MUSCULOSKELETAL TRAUMA
RACHEL W. THOMPSON, MD, YOUNG-JO KIM, MD, PhD, AND LOIS K. LEE, MD, MPH
GENERAL PRINCIPLES OF PEDIATRIC ORTHOPEDICS
Goals of Emergency Therapy
Orthopedic trauma currently accounts for 10% to 15% of emergency department (ED) visits in urban pediatric hospitals. The number and spectrum of musculoskeletal injuries sustained by children and adolescents appear to be on the rise since the mid-1990s, in part because of the rapid growth of organized sports and other youth recreational activities. As a consequence of their skeletal immaturity and the associated anatomic and physiologic differences in bony structure, pediatric standards of care, fracture patterns, and outcomes are different than in the adult population. Thus, the emergency clinician must maintain a high level of suspicion for fracture in the child presenting with focal bony pain, even in the absence of obvious deformity. Priorities in the emergency care of these patients include the recognition and treatment of pain by both pharmacologic and other comfort measures, and the consideration of using minimal radiation when possible, given the evidence of the inverse correlation of age and risk of radiation-associated malignancy. Finally, emergency care is performed with the ultimate goal of preserving long-term function. This requires recognizing and addressing factors that may otherwise lead to complications, such as neurovascular compromise, open injuries at risk for infection, and physeal injuries that may lead to growth disturbance.
KEY POINTS
 Injury frequency increases with increasing age as children become more mobile.
Injury frequency increases with increasing age as children become more mobile.
 The anatomy and physiology of the immature skeleton results in unique pediatric fracture patterns including greenstick, torus (buckle), and physeal (growth plate) fractures.
The anatomy and physiology of the immature skeleton results in unique pediatric fracture patterns including greenstick, torus (buckle), and physeal (growth plate) fractures.
 Pediatric bones have less tensile strength than the attached ligaments, resulting in higher rates of fracture from mechanisms that would produce a sprain or dislocation in skeletally mature bone.
Pediatric bones have less tensile strength than the attached ligaments, resulting in higher rates of fracture from mechanisms that would produce a sprain or dislocation in skeletally mature bone.
 In addition to examination of the injured extremity with inspection, palpation, range of motion (passive and active), and neurovascular examination, there should also be a careful examination of the joints proximal and distal to the point of maximal tenderness.
In addition to examination of the injured extremity with inspection, palpation, range of motion (passive and active), and neurovascular examination, there should also be a careful examination of the joints proximal and distal to the point of maximal tenderness.
 The Salter–Harris classification of physeal injuries describes five types of injuries involving the physis and provides important prognostic information.
The Salter–Harris classification of physeal injuries describes five types of injuries involving the physis and provides important prognostic information.
 Weight-based dosages for pain control should be provided for all pediatric fracture patients both in the ED and once discharged home.
Weight-based dosages for pain control should be provided for all pediatric fracture patients both in the ED and once discharged home.
RELATED CHAPTERS
• Cardiopulmonary Resuscitation: Chapter 4
• Interfacility Transport and Stabilization: Chapter 6
Signs and Symptoms
• Injury: Shoulder: Chapter 38
Medical, Surgical, and Trauma Emergencies
• Child Abuse/Assault: Chapter 95
• Musculoskeletal Emergencies: Chapter 129
• Procedural Sedation: Chapter 140
GENERAL PRINCIPLES AND PROPERTIES OF PEDIATRIC FRACTURES
Goals of Treatment
The anatomic and physiologic differences between adults and children are reflected in the different types of fractures and injuries unique to the pediatric age group, including physeal fractures, torus fractures, greenstick fractures, bowing deformities, and avulsion fractures. The emergency clinician must have an understanding of the properties of pediatric bone that result in these unique fractures. With this foundation, the provider can more accurately make the diagnosis and avoid potential complications and missed injuries.
Anatomy and Physiology of Pediatric Bone
CLINICAL PEARLS AND PITFALLS
• During periods of growth, the regions of the pediatric skeleton undergoing rapid metabolic activity are more susceptible to fracture.
• Fracture remodeling in pediatric patients is robust and allows for more angulation at the time of casting, and less frequent operative repair than adult fractures.
