NECK TRAUMA
GEORGE A. WOODWARD, MD, MBA AND LILA O’MAHONY, MD, FAAP
GOALS OF EMERGENCY CARE
Pediatric neck injuries are uncommon; but many children are routinely evaluated for injuries after trauma. Because neck injuries can be life-threatening, including those that are subtle on presentation, children with neck trauma need to be assessed in a timely and orderly manner with a high index of suspicion. The goals of emergency care are to ensure a patent airway with adequate oxygenation and ventilation, control hemorrhage, maintain spinal stability, and identify and prevent progression of all injuries. A listing of common mechanisms of neck injury is given in Table 120.1. This chapter will discuss the evaluation and management of penetrating and direct blunt injuries, as well as the evaluation of the cervical spine taking into consideration the unique features that differentiate pediatric from adult neck anatomy and physiology.
KEY POINTS
 Pediatric neck injuries are uncommon.
Pediatric neck injuries are uncommon.
 Children have unique anatomical differences and mechanisms of injury that contribute to characteristic patterns of injury that vary from adults.
Children have unique anatomical differences and mechanisms of injury that contribute to characteristic patterns of injury that vary from adults.
 Multiple structures within the neck and cervical spine are at risk for injury, knowing their anatomic relationships will help guide the emergency evaluation.
Multiple structures within the neck and cervical spine are at risk for injury, knowing their anatomic relationships will help guide the emergency evaluation.
 Management priorities are first to ensure a patent airway, adequate respiration, control of hemorrhage, and spinal stabilization and second to identify and prevent progression of all injuries.
Management priorities are first to ensure a patent airway, adequate respiration, control of hemorrhage, and spinal stabilization and second to identify and prevent progression of all injuries.
RELATED CHAPTERS
Resuscitation and Stabilization
• Approach to the Injured Child: Chapter 2
Signs and Symptoms
• Respiratory Distress: Chapter 66
Medical, Surgical, and Trauma Emergencies
PENETRATING TRAUMA
Goals of Treatment
To anticipate, identify, manage, and prevent progression of all injuries to structures and tissues within the neck, including the airway, major blood vessels, nerves, and osseous structures.
CLINICAL PEARLS AND PITFALLS
• Penetrating trauma may be associated with extracervical injuries and involve multiple organ systems within the neck.
• Pattern of injury may not be limited to the pathway of the penetrating object.
• Injury to blood vessels can be dramatic or subtle with an initially normal examination. Vigilance and high index of suspicion is warranted.
• History of large blood loss, pulsatile lesion, rapidly expanding hematoma, hypovolemic shock, or neurologic deficits (paresis, visual loss or aphasia, altered level of consciousness) indicates possible vascular injury.
• Respiratory distress, stridor, hoarse voice, and speech difficulties may also be indicators of injury.
• Spinal cord and vertebral levels are not the same. In the cervical area, the cord level lies one segment higher than the corresponding vertebral level (C4 cord level lies opposite the C3 vertebral body). In the lower cervical area, a disparity of up to two levels may be present. This means that physical injury and objective findings may not be straightforward.
• Evaluate the chest for signs of major vessel injury, including hemothorax, widened mediastinum, and cardiac tamponade.
TABLE 120.1
COMMON MECHANISMS OF BLUNT AND PENETRATING NECK INJURIES
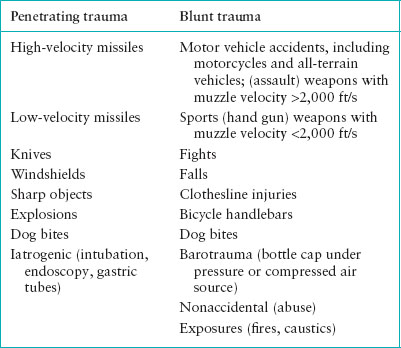
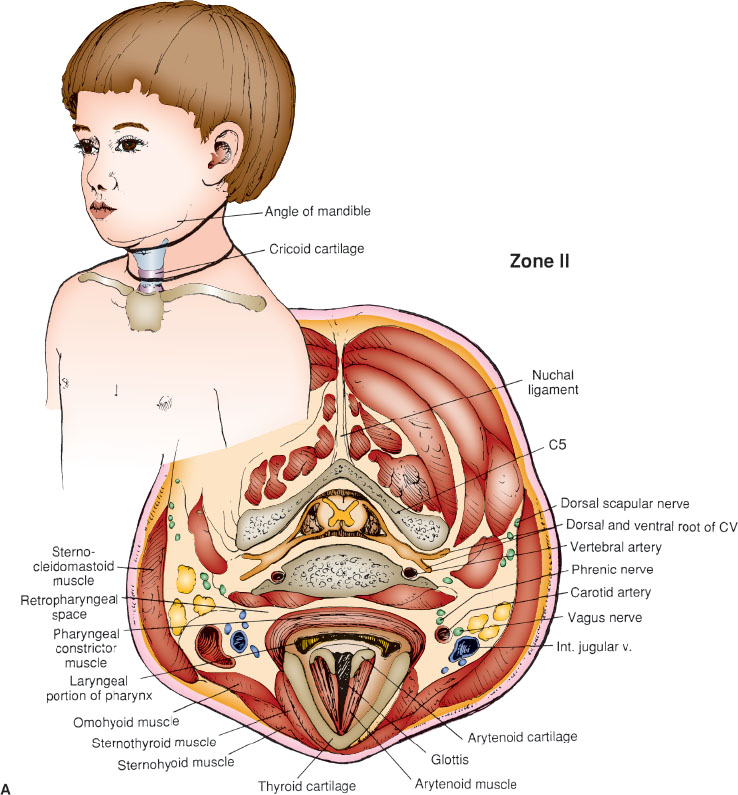
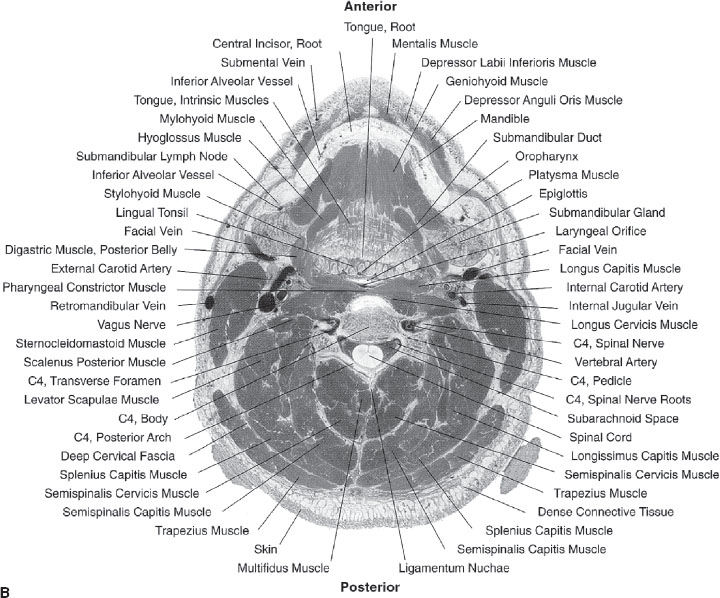
FIGURE 120.1 Anatomic neck divisions and contents of zone II located between the upper boundary of zone I and the angle of the mandible. B: Anatomic specimen demonstrating zone II relationships. (B: From Spitzer VM, Whitlock DG. Atlas of the visible human male: reverse engineering of the human body. Sodburg, MA: Jones & Bartlett, 1998. Reprinted with permission.)
