| Type | Microbial etiology |
|---|---|
| Type I | Polymicrobial (most common) |
| Type II | Monomicrobial (streptococci, staphylococci, clostridia) |
| Type III | Vibrio vulnificus (associated with seawater exposure) |
Presentation
Classic presentation
- NSTIs are notoriously difficult to diagnose early in the disease course, with initial signs and symptoms usually typical of cellulitis.
- Classically the pain is out of proportion to physical examination findings. As the infection rapidly spreads along the fascial planes, pain and swelling may extend beyond the areas of overlying erythema.
Critical presentation
- As an NSTI progresses, patients may present with ecchymoses, bullae, and crepitus as a result of subcutaneous emphysema. However, these occur later in the disease process (Figure 57.1).
- It is more common to see signs of systemic toxicity with NSTIs versus soft tissue infections without necrotizing component. This is due to the systemic inflammatory response from cytokine release, which can manifest as abnormal vital signs or abnormal laboratory markers.
- Type III NSTI associated with Vibrio vulnificus can present with cardiovascular collapse and rapid deterioration.

Figure 57.1. Ecchymosis and bullae of the upper extremity of a patient with an NSTI.
Diagnosis and evaluation
- NSTI is difficult to diagnose early in the disease process.
- Radiological studies can be helpful, but should not delay surgical intervention when there is a strong clinical suspicion for NSTI.
- Plain radiographs can demonstrate subcutaneous emphysema, but this is a late finding and should not be used to rule out NSTI (Figure 57.2).
- Advanced imaging modalities such as CT and MRI can reveal fascial thickening, edema, fluid along the fascial planes, and subcutaneous emphysema. They are not appropriate in unstable patients, or if they would result in a delay in surgical intervention.
- Emergency ultrasonography (EUS) can also aid in the diagnosis. EUS can reveal the above findings and also offers the advantage that it can be done quickly at the bedside (Figure 57.3).
- The gold standard for diagnosis remains surgical exploration for direct visualization of the deep subcutaneous tissues with histological confirmation.
- The classic intraoperative finding is “dishwater pus” and tissue necrosis.
- The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score can be utilized when trying to differentiate between necrotizing and nonnecrotizing serious soft tissue infections. It includes six variables associated with NSTIs that are used to calculate a score correlating with the magnitude of the risk (Tables 57.2 and 57.3).

Figure 57.2. Plain radiograph of the foot demonstrating subcutaneous emphysema.
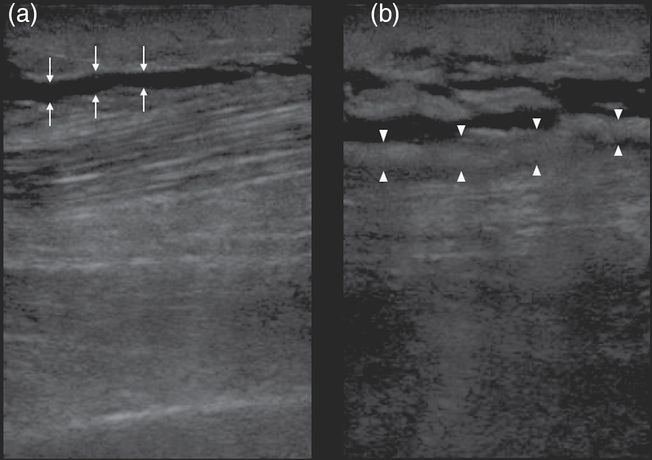
Figure 57.3. (a) Arrows indicate anechoic (black) fluid tracking along the echogenic (bright white) deep fascial plane. (b) Arrowheads delineate the thickened irregular fascia. In addition, anechoic fluid can be seen tracking along the deep fascial plane.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




