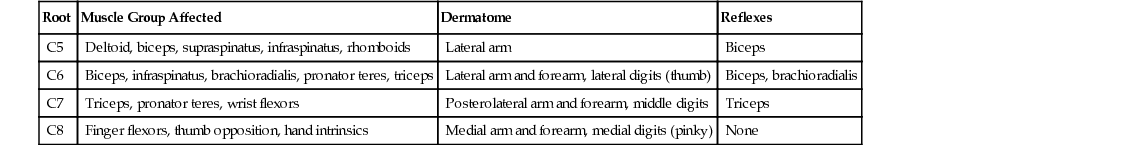
Zacharia Isaac, Sharon Alzner, María I. Bascarán Neck pain is a common complaint in primary care practices because most people are likely to have some degree of neck pain in their lifetime. The annual prevalence among adults exceeds 30%, and 33% to 65% of these patients are recovered at 1 year.1 In addition, of those who experience neck pain, 50% to 75% will experience another episode 1 to 5 years later. Neck pain is the fourth leading cause of disability.1 There are several identifiable sources of neck pain, including the bone, disks, joints, ligaments, fascia, muscles, and nerve roots. Pain can be experienced solely in the neck or can move into the head, shoulders, or arms and can start without an inciting event. If an episode of neck pain lasts longer than 12 weeks, it is typically defined as chronic neck pain. Chronic neck pain can also occur after a hyperextension injury (whiplash), usually in a motor vehicle collision or sometimes during work or sporting events. In chronic whiplash injury, many structures may be involved, including but not limited to the intervertebral disks; facet joints; ligaments; and other cervical soft tissues. Risk factors for neck pain include manual labor occupations, female gender, headaches, smoking, poor job satisfaction, and poor biomechanics. The cervical spine is made up of seven cervical vertebrae, C1 through C7. The C2 through C7 bodies are separated by five intervertebral disks, giving this portion of the spine a natural cervical lordosis. Each intervertebral disk consists of a gelatinous nucleus pulposus, surrounded by the fibrous rings of the anulus fibrosus. The nucleus pulposus consists of water, proteoglycans, and collagen. At birth it is 90% water, and it degenerates with time. These disks allow dissipation of axial loading forces throughout various ranges of motion; with degeneration over time, they can cause mechanical bilateral or midline neck pain. The support of the cervical spine comes from the various ligamentous, articular, and muscular structures, which can also be pain-mediating structures. The uncovertebral articulation is an important structure in the cervical spine and represents an area of vertebral and disk articulation in the cervical neural foramen. The degenerative hypertrophy of this area and the resultant narrowing of the neural foramen commonly result in radicular pain. Cervical sprains and strains can be caused by overstretching or tearing of spinal ligaments and muscles. In the acute phase of neck pain without neurologic symptoms, the diagnosis of cervical sprain and strain is often made without an inciting event, and the precise diagnosis is not evident. Cervical sprains and strains commonly occur after automobile accidents, trauma, or other injuries. In addition, motor vehicle accidents and associated whiplash injuries have been known to cause upper cervical facet joint–mediated pain. These occur most frequently as a result of rear-end or side-impact motor vehicle collisions. There are well-described sclerotomal referral patterns for neck pain arising from the facet joints, with the pain extending into the head and shoulders, either unilaterally or bilaterally. Cervical radiculopathy can typically cause neck pain extending into the arm. The pain pattern is usually worse in the arm than in the neck with associated neurologic symptoms, such as weakness, numbness, and tingling. One common cause of radicular neck pain is a herniated cervical intervertebral disk (most commonly at the C6-7 followed by the C5-6 level). Herniated disk material has been shown to be inflammatory in nature and produces phospholipase A2, a key mediator in the arachidonic acid cascade. Cervical spondylosis can also result from uncovertebral hypertrophy and is also a common cause of cervical radiculopathy. As the disks degenerate with time, there can be small herniations that calcify, causing disk osteophyte complexes to form. These complexes, combined with the ligamentous hypertrophy and loss of disk height that occur with aging, can cause impingement of nerve roots with resultant radicular pain.2 Cervical myelopathy caused by spinal cord compression is a possible complication of cervical spondylosis and can manifest with neck pain, radicular extremity pain, loss of manual dexterity, globally referred symptoms, gait instability, bowel or bladder dysfunction, and progressive weakness. Such symptoms warrant further diagnostic evaluation with magnetic resonance imaging (MRI) of the cervical spine if there is no contraindication. A thorough history, including past medical, social, occupational, and family history, as well as a review of systems, including constitutional symptoms, skin changes, visceral pain, neurologic changes, and bowel or bladder complaints, should be performed. In addition, any history of previous trauma or whiplash should be elicited. Details surrounding the onset of pain, location and radiation of the pain, quality of pain over time, aggravating and alleviating factors, and associated symptoms such as headaches or systemic symptoms should be sought. Psychosocial elements including psychological and occupational history should also be evaluated to look for any confounding variables. The location and radiation of pain can help elucidate the cause. Neck pain that remains in the neck region without radiation into the arms is typically referred to as axial neck pain. This pain can result from a cervical sprain or strain or be referred from the intervertebral disks or facet joints. Neck mobility may be limited from many of these causes; however, certain maneuvers can help elucidate the painful source. With axial neck pain, the motor strength and reflex examination findings are normal. Radicular neck pain is usually described as pain greater in the arm than in the neck but commonly occurring in both. Neurologic symptoms, such as pain, weakness, numbness, and tingling, can also be found in the affected spinal nerve root distribution. The patient will likely report a relatively abrupt onset of pain that may worsen with particular movements, including cervical extension and ipsilateral rotation. In addition, a patient may have the arm in a position that decreases neural tension on the nerve root. This usually involves placing the upper arm closer to the head either in an overhead position or crossed in front of the throat. If the patient has any neurologic symptoms, such as weakness in the lower extremities, gait disturbance, bowel or bladder dysfunction, or sexual dysfunction, cervical myelopathy should be considered and immediately evaluated. Facet joint pain is also a cause of axial neck pain and has been associated with whiplash injuries and headaches. Whiplash injury is experienced with an abrupt flexion-extension type of injury. Pain is typically off the midline, and although there are defined sclerotomes for referral, pain is usually worse in the neck. The pathophysiologic mechanism for whiplash syndrome is unclear; however, it is thought to be caused by soft tissue injury with local release of inflammatory mediators. The cervical zygapophyseal joints have been implicated as the major source of chronic pain after whiplash.1 Significant biomechanical and psychosocial factors play a role, and severity of acute symptoms, comorbid depression, anxiety, and not being at fault for the accident are poor prognostic factors. Physical examination starts with careful observation of the patient, looking for cervical alignment, discomfort, and frequent position changes and evaluating the patient’s affect. Gait should be examined for unsteadiness, spastic or mechanical movement, and widened or narrowed steps. The skin and vascular system should be appraised for medical causes of neck pain, including meningitis, dental or jaw pain, and malignant neoplasm. Cervical range of motion should be determined. It should be noted whether the patient moves in a limited, guarded fashion or if there is an ease to the movement. The normal range of motion of the cervical spine is 90 degrees of rotation, 45 degrees of lateral tilt, 60 degrees of forward flexion, and 75 degrees of extension. The patient should be inspected for loss of cervical lordosis and atrophy of the paraspinal, periscapular, and arm muscles. Palpation of the paraspinal muscles and trapezius muscles should be performed to assess for the degree of tenderness, although positive findings of pain are nonspecific in nature and can be related to many causes of axial neck pain. The facet joints should also be palpated to reproduce the patient’s typical symptoms. Neurologic examination should include manual muscle strength testing, sensation, and reflexes and evaluation for upper motor neuron signs. Examination and manual muscle strength testing (shoulder elevation, abduction, and internal and external rotation; elbow flexion and extension; wrist extension and flexion; and hand and digit intrinsic muscles) may help define the involved dermatome (Table 183-1). In addition, sensation to both light touch and pinprick should be checked for deficits throughout the dermatomes. Reflexes should also be elicited at the biceps, triceps, and brachioradialis tendons bilaterally to look for asymmetry or hyperreflexia. The Babinski response and Hoffmann sign as well as evaluation for both clonus and muscle spasticity can determine if central nervous system involvement of the brain or spinal cord is occurring. Provocative maneuvers such as the modified Spurling maneuver, when it is performed and the response is positive, can be suggestive of cervical spinal nerve root involvement (high sensitivity, low specificity). This test is performed by placing the head in extension, lateral flexion, and ipsilateral rotation. With placement of an axial load on the head, reproduction of typical symptoms down the arm can be specific for cervical radiculopathy.3 The Elvey upper limb tension test is performed by turning the head contralaterally with the arm abducted and elbow extended; a positive test response is reproduction of arm symptoms.3 The Lhermitte sign can also be elicited by rapidly flexing the neck while the patient is seated.2 This can produce an electric shock sensation down the spine and into the limbs; the response is positive with cervical cord disorders such as compression, tumor, and multiple sclerosis. In addition to cervical causes of neck pain, the provider should evaluate for other mimicking disorders. The Adson test for vascular thoracic outlet syndrome is done with the patient standing. The examiner palpates the radial pulse while moving the upper extremity in abduction, extension, and external rotation as the patient rotates the head toward the ipsilateral side with the breath held.2 If the patient’s pulse diminishes, this is considered a positive test result; however, this finding is often nonspecific. Mechanical shoulder disorders can also refer pain in a distribution similar to that of the cervical spine. Shoulder examination should also be performed to ensure that there is no shoulder disorder that is mimicking or contributing to neck pain symptoms. • Plain radiographs of the cervical spine are warranted if the patient has a history of cancer, recent trauma, long-standing corticosteroid use, osteoporosis, drug or alcohol abuse, or concerning constitutional or neurologic symptoms. When a patient visits the clinic with cervical spine pain after trauma or a motor vehicle accident, the Canadian Cervical Spine Rule, when used correctly, is helpful in identifying those patients who are at high risk for a cervical spine fracture and should therefore undergo cervical radiography.4 The Canadian Cervical Spine Rule has been validated with high sensitivity using CT scan as the gold standard, is superior to the National Emergency X-Radiography Utilization Study (NEXUS) Low-Risk Criteria, and results in reduced rates of radiography.5,6 • If the patient has neurologic findings, symptoms concerning for medical causes of pain, occult fracture, or persistent pain after conservative treatment, further imaging is warranted. Computed tomography (CT) scans or MRI can be considered. • MRI is the most widely used imaging modality to evaluate for neck pain and radiculopathy. Its principal use is to evaluate the bone structures and soft tissues, and it can be helpful in identifying degenerative disk disease, annular tears, disk herniations, spinal stenosis, and cord or nerve root compression. With the addition of gadolinium, it can be used to look for tumor or infection. Although it is superior at evaluating degenerative changes in the spine, there is a high likelihood that many findings are asymptomatic and may not be the source of the patient’s pain. MRI studies have revealed that 19% of asymptomatic patients have anatomic abnormalities such as cervical disk herniations without any reported neck pain or radicular symptoms.7 • Other diagnostic workup can be included for more patient-specific situations. • Electrodiagnostic studies can be helpful in distinguishing neurologic changes with denervation and reinnervation from subacute and chronic radiculopathy.8 These studies will not show acute changes until approximately 3 to 4 weeks after the initial insult; however, needle electromyography (EMG) can highlight chronic changes with good sensitivity and high specificity.8
Neck Pain
Definition and Epidemiology
Pathophysiology
Clinical Presentation
Physical Examination
Diagnostics
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Neck Pain
Chapter 183