Current Evidence
Penetrating neck trauma is uncommon in children, but most often is the result of a wound from a gunshot (usually low muzzle velocity <2,000 ft per second) (Fig. 120.1), knife, broken windshield, other sharp object, or explosion (Table 120.1). The soft tissues and visceral components of the neck are protected by the spine posteriorly, the mandible anteriorly and superiorly, the shoulders and clavicles anteriorly and inferiorly, and the neck muscles. The child’s relatively large head, mandible, and short neck make the anterior neck less accessible to direct trauma. However, if the neck is hyperextended, the structures of the anterior neck, including the larynx, trachea, and esophagus, are more exposed and susceptible to injury. The potential severity of direct penetrating or blunt injuries (Table 120.2) is increased because of the relatively small neck area with its large number of vital organs and structures.
Traditionally, the anterior neck has been divided into three anatomic zones (Figs. 120.2 to 120.4). Zone I encompasses the area between the thoracic inlet and the cricoid (the lower boundary of zone I is the thoracic inlet, the upper boundary is most often classified as the cricoid); zone II is the area between the cricoid and the angle of the mandible; and zone III is the area above the angle of the mandible. Knowledge of the divisions and structures they contain can be useful in the evaluation and management of neck trauma (Figs. 120.2 to 120.4). The most common site of significant penetrating injuries is in zone II. Compared to injuries in the other zones, zone II injuries tend to have a more straightforward presentation and surgical exploration with an associated mortality between 3% and 9%, with or without surgical intrervention.
Vascular injury is the most common complication of penetrating trauma and is the second most common cause of death. Injuries include aneurysms, dissections, occlusions, and fistulas. Major vessels that can be injured in the neck include the common, internal, and external carotid arteries; vertebral arteries; internal and external jugular veins; and nearby innominate and subclavian vessels (Table 120.2). Approximately one-third of arterial injuries present with neurologic deficits, whereas the remaining two-thirds are often more challenging to diagnose.
The subtle presentation of vascular injuries historically, led many authors to suggest mandatory exploration of all neck injuries when the outermost muscle layer (platysma) was penetrated. More recently, the literature suggests that careful evaluation, along with ancillary studies, including arteriography, helical multislice computed tomographic (CT) scan, and color flow Doppler (CFD) coupled with the use of selective exploration, can reliably identify most significant injuries without an increase in morbidity and mortality from delays while diagnostic evaluation is being completed. The multislice helical CT scan has been noted to be a sensitive and specific diagnostic tool including the multislice helical CT angiography (CTA) in detecting vascular and aerodigestive injury with reported 100% sensitivity and 93% specificity. In some institutions, CTA has replaced conventional angiography for the vascular assessment of neck injuries, resulting in fewer neck explorations, and essentially eliminating negative exploratory surgeries. Subsequently, the use of CTA has transcribed the zone of injury into a descriptor rather than a triage tool or guide for exploratory surgery. CFD is a noninvasive, relatively sensitive screening tool with high specificity, PPV and NPV for vascular injury, but can be limited by adjacent or overlying hematomas and pneumothoraces as well as by the skill of the individual operator. The physical examination alone has been reported to have 93% sensitivity and 87% positive predictive value in predicting vascular injuries.
TABLE 120.2
NECK CONTENTS AND CLOSELY APPROXIMATED STRUCTURES
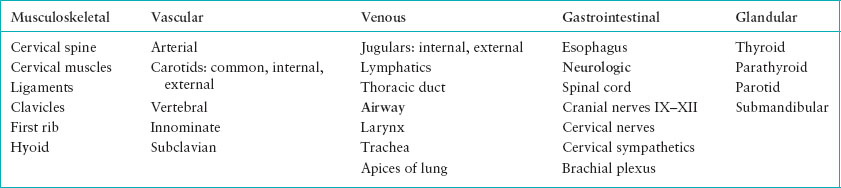
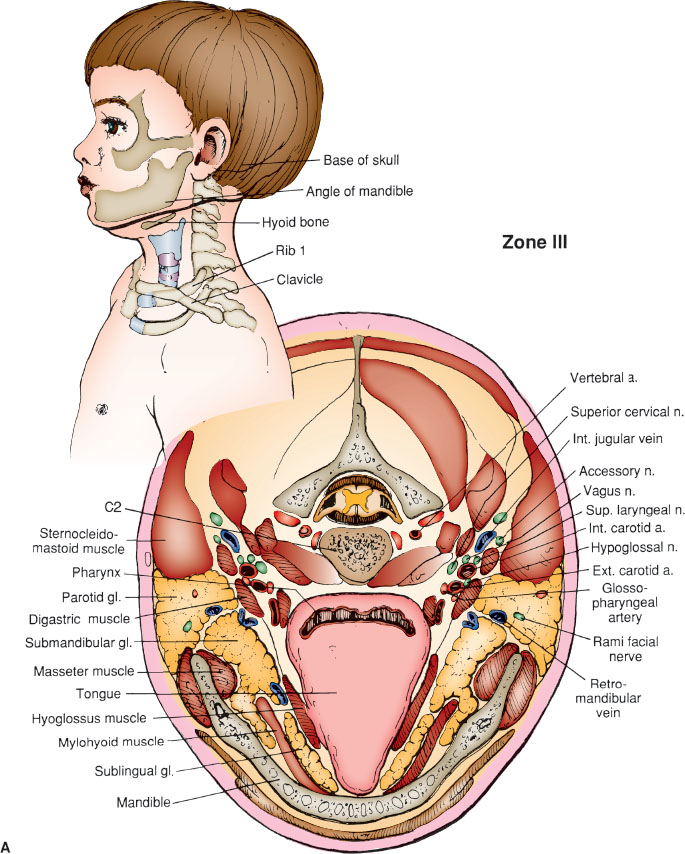
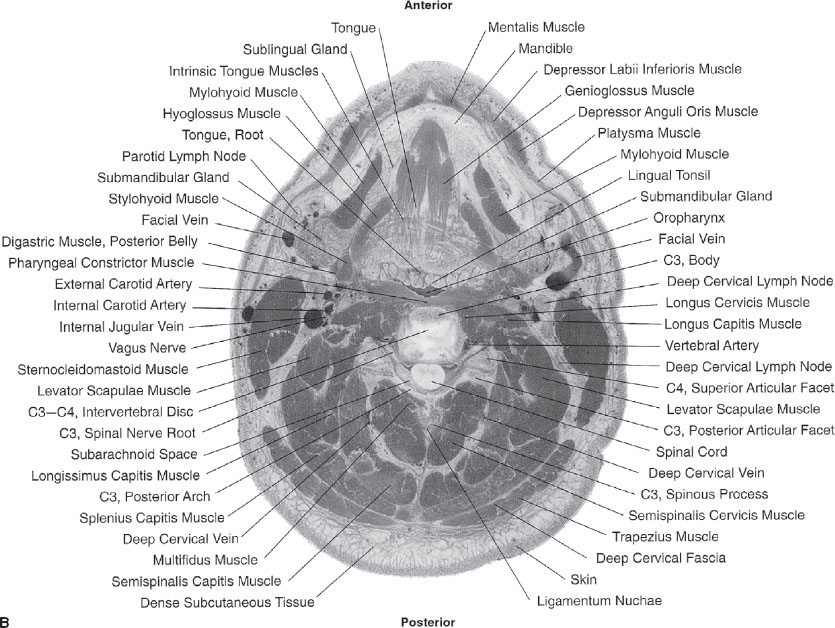
FIGURE 120.2 A: Anatomic neck divisions and contents of zone III. Zone III includes the area above the upper boundary of zone II. B: Anatomic specimen demonstrating zone III relationships. (B: From Spitzer VM, Whitlock DG. Atlas of the visible human male: reverse engineering of the human body. Sodburg, MA: Jones & Bartlett, 1998. Reprinted with permission.)
