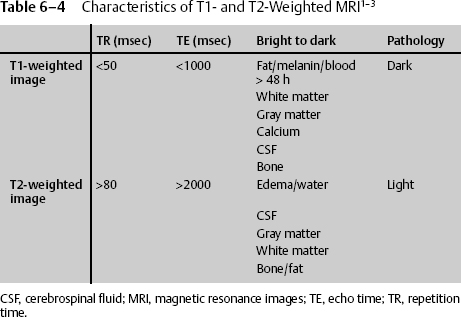
- T1-weighted image
- Echo time (TE) < 50, repetition time (TR) < 1000
- Progressing in intensity from hypointense, to isointense, to hyperintense (from dark to bright): bone→calcium→CSF→gray matter→white matter→fat/ melanin/blood > 48 hours old4
- Most pathology is dark (hypointense = low signal).
- Good for detecting gadolinium contrast enhancement
- Echo time (TE) < 50, repetition time (TR) < 1000
- T2-weighted image
- TE > 80, TR > 2000
- Progressing from dark to bright: fat→bone→white matter→gray matter→CSF→edema/water
- Notice that fat becomes dark on a T2-weighted image, whereas it is bright on a T1-weighted image.
- Most pathology is light.
- Gadolinium contrast enhancement does not cause much change in intensity of signal.
- Good for detecting pathological areas with edema, inflammation, or water (Table 6–4)
- TE > 80, TR > 2000
- Diffusion-weighted image
- Based on movement of water in tissues
- Freely diffusing water (CSF) appears dark, whereas restricted diffusion seen with intracellular edema–associated cell swelling from infarction appears bright.
- Acute infarction appears bright within minutes.
- Based on movement of water in tissues
- Perfusion-weighted image
- Uses a bolus of gadolinium
- Provides information on microcirculation and further insight into tissue infarction
- Used in combination with a diffusion-weighted image to define the area of ischemic penumbra (tissue near the infarction zone that may be salvageable by thrombolytic therapy)
- Uses a bolus of gadolinium
Other MRI protocols include fast spin echo, gradient echo, fluid attenuation inversion recovery (FLAIR), short T1 inversion recovery (STIR), and proton density.
MRI of the Brain
In general, MRI is good for evaluation of soft tissue, posterior fossa lesions, small lesions, and seizure workup when quantifying the amount of specific tissue present, such as the size of the hippocampus. Gadolinium contrast can be used in renal failure when CT contrast may not be used. MRI is still not the most accepted study when evaluating acute bleeding in the brain or for bone evaluation. The MRI scan is much slower than a CT scan, the former taking 20 to 40 minutes, the latter, mere seconds. It should not be used when patients have active pacemakers, known life-sustaining ferromagnetic implants, or any ferromagnetic implants directly in the area to be examined. Gunshot is not ferromagnetic unless a steel-jacket bullet is used, such as in the military.
MRI of the brain should be the first advanced scan in numerous conditions, such as
- Plain MRI
- Demyelinating disease
- Degenerative disease
- Edema
- Infarct (to distinguish between old and new strokes)
- Diffuse axonal injury caused by shearing from rotational or deceleration/ acceleration, seen at the gray matter-white matter junction, the corpus callosum, and the dorsolateral aspect of the upper brainstem, in order of frequency
- Midbrain and pontine injury
- Orbital compartment syndrome
- Demyelinating disease
- Contrasted MRI
- Tumor
- Infection
- Inflammation of nerves
- Tumor
MRI of the Spine
MRI is also very useful in the spine, especially when soft tissue evaluation is essential. It is the evaluation of choice after taking the patient’s history and performing a physical exam for herniated disc and nerve root impingement, congenital abnormalities, stroke, hemorrhage, ligamentous injury, spinal cord injury, and spinal cord hemorrhage. In the spine, MRI contrast and noncontrasted films are the imaging modality of choice for tumors, including drop metastases; infection, including paravertebral lesions; fistulas; the extent of tumor removal; and postoperative infection.6
In facilities with a neurosurgical intensive care unit, an MRI scanner must be available 24 hours a day. It is used emergently in patients with incomplete spinal cord injury or worsening neurological deficit, as well as clinical evidence without radiographic proof of spinal cord injury.5
Other Uses of MRI
MRI is used without contrast in determining peripheral nerve injury. Just as CT angiography provides detailed anatomy of the vessels in the brain and the large vessels of the spine, MRI angiography (MRA) demonstrates normal and pathological vascular anatomy such as carotid-cavernous fistulas, as well as vascular malformations, including aneurysms and arteriovenous malformations (AVMs). The venous phase of circulation can also be specifically probed when looking for venous sinus thrombosis. MRI has been employed in neuroscience for decades. It was once referred to as nuclear magnetic resonance (NMR), but the term was changed because of the connotation attached to nuclear. MRI examines the characteristic molecules in tissue samples. Magnetic resonance spectroscopy does the same thing on a much larger scale; it produces a graph based on the chemical shift and is used primarily in the brain to help distinguish tumor from infection.2
 Additional Imaging in the NICU
Additional Imaging in the NICU
The angiogram is an invasive test having a 0.5 to 2% risk of major morbidity or mortality.3 It also carries the risk of ionizing radiation. Although still the “gold standard” in many vascular cases, it has been replaced in some large institutions with CTA and MRA. In the community neurosurgical setting, it remains the procedure of choice to investigate cerebral AVM, aneurysm, and carotid-cavernous fistulas, to determine tumor blood supply and embolization of arterial feeders, to administer an injection for vasospasm, and to evaluate vessel injury (e.g., with gunshot wounds) and pseudoaneurysm development. In the spine the angiogram can be used to evaluate spinal AVM and dural fistulas.
Nuclear medicine scans, such as bone and tagged white blood scans, are used to evaluate osteoblastic activity seen in infection, tumor, and abnormal metabolism. They also can be used to differentiate between old and new fractures.
Transcranial Doppler scans have become extremely useful tools in both trauma and cerebral vascular disease. Such a scan can be performed at bedside to determine if there is vasospasm in the intracranial circulation, as well as the efficacy of thrombolysis in acute stroke. A transcranial Doppler is used to determine brain death.
Ultrasound has become critical in the evaluation of extracranial circulation, both carotid and vertebral, for the degree of stenosis, as well as in the evaluation of the neonatal brain.
 Radiology in the NICU
Radiology in the NICU
The brain and spinal cord cannot be directly visualized in the intact patient. The most important pieces of information needed to determine the disease process and treatment modalities in the neurocritical patient are the patient’s history and physical exam. After obtaining these, the physician must develop an informed opinion of what is wrong and how to treat the patient. Only after this opinion is formed should a radiographic examination be performed to confirm the physician’s hypothesis. Radiographic information is not a substitute for good clinical skills.
< div class='tao-gold-member'>