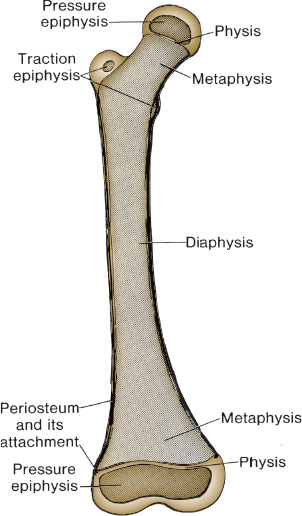
FIGURE 119.1 Diagrammatic representation of the femur in late childhood.
Current Evidence
The basic bony architecture in children includes a thick and active periosteum, a growth plate (physis), an epiphysis (secondary ossification center), and perichondrial rings (Fig. 119.1). Structurally, the bones of a child are much more porous and pliable than those of an adult. As a result, overall bony strength is less, and the incidence of fractures is greater in children than in adults. Moreover, ligaments have greater strength than the physes and perichondrial rings; thus, a child is more likely to suffer a fracture from an injury that, in a skeletally mature individual, would result in a sprain, ligamentous injury, or dislocation.
Unlike in adults, remodeling and anatomic fracture union for pediatric fractures is the expectation rather than the exception. In general, significant remodeling can be anticipated both in younger children and when the fracture occurs in the metaphysis of growing bones. The greatest degree of remodeling is anticipated with bony injuries occurring in the plane of motion of the adjacent joint. In contrast, the injuries least likely to correct without intervention include those that occur in the diaphysis of long bones in adolescents, those with bowing greater than 10 degrees, and fractures with rotational malalignment. In general, the goal is to obtain as near an anatomic reduction of the fracture fragments as possible in all age groups and not to rely on remodeling to align angulated fractures; however, relative guidelines for acceptable angulation by age are provided.
Physeal Fractures
 Salter–Harris type I injuries are frequently diagnosed clinically by point tenderness at the physis and may not be evident radiographically.
Salter–Harris type I injuries are frequently diagnosed clinically by point tenderness at the physis and may not be evident radiographically.
 Selective use of radiographs of the contralateral extremity may help with diagnosing physeal injury.
Selective use of radiographs of the contralateral extremity may help with diagnosing physeal injury.
 An important complication of physeal fractures is growth disturbance, which may result in angular deformity, limb length discrepancy, and/or epiphyseal distortion.
An important complication of physeal fractures is growth disturbance, which may result in angular deformity, limb length discrepancy, and/or epiphyseal distortion.
 Orthopedic referral is an important component of management and follow up for these injuries.
Orthopedic referral is an important component of management and follow up for these injuries.
The physis is the transition zone between the metaphysis and the epiphysis. In assessing young children with musculoskeletal trauma, the clinician must be attuned to the possibility of fractures occurring at the physis (growth plate), which may not be readily apparent on plain film. These relatively common injuries generally occur through the zone of provisional calcification, a relatively weak area of the germinal growth plate that becomes even more susceptible to injury during periods of growth in adolescence (peak incidence at 11 to 12 years of age). Most growth plate injuries occur in the upper limb, particularly in the radius and ulna.
Several classification systems have been described for physeal fractures. The most widely used is that of Salter and Harris, who described five types of growth plate fractures, each having specific prognostic and treatment implications (Fig. 119.2).
Salter–Harris type I fracture. This fracture type is a separation of the metaphysis from the epiphysis through the zone of provisional calcification resulting in a widening of the physeal space. Diagnosis may be challenging if displacement is minimal. Radiographs may only show associated soft tissue swelling. Type I fractures are generally benign, and growth disturbance is uncommon if near-anatomic reduction is achieved. Exceptions include type I injuries of the proximal and distal femur and the proximal tibia, which are subject to premature physeal closure and posttraumatic growth arrest. In general, when radiographic studies are negative, but physical examination findings are suggestive of a Salter–Harris type I injury (e.g., point tenderness over a growth plate), immobilization and a follow-up examination are essential. Imaging showing periosteal reaction along the physis 7 to 10 days after possible Salter–Harris fractures may help diagnose the occult injury.
Salter–Harris type II fracture. Type II fractures are the most common type of pediatric physeal fracture. These fractures extend through both the physis and the metaphysis. Like the type I injuries, these fractures generally carry a good prognosis and rarely cause functional deformity.