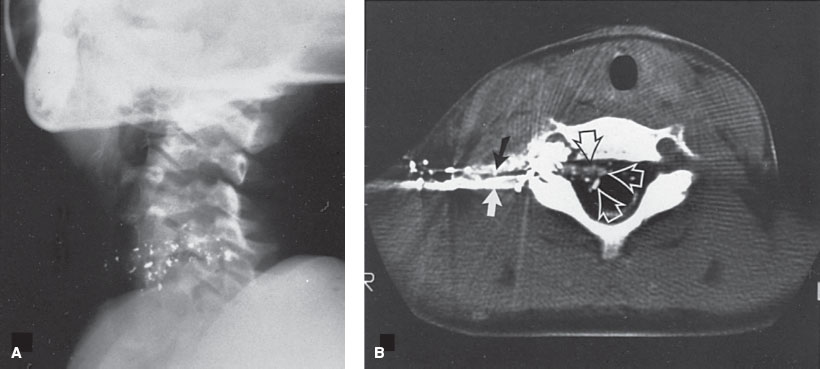
FIGURE 120.3 A: Gunshot wound (0.22 caliber) to the neck in a 5-year-old girl. A: Lateral neck radiograph showing fragmentation of bullet along path. B: Computed tomography (CT) scan of same patient demonstrating bullet fragments in and around the spinal canal, as well as cerebrospinal fluid and contrast leak from disruption of the dura.
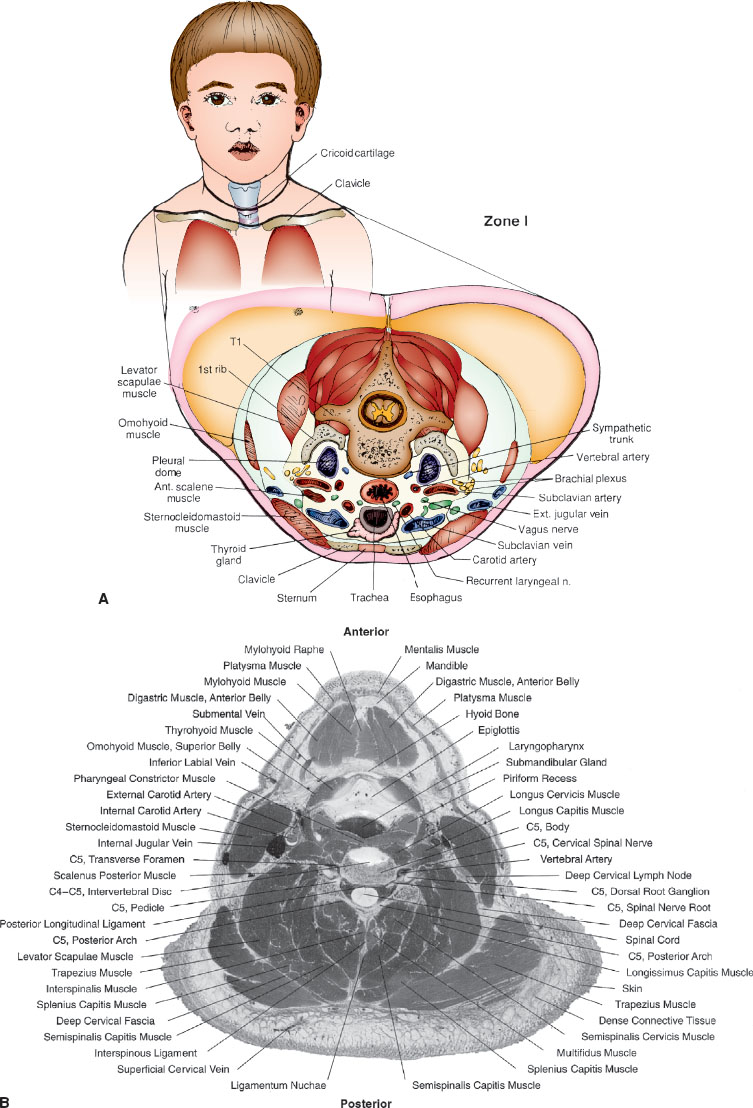
FIGURE 120.4 A: Anatomic neck divisions and contents of zone II located between the upper boundary of zone I and the angle of the mandible. B: Anatomic specimen demonstrating zone II relationships. (B: From Spitzer VM, Whitlock DG. Atlas of the visible human male: reverse engineering of the human body. Sodburg, MA: Jones & Bartlett, 1998. Reprinted with permission.)
Penetrating injury of the larynx and trachea occur, although blunt trauma to these areas is more common and can be associated with significant morbidity and mortality (see Chapter 126 ENT Emergencies).
Clinical Considerations
Clinical Recognition
While penetrating neck trauma is rare in children, if a child presents with a history consistent with this type of injury, the clinician should have a high index of suspicion for potential injuries based on the penetrating object, force, location of penetration, and initial clinical assessment. Consequences of missed injuries include airway obstruction, delayed hemorrhage, neurologic compromise, and deep neck infection, with potentially significant morbidity and mortality.
Triage Considerations
These patients require close monitoring, may have difficult airway management, and may require massive transfusion support for severe blood loss. All penetrating objects protruding from a child’s neck should be stabilized and not removed in the emergency department unless under direct supervision by appropriate specialist after complete evaluation. Early transfer to a pediatric trauma center should be considered if appropriate surgical or critical care staff is not available.
Clinical Assessment
Rapid assessment of the patient’s physiologic status should take precedence and will largely determine the ensuing management or further clinical evaluation. For patients who have “hard signs” of injury (cardiovascular shock, pulsatile bleeding or expanding hematoma, audible airway compromise, bubbling wound, extensive subcutaneous air, stridor, hoarseness, signs of intracerebral ischemia), surgical evaluation and intervention will likely ensue. For those patients without “hard signs,” further clinical evaluation will continue.
The history of the event is important in the evaluation of penetrating neck trauma. Inquiries about the mechanism of injury, time of incident, events before arrival in the ED, amount of blood loss, history of pulsatile lesions, neurologic dysfunction including transient ischemic attack, limb paresthesias, hemiplegia, blindness, Horner syndrome (ptosis, miosis, enophthalmos, loss of sweating on the ipsilateral side of the face), and aphasia; and airway compromise should all be noted. In particular, knowledge of the mechanism of injury and associated risks of injury can help direct the management of both the stable and unstable patient.
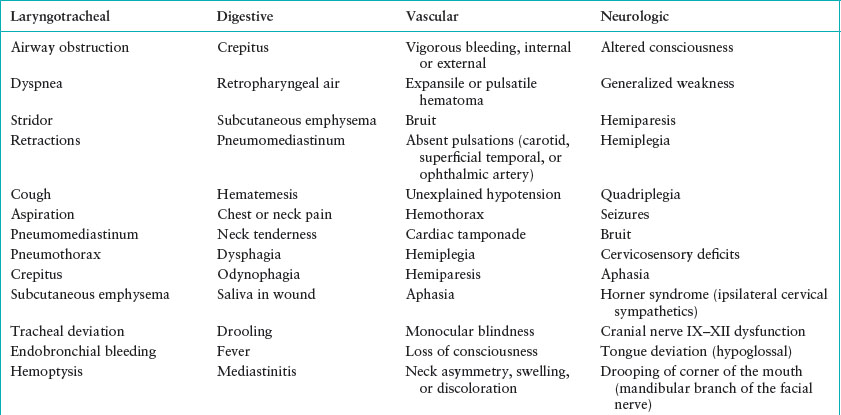
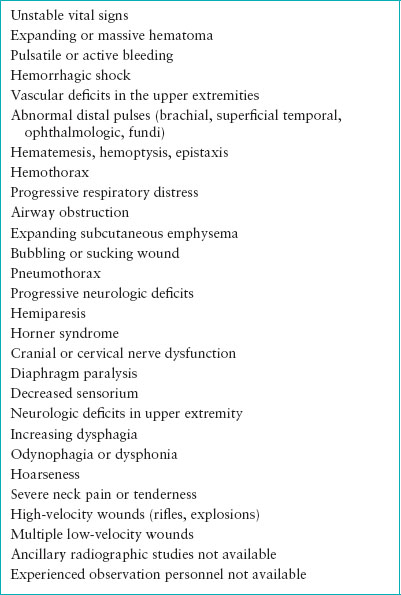
The symptoms and signs suggestive of vascular and other neck injuries are presented in Table 120.3. Completely transected arteries often retract and contract with minimal bleeding. Vessels that are partially severed may continue to bleed significantly with normal pulses because blood flow may not be totally interrupted. Vascular abnormalities can be assessed partially by evaluating the carotid (external), superficial temporal, and brachial pulses, although pulses are not easily accessible to evaluate the internal carotid or vertebral arteries. Abnormal pulses suggest vascular injury, whereas normal pulses do not guarantee vascular integrity.
Auscultation of the neck is useful to identify bruits. Although a carotid bruit may be normal in children, a continuous bruit suggests a traumatic arteriovenous fistula whereas a systolic bruit suggests a partial arterial tear. Bleeding from a posterior neck wound, neurologic deficits in areas supplied by the vertebral arteries (brainstem, cerebellum), bleeding not controlled by carotid compression, a posterior bruit, or bleeding that accompanies a cervical spine transverse process fracture suggests a vertebral artery injury. Carotid artery trauma should be suspected if presentation involves an anterior triangle hematoma, Horner syndrome, transient ischemic attack, loss of consciousness after a lucid interval, or hemiplegia.
Neck vessels may be injured indirectly as a result of shock waves from a penetrating object or bullet. These patients may have clinically unrecognized vascular intimal damage that can progress to vascular thrombus or occlusion. Venous or lymphatic (thoracic duct) injuries also occur with penetrating trauma. These injuries are rarely severe and usually present as an expanding hematoma or less often with a venous air embolism. If venous air embolism is suspected because of an unexplained decrease in cardiac output and blood pressure, increase in central venous pressure, cyanosis, arrhythmias, or air in the heart on chest radiograph, the patient should be placed in the left lateral decubitus and Trendelenburg positions.
Injuries to the aerodigestive tract (pharynx, larynx, trachea, and esophagus) also occur in cases of penetrating trauma, although these relatively mobile structures are often spared. The esophagus is somewhat protected in that it is usually collapsed as it courses through the neck but it may be injured by direct penetrating objects, usually a stab or gunshot wound. These injuries can present initially in a subtle fashion, but delays in diagnosis can lead to significant increase in observed morbidity and mortality.
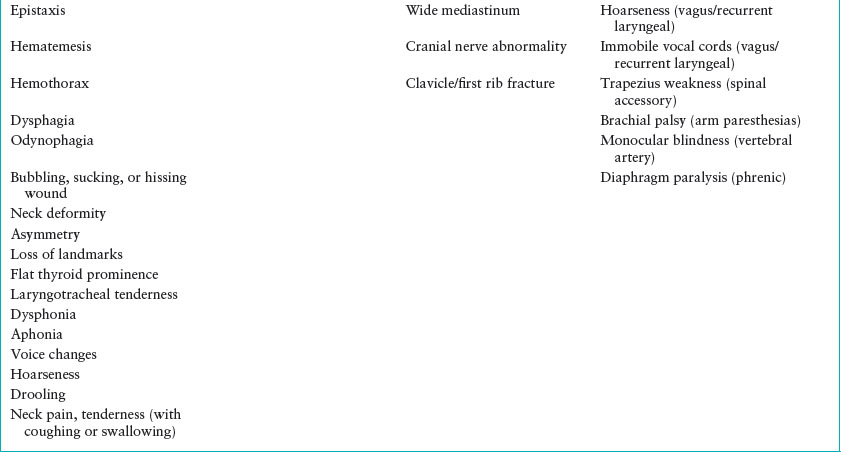
Direct nervous system injury (brachial plexus, spinal cord, cervical nerves) is possible with penetrating neck trauma and the evaluation of the patient should assess these structures and their function. A thorough neurologic examination should be completed and abnormal findings should correspond to the injured structure (Fig. 120.5). Primary injury to the cervical cord often results from bony or foreign-body penetration or impingement or cord distraction. Secondary cord injury can occur from vascular compromise, edema, lipid peroxidation, ischemia, and ligamentous damage.
Management
The goals of management are to ensure airway patency and adequate respiration, control hemorrhage, maintain osseous stability, and identify and prevent progression of all injuries. Methodical and timely acquisition of historical and physical findings is mandatory. The patient must be managed with strict adherence to the ABCs, with consideration of potential rapid or gradual deterioration. Penetrating objects that are lodged in the neck should remain in place until removed under surgical care, preferably in an operating room. All patients, other than those with minor injuries such as contusions, abrasions, or superficial lacerations (not through the platysma muscle), should receive supplemental humidified oxygen, cervical spine stabilization if indicated, correct airway positioning, suctioning, close observation, and monitoring. The patient should be maintained in a supine or Trendelenburg position to avoid the possibility of venous air embolism. A decision tree for the evaluation of direct blunt and penetrating neck trauma is presented in Figure 120.6. Patients with “hard signs” of injury should be immediately evaluated for surgical intervention.
TABLE 120.3
SYMPTOMS AND SIGNS OF NECK INJURIES
Airway assessment is the initial step in the evaluation of all patients with trauma. Any airway manipulation should be accomplished with consideration and prevention of possible cervical spine injury. Potential indications for an artificial airway with neck trauma include stridor, dyspnea, hypoxia, rapidly expanding hematoma, expanding crepitus, pneumothorax, hemothorax, tracheal deviation, altered mental status, quadriplegia, hemiparesis, and other signs of vascular or airway insufficiency. If the airway is unstable, intubation should be considered. Orotracheal intubation is the preferred method in children. Intubation should be attempted only after preparation for the placement of a surgical airway, if time allows. Fiber-optic intubation via the nasal route, performed by a skilled provider, may be useful. The physician must be especially careful with the use of blind nasotracheal intubation in the patient with blunt or penetrating neck or facial trauma because the airway anatomy may be distorted. Passage of the nasotracheal or orotracheal tube into a false or blind passage may make subsequent airway control attempts difficult, if not impossible. Therefore, considering the difficulty of emergent surgical airway placement in children, elective intubation is not recommended outside a setting where a surgical airway can be efficiently and skillfully placed.
FIGURE 120.5 A: Sensory dermatomes. B: Motor dermatomes. Knowledge of sensory and motor dermatomes can be invaluable in description of neurologic findings during initial and subsequent evaluations.
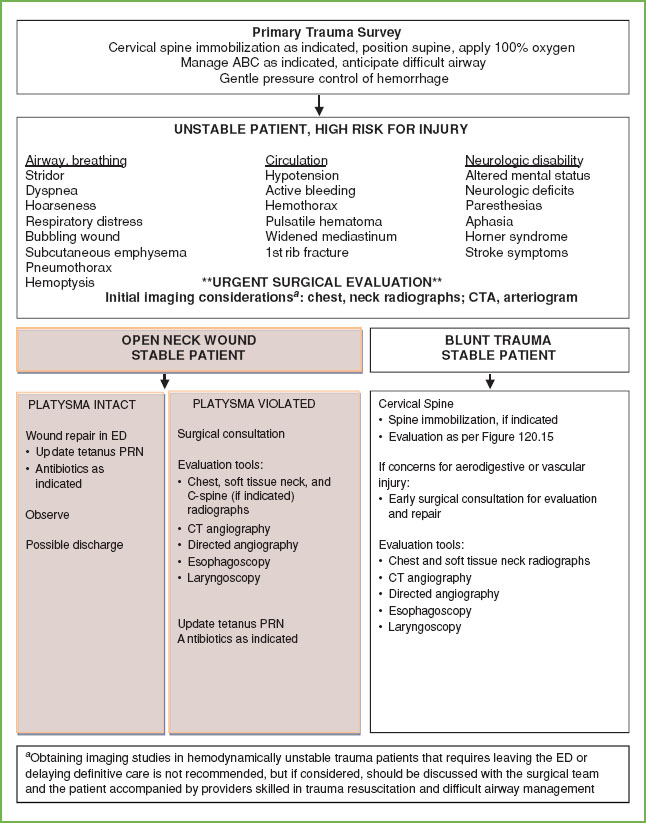
FIGURE 120.6 Evaluation of blunt and penetrating neck trauma.
If there is evidence of crepitus over the larynx, laryngeal or tracheal tenderness, a flattened thyroid prominence, anterior neck deformity, severe respiratory distress, an abnormal neck radiograph, or other evidence suggestive of a laryngotracheal fracture or disruption, a tracheostomy may be preferable. In this scenario, intubation should only be attempted if the airway is completely obstructed. Attempts at intubation from above may separate a tenuously attached trachea and larynx, resulting in a total loss of the airway, with the trachea commonly retracting substernally into the chest (Fig. 120.7). Attempts at cricothyrotomy in patients with direct laryngeal trauma may result in retrotracheal placement of the airway. Cricothyrotomy may be helpful in patients who have severe facial or other neck injuries that preclude intubation from above. Intubation may be attempted through an open laryngeal wound if present, although, if possible, a tracheostomy should not be performed through injured tissue. The flexible fiber-optic bronchoscope may be helpful in evaluating the patency of the airway and establishing the artificial airway. If patient condition allows, rigid bronchoscopy can also be useful in securing an airway in these patients. Care should be taken to ensure correct positioning and securing of the artificial airway, as the usual landmarks and adjacent tissues may be injured or altered.
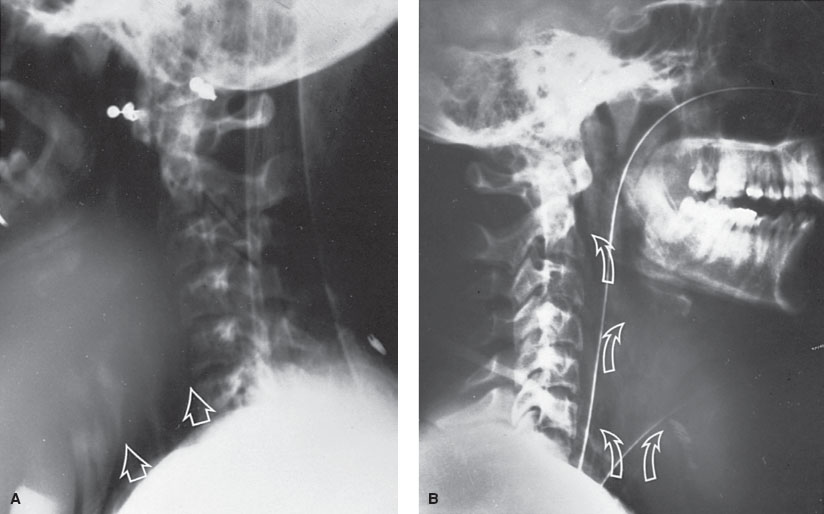
FIGURE 120.7 Tracheal injury. A: Initial lateral neck radiograph showing subcutaneous emphysema (solid arrows) in 14-year-old girl kicked in the neck by a horse. Patient’s airway clinically stable at the time of this radiograph (more than 1 hour after the injury). B: Postcricothyrotomy radiograph in same patient demonstrating significant subcutaneous emphysema and an artificial airway in place (open arrows). Initial attempt at orotracheal intubation separated tenuously attached trachea, completing traumatic disruption of the trachea and requiring immediate placement of surgical airway.
Breathing abnormalities may suggest associated injuries. Missiles to the neck may also pass through or lodge in the chest. Zone I injuries of the neck can easily involve the lung apices and result in hemothorax, pneumothorax, or pneumomediastinum. Further penetration may lead to cardiac tamponade. A chest radiograph is helpful in the assessment. A normal physical examination and chest radiograph are likely sufficient to obviate the need for arteriography in this population.
In addition to the usual assessment for hypovolemia, the patient should be examined for expanding hematomas or other obvious external bleeding. External bleeding should be treated with gentle compression. Attempts to clamp bleeding vessels in the neck can injure the vessels and surrounding structures, as well as jeopardize subsequent repair attempts. Two large-bore intravenous (IV) catheters should be inserted, ideally on the side opposite to the injury if an obvious vascular abnormality is identified. If a subclavian vein injury is suspected, one of the IV catheters should be placed in the lower extremity; if there are no contraindications.
A neurologic examination for signs of cerebral injury secondary to vascular insufficiency, direct spinal cord, cranial or cervical nerve, or brachial plexus injury should be completed. An abnormal or changing neurologic examination may indicate progressive vascular insufficiency and the need for rapid surgical evaluation. Rapid assessment by CT or magnetic resonance imaging (MRI), followed by surgical intervention, will provide opportunity for optimal outcome. Direct nerve injuries may not necessitate surgical repair.
Tetanus status should be assessed in all patients with penetrating trauma. The clinician should consider a broad-spectrum antibiotic for a patient with evidence of neck trauma, especially if esophageal or pharyngeal injury seems likely. Placement of a nasogastric or an orogastric tube is controversial for the patient with cervical injury because it may worsen a pre-existing esophageal injury or dislodge clots in zone I of the neck. When placed, these tubes should be well lubricated, inserted gently and slowly, and withdrawn if difficulty in passage or evidence of obstruction occurs.
Superficial abrasions, lacerations, and puncture wounds are common in children. Wounds superficial to the platysma can be cleaned and sutured under local anesthesia in the ED. Clean wounds can be sutured as late as 12 to 18 hours after the injury because of the excellent blood flow in the neck. Closure after 72 hours is not recommended. Penetration of the platysma is an indication for surgical referral and, in some cases, surgical exploration. When neck wounds that penetrate the platysma are evaluated, exploration in the ED is discouraged because of the risk of clot dislodgement and venous air embolism. Rapid surgical exploration and repair are indicated in patients struck by a high-velocity missile, those with unstable vital signs, uncontrollable bleeding, rapidly expanding hematomas, progressive airway compromise, worsening neurologic symptoms, increasing subcutaneous emphysema, or bubbling wounds (Table 120.4).
TABLE 120.4
INDICATIONS SUGGESTING SURGICAL EVALUATION IN PATIENTS WITH NECK TRAUMA
Surgical evaluation may give false-negative results with esophageal lacerations, small vessel lacerations, pharyngeal lacerations, or tracheal injuries. The patient who has stable vital signs, no symptoms of impaired neurologic or cardiovascular status, an intact airway, and mechanisms of injury with a low-velocity bullet or single knife wound may be managed expectantly with the use of ancillary diagnostic tests and close observation, preferably for at least 48 hours. These decisions should be made in conjunction with experienced surgical staff.
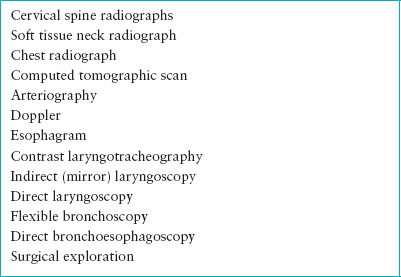
Adjuncts to the history and physical examination are given in Table 120.5. Initial evaluation should include cervical spine radiographs to detect bony or structural abnormalities, as well as a soft tissue lateral neck radiograph to assess for blood, edema, subcutaneous air, foreign bodies, and airway impingement or disruption. A chest radiograph should be evaluated for evidence of hemothorax or pneumothorax, mediastinal emphysema or widening, and heart size. If a serious injury is likely, radiographs should be obtained in the ED or the patient should be accompanied to the radiology department by someone skilled in airway management. If the patient is stable and a vascular injury is suspected, a CTA or arteriogram should be performed (Fig. 120.8). Contrast laryngography, tomography, and xeroradiography have been used for further evaluation; however, these methods have generally been replaced by the CT scan. CT may not be accurate for detection of mucosal degloving injuries, mucosal perforation in the presence of subcutaneous emphysema, endolaryngeal edema or hematoma, and partial laryngotracheal separation. Noninvasive Doppler studies and oculoplethysmography may also be useful in evaluating vascular injuries.
TABLE 120.5
ADJUNCTS TO HISTORY AND PHYSICAL EXAMINATION
Contrast esophagram is helpful in evaluating the esophagus for tears or perforations, but false-negative rates of up to 50% have been reported. Evaluation can also include indirect mirror laryngoscopy to assess the larynx, vocal cord mobility, presence of mucosal edema, ecchymosis, and mucosal tears, as well as direct endoscopy to examine for tracheal, bronchial, and esophageal damage. Flexible endoscopy may be less invasive and easier to accomplish, but rigid endoscopy offers the most complete examination. Even rigid endoscopy, however, is not 100% sensitive in detecting tracheal and esophageal injuries. As mentioned, operative evaluation is mandatory for some patients and optional for others. Determinants of specific management direction include mechanism of injury, wound size and type, patient signs and symptoms, and relative stability.
Clinical Indications for Discharge or Admission
Patients can be discharged if they do not have a significant injury without platysmal penetration, are hemodynamically stable, without airway compromise, able to tolerate oral intake, and no indication or risk of abusive trauma or neglect is present. Otherwise, admission is indicated.
BLUNT TRAUMA
Goals of Treatment
To ensure airway patency, respiratory sufficiency, hemorrhage control, cervical spine stability, and identify and prevent progression of injuries to all structures and tissues within the neck, including the airway, major blood vessels, neurologic, and osseous structures.
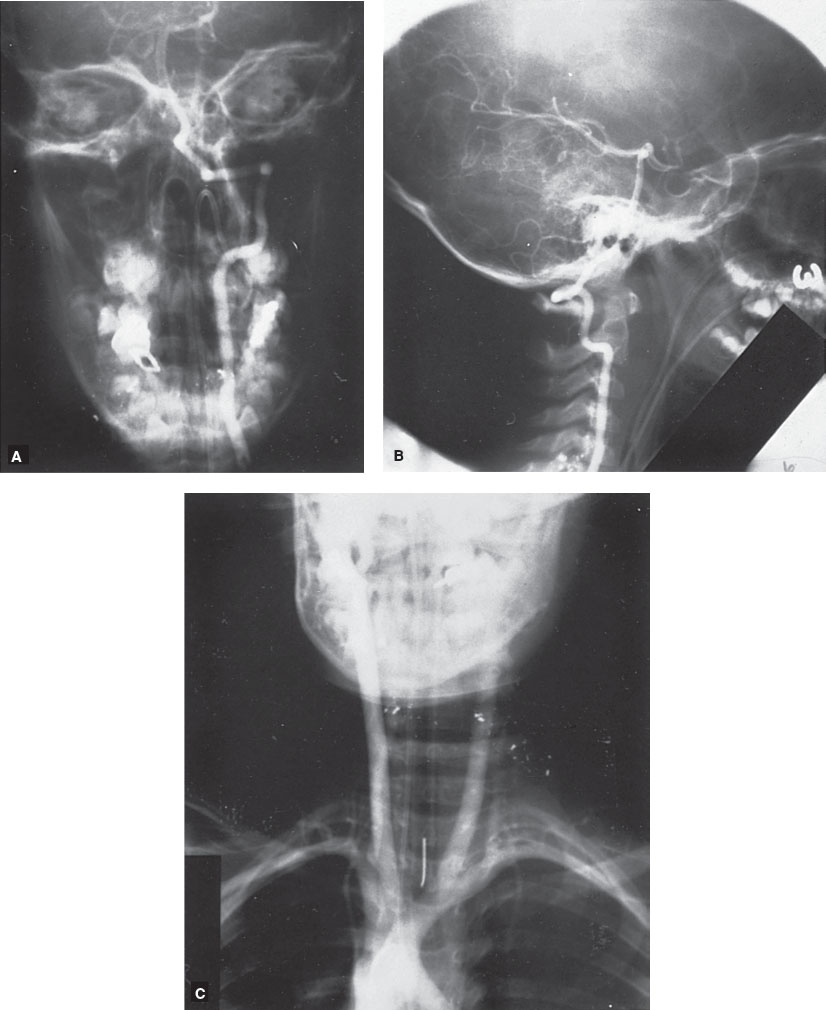
FIGURE 120.8 Angiograms in 5-year-old child shot in the neck, demonstrating normal vascular integrity. A: Vertebral artery angiogram (anteroposterior view). B: Vertebral artery angiogram (lateral view). C: Carotid angiogram.
CLINICAL PEARLS AND PITFALLS
• The airway may be injured with direct blunt trauma in part due to the anterior position of the larynx and trachea.
• Dyspnea, hemoptysis, and stridor suggest laryngeal airway.
• Cervical emphysema, dysphagia, and progressive airway obstruction characterize supraglottic injuries.
• Hemoptysis and persistent air leak suggest injuries inferior to the glottis.
• Early airway management should be considered for patients with facial and neck burns.
• Vascular injuries are less common compared to penetrating trauma, but are also missed on routine examination. Maintain a high index of suspicion.
• The cervical spine should be immobilized if indicated by mechanism of injury, inability to clinically clear, or in the presence of significant head/neck trauma.
Current Evidence
Blunt trauma is often the result of a motor vehicle accident, although it can also result from sports-related injuries; clothesline and handlebar injuries from bicycles, motorcycles, all-terrain vehicles, and snowmobiles; strangulation; hanging; direct blows and various forms of child abuse (Table 120.1). Pediatric-specific mechanisms of injury as well as the fact that children have a relatively short neck, mobile laryngotracheal structures, and a superior-positioned larynx protected by the mandibular arch make it less likely for children to sustain airway fractures and may impact overall severity of injury. On the other hand, the small and narrow airway increases the risk of airway-related morbidity secondary to airway edema, bleeding, swelling, and obstruction. Blunt trauma is often associated with extracervical injuries, especially maxillofacial, head, chest, and aerodigestive injuries, but is less likely than penetrating trauma to involve multiple structures within the neck or cause vascular damage.
The airway may be injured with direct blunt trauma in part as a result of the anterior and relatively fixed position of the larynx and trachea. High-impact blunt trauma to the trachea has been associated with a mortality rate of approximately 15%, although this is likely higher when one considers patients who die at the scene. The anterior neck is relatively well protected by bony structures, unless the neck is extended. With neck extension, the larynx, trachea, and esophagus are exposed to direct trauma and a blunt force may crush these structures against the posterior spinal column. A tracheal tear or rupture may occur from a sudden increase in intratracheal pressure against a closed glottis, direct blunt trauma, crush, or acceleration/deceleration injury. Shearing forces can cause edema, submucosal hematoma, laceration, perforation, vocal cord injury, and, less commonly, partial or complete airway transection. A prime target for airway fracture is the cricoid ring, which is the only complete tracheal ring.
Approximately 85% of patients with blunt tracheal injury reportedly have subcutaneous emphysema, although the onset may be delayed (Fig. 120.9). However, airway injuries may be subtle and not apparent with initial history or physical examination but progress to severe abnormalities such as airway obstruction from tracheal edema as late as 48 hours after the injury.
The esophagus is mobile and is usually collapsed as it courses through the neck but may be dilated while eating. This mobility helps protect the esophagus, but its delicate mucosal walls can be damaged easily by blunt traumatic events. Iatrogenic esophageal injuries can result from endoscopy, passage of a nasogastric or orogastric tube, vigorous suctioning, and difficult intubations. Esophageal injuries can also be seen with ingested foreign bodies and caustic chemicals. The injuries, which can be subtle, occult, and difficult to diagnose, can lead to increased morbidity and mortality if not identified.
Isolated or concurrent hyoid bone injuries are also possible, but rare. The hyoid is mobile and fairly well protected, which explains the paucity of isolated injury. As with other injuries, these symptoms and signs can be subtle initially, with progressive edema and airway obstruction.
Vascular injuries are also rare with blunt trauma. These injuries are often unsuspected and undiagnosed on routine examination. Risk factors for injury have been reported to include Glasgow Coma Scale score of less than 8; head injury; basilar skull fracture; and facial, neck, thorax, or abdominal injury. The most common vascular structure injured with blunt trauma is the common carotid artery. The vertebral arteries are rarely injured by blunt forces unless a concurrent transverse process or other cervical spine fracture occurs. Atlantooccipital dislocation can also be associated with vertebral artery injury, which if occurs frequently leads to early death in the field. Vascular contusions with intimal damage may also be seen with blunt neck trauma.
The glandular structures in the neck, including the thyroid, parathyroid, parotid, and submandibular glands, may also be injured. While these organs may be traumatized, they are rarely completely destroyed.
Clinical Considerations
Clinical Recognition
In the presence of blunt neck trauma, the triad of dyspnea, stridor, and hemoptysis suggests laryngeal injury. Injuries above the glottis often demonstrate cervical emphysema, dysphagia, hoarseness, and progressive airway obstruction, whereas those below present with hemoptysis and persistent air leak, although any or all symptoms and signs listed in Table 120.3 may be present. If a laryngeal injury is noted, the patient should be evaluated carefully for other commonly associated injuries, including in the cervical spine, chest, face, pharyngoesophageal area, and recurrent laryngeal nerve palsy.
Symptoms and signs of hyoid injury include pain in the throat that worsens with swallowing or coughing, tenderness to palpation, neck crepitus, pain on head rotation, dysphagia, dyspnea, or dysphonia.
The symptoms and signs associated with esophageal injury are listed in Table 120.3 and include neck tenderness and pain, dysphagia, odynophagia, drooling, crepitus, subcutaneous emphysema, hematemesis, fever, and mediastinitis (see Chapters 52 Pain: Dysuria, and 89 Head Trauma).
The clinician must consider subclavian or innominate vessel injuries if a fracture of the clavicle or first rib is identified.
Patients with signs or symptoms of facial or neck burns will require careful assessment, as airway edema may initially be subtle but progress rapidly. Early recognition and protection of a difficult airway is paramount.
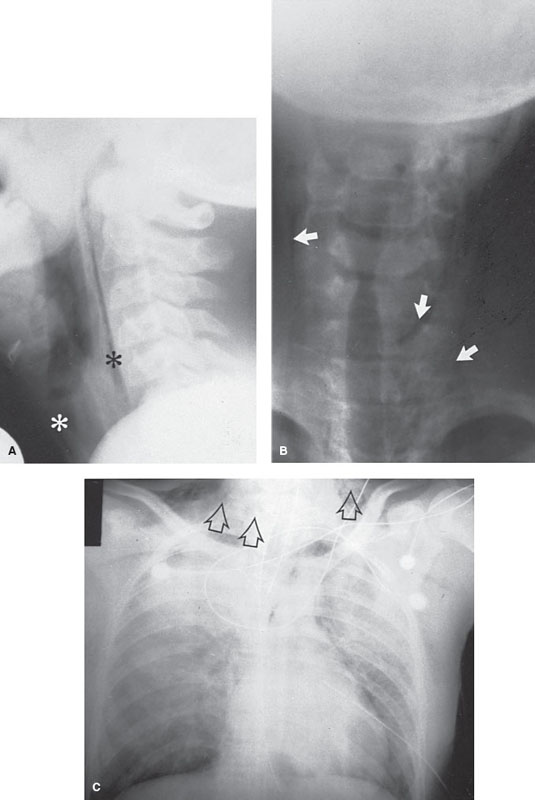
FIGURE 120.9 A–C: Subcutaneous emphysema (asterisks and arrows) of neck and chest in 11-year-old patient from barotrauma sustained when opening carbonated beverage container with teeth.
Triage Considerations
These patients require expedited evaluation, close monitoring and providers should anticipate difficult airway management. Early transfer to a pediatric trauma center should be considered if appropriate surgical or critical care staff is not available.
Clinical Assessment
As with all trauma patients, initial rapid assessment of their airway, breathing, and circulatory status should be completed. Given the risk of airway injury, particular attention must be paid to subtle signs and symptoms of airway injury (Table 120.3). Continued monitoring with repeat examinations is important in the recognition and identification of vascular and neurologic injuries (Table 120.3). Refer to penetrating trauma clinical assessment section for detailed recommendations.
Management
Blunt neck trauma requires similar vigilance and potentially, similar diagnostic modalities as penetrating trauma. Refer to penetrating trauma section for management recommendations. Special management considerations are included here.
Early airway management should be considered for patients with facial and neck burns, including from ingested caustic substances. For circumferential burns, an escharotomy may be indicated which involves a vertical incision from the chin to the superior aspect of the sternal notch. This should only be performed by an experienced provider familiar with pediatric neck anatomy (see Chapter 112 Burns).
In blunt trauma, progressive onset pain, irritability, and signs of cord compression may suggest a spinal (usually venous) epidural hematoma. Rapid assessment by CT or MRI, followed by surgical intervention, will help ensure optimal outcome.
Clinical Indications for Discharge or Admission
The patient can be discharged if they do not have a significant injury, are hemodynamically stable, without any airway compromise, able to tolerate oral intake to maintain their hydration, and no indication or risk of abusive trauma or neglect is present. Otherwise, admission is indicated.
CERVICAL SPINE TRAUMA
Goals of Treatment
The goals are to identify cervical spine injury and prevent progression of secondary injury by applying the principles of spine immobilization and acute trauma resuscitation to maintain adequate ventilation, oxygenation, and hemodynamic status.
CLINICAL PEARLS AND PITFALLS
• Cervical spine injuries are uncommon in children but account for the majority of vertebral injuries in children.
• Younger children tend to have higher proportion of upper cervical spine injuries (C1–C4) due to the higher fulcrum of the immature spine, dislocations instead of fractures, and spinal cord injury without radiographic abnormality (SCIWORA).
• Children with congenital spine abnormalities, osseous weakness, or ligamentous instability are at increased risk for spinal injury.
• Airway management should be accomplished with simultaneous stabilization of the cervical spine.
Current Evidence
Cervical spine injuries are uncommon in children, occurring in an estimated 1% to 2% of patients with multiple trauma. Most injuries are a result of blunt forces due to motor vehicle crashes, followed by fall, sport-related injuries, and nonaccidental trauma. Mechanism of injury also varies by age. In a 2014 study, nonaccidental trauma was responsible for 38% of spinal injuries among children 0 to 2 years of age with 73% within the cervical spine, as common a mechanism as motor vehicle collisions in this age group; where as in older children sports-related injuries accounted for as many cervical spine injuries as motor vehicle collisions.
It is estimated that 5% of all spinal injuries occur in children younger than 16 years. However, approximately 72% of spinal injuries in children younger than 8 years occur in the cervical region. Certain pre-existing conditions (Down, Maroteaux–Lamy, Morquio’s, Grisel, and Klippel–Feil syndromes; achondroplasia; congenital cervical stenosis; Chiari malformation; rheumatoid disease; and acute soft tissue or bony infection or infiltration) may result in a cervical spine more predisposed to injury with minor or more significant trauma. Neurologic sequela may also occur in pediatric patients undergoing spinal manipulation for therapeutic purposes. Neonatal spinal injury may result from birth-associated trauma and is reported in approximately 1 in 60,000 births. These patients often have a history of cephalic forceps use during delivery and may have presenting signs that include weakness, flaccid quadriplegia, spinal shock, and apnea. These birth-related injuries carry high morbidity and mortality.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