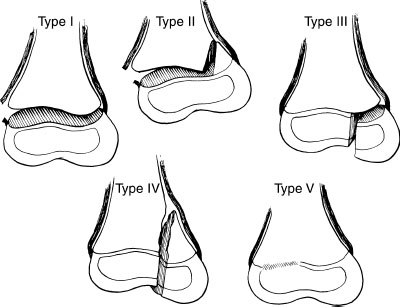
FIGURE 119.2 The Salter–Harris classification for physeal fractures. The prognosis for growth disturbance worsens from type I through type V.
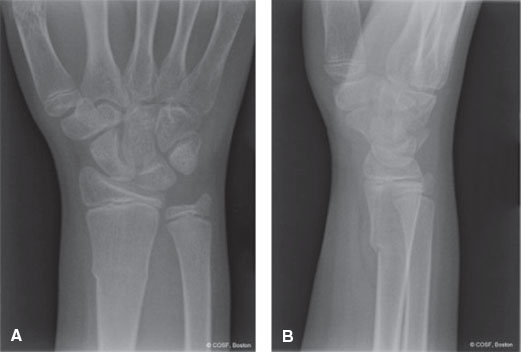
FIGURE 119.3 Anteroposterior (A) and lateral (B) radiographs of a distal radius torus fracture. (From Flynn JM, Skaggs DL, Waters PM. Rockwood and Wilkins’ fractures in children. 8th ed. Philadelphia, PA: Wolters Kluwer, 2014.)
Salter–Harris type III and IV fractures. Type III and IV injuries are growth plate injuries that involve the intra-articular surface. In type III fractures, the fracture line typically extends from the epiphysis into the physis, resulting in a separation of the epiphysis and its associated growth plate from the rest of the epiphysis. The fracture line in type IV injuries crosses through all three regions of the bone (epiphysis, physis, and metaphysis). Anatomic position must be reestablished to restore normal joint mechanics and prevent growth disturbance. Because of these risks, which may result in functional disability, orthopedic consultation should be obtained while the patient is in the ED for all but the most minor type III and IV injuries.
Salter–Harris type V fracture. Type V fractures are the least common physeal fracture, and most commonly occur at the knee and ankle. These fractures are a crushing injury of the growth plate as a result of axial compression. It is often difficult to diagnose these injuries during the ED presentation, but a high index of suspicion should be maintained if there is a concerning mechanism or presence of a joint effusion in the absence of radiographic abnormalities of the bone. These fractures have the worst prognosis for growth disturbance as the compressive force may result in premature closure of the physis. Unfortunately, the diagnosis is often made in hindsight after a growth arrest becomes evident.
Torus Fractures
Torus (buckle) fractures are common fractures in young children. They most often occur at the junction of metaphysis and diaphysis from a compressive load. The cortex of the bone buckles in a small area, resulting in a stable fracture pattern (Fig. 119.3). As the child matures, the stiffness of the metaphyseal region increases, and the incidence of this fracture pattern decreases.
Greenstick Fractures
The composition of pediatric bones makes them less likely to propagate the force of injury into comminuted fragments. Thus, with greenstick injuries, the bone bends before it breaks, with the thick and active periosteum remaining intact on one cortex and acting like a hinge: torn on the convex side of the fracture while remaining intact on the concave side. The intact cortex thus maintains apposition at the site of fracture; however, to obtain an anatomic reduction, the fracture must often first be completed. The emergency clinician must be attuned to this injury as inadequate reduction of the deformation or bowing of the bone can result in an abnormal growth pattern and loss of function (Fig. 119.4).
Bowing Fractures
Bowing fractures occur uniquely in children. Evidence suggests that the mechanism is a longitudinal force causing “plastic” deformation (bowing), but stops short of creating a fracture (Fig. 119.4). Little remodeling can be expected from the injury, and both cosmetic and functional deficits are common. Anatomic reduction produces the most satisfactory result. All bowing deformities should be referred to an orthopedic surgeon.
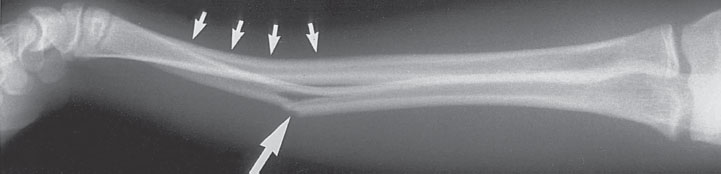
FIGURE 119.4 Greenstick fracture of the ulna (large arrow) and a bowing fracture (small arrows) of the radius. The extent of bowing can often be fully appreciated only with comparison views of the opposite extremity.
Avulsion Fractures
The frequency of avulsion fractures in pediatrics is a consequence of the strong muscular attachments to relatively weak secondary centers of ossification in the developing skeleton known as apophyses. During intense muscular contraction, fractures can occur through the apophyseal plate. Common sites include the pelvis, tibial tubercle, and the phalanges. Avulsion fractures infrequently require open or closed reduction. Conservative care is the mainstay of treatment.
GENERAL PRINCIPLES OF ACUTE ORTHOPEDIC CARE
CLINICAL PEARLS AND PITFALLS
• Any child with obvious extremity deformity should be made nil per os (NPO) at triage given the potential need for procedural sedation or operative management for fracture reduction and casting.
• Based on the history and mechanism of injury, the possibility of other injuries (e.g., head, chest, intra-abdominal organs) should be considered.
• Physical examination must include inspection, palpation, range of motion (passive and active), and neurovascular examination with careful examination of the joints proximal and distal to the point of maximal tenderness.
• Always carefully remove all splints, bandages, and clothing in order to perform an accurate examination with documentation of breaks in the skin, which may represent a possible open fracture.
• Splinting the injured extremity immediately after evaluation and before radiographs are taken can decrease the child’s discomfort and prevent further injury.
• Neurovascular status should be assessed before and after any splinting is performed.
• If the orthopedist is not readily available, gentle longitudinal traction and gross realignment may be performed by the emergency clinician for fractures that are grossly displaced, unstable, or if there is vascular compromise.
Current Evidence
Rapid assessment and treatment of pain both in the ED and after discharge are key components of the emergency care of musculoskeletal trauma. Increasingly, triage protocols include the administration of appropriate oral analgesics prior to physician care. For significantly painful injuries, clinicians should consider intranasal fentanyl, which has the advantage of a relatively fast onset of action (<5 minutes) without requiring an IV. With this initial pain control in place, an IV can then be placed for intravenous narcotics if clinically indicated.
After discharge from the ED, children experience the most fracture pain in the first 3 days. Ibuprofen, acetaminophen, or oxycodone is recommended for pain control at home. Those requiring narcotics for pain control while in the ED and those children discharged overnight (between 10 PM and 8 AM) have an increased risk of having more pain, and these children may benefit from having a prescription for oral narcotics to be taken at home for pain. Acetaminophen with codeine is no longer recommended due to the variable metabolism of codeine in different populations, leading to either ineffective pain control or the risk of respiratory compromise.
Goals of Treatment
A systematic approach to the evaluation and management of pediatric musculoskeletal injuries is important in order to avoid overlooked injuries and prevent potential complications. The initial goals of treatment in the ED are to provide pain control, evaluate the injured extremity for any neurovascular compromise, and immobilize the injured area. Next, the specific injury must be identified with physical examination and radiologic imaging. The injured extremity should be immobilized to enhance comfort and prevent further trauma until definitive orthopedic care can be obtained. Adjunctive interventions such as elevating the injured extremity and applying a cold pack can help mitigate swelling.
Clinical Considerations
Clinical Recognition
A history of a traumatic event with physical examination findings of a painful extremity or body part with swelling, or deformity or the inability to use the extremity allows for rapid recognition of a musculoskeletal injury. Less severe injuries may be more difficult to diagnose as they may present with only mild swelling or a history of not using the extremity normally. For long bone injuries, the joints above and below the injured extremity must be examined for possible associated injuries.
Triage Considerations
Children presenting with significant pain or with a grossly deformed extremity should be evaluated immediately by the emergency clinician. A focused neurovascular assessment should be performed. Those children with a more subacute presentation (e.g., trauma occurred the day prior), and those with minimal pain may be seen less urgently.
Clinical Assessment
The injured extremity should be inspected for swelling and deformity, and the joints above and below the injury should be examined. The skin should be examined for ecchymosis, abrasions, lacerations, soft tissue defects, or exposed bone. If an open wound is present, the location, degree of contamination, and rate of active bleeding should be documented. The neurovascular status should be determined by examining the motor and sensory function distal to the fracture site. The pulses should be palpated and capillary refill assessed.
Management
Imaging. In addition to the physical examination, the history and knowledge of the most common injuries for a specific age group can guide the choice of radiographic studies. The radiographs should include the joints proximal and distal to the fracture and should include at least two views taken at 90 degrees to one another (i.e., anteroposterior and lateral views). When routine views do not identify a fracture, but clinical suspicion is high, oblique or other additional views may be useful. With the degree of normal variability, especially with the immature bone, comparison views of the contralateral extremity may be helpful to determine if a radiographic finding is a traumatic injury or normal anatomy.
In addition to plain radiography, advanced imaging may be indicated for further evaluation of the injury. For complex, intra-articular, or spine injuries, computed tomography (CT) is often used. Although not commonly used in the ED, magnetic resonance imaging (MRI) is also used for the evaluation of physeal injuries as well as the diagnosis of avulsion and stress fractures, as it can visualize cartilaginous and soft tissue structures as well as osseous ones. The use of ultrasound in the ED setting is also expanding, both for diagnosis as well as to guide closed fracture reduction.
Immobilization. Paired with pain control, immobilization is fundamental to the initial treatment of fractures. Either plaster or fiberglass may be used to immobilize the fractured bone as well as the joints above and below the fracture. Immobilization provides pain control and helps to prevent further injury. The application of several layers of padding material before the splint or cast is placed is important for comfort and to decrease neurovascular compromise from swelling of the extremity (see Chapter 141 Procedures, section on Splinting of Musculoskeletal Injuries). The decision for the emergency clinician to splint or place a circumferential cast depends on the degree of actual or anticipated swelling, the risk for compartment syndrome, and the training of the provider.
Pain Control. At triage, pain management can begin with oral analgesics (e.g., ibuprofen, acetaminophen), either given alone or in combination. For injuries with more significant pain, intranasal fentanyl or intravenous narcotics may be administered. In addition, local and regional anesthesia blocks may be used based on the injury location. When fracture reduction is performed in the ED, procedural sedation with nitrous oxide or intravenous agents should be used by appropriately trained personnel (see Chapter 140 Procedural Sedation).
Orthopedic Consultation and Referral. When consulting the orthopedic surgeon, the emergency clinician needs to present accurate and descriptive information about the injury so the orthopedist can make appropriate treatment recommendations. The initial communication should include patient’s age and gender, mechanism of injury, anatomic location, neurovascular status, and extent of soft tissue injury. The radiographic description should note the anatomic location of the fracture, the type of fracture (e.g., transverse, spiral, oblique), amount of displacement, degree of angulation, shortening, or malrotation, degree of comminution, and the extent of involvement of the joint and physis (Fig. 119.5). Displacement for long bone fractures is commonly described using the approximate percentage of the shaft width displaced. Angulation is measured by drawing one line along the proximal fracture fragment as the reference and another line along the distal fracture fragment. The angle measured between the axes of those two lines describes the degree of angulation of the fracture.
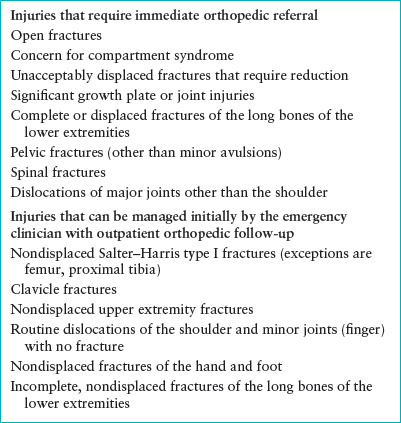
Indications for orthopedic consultation will vary with the ability and experience of the emergency clinician and availability of the orthopedist. Emergent orthopedic consultation is required to evaluate open fractures, those that are significantly displaced, or if neurovascular compromise is present. Orthopedic consultation is also recommended during ED visits for pelvic fractures (other than avulsions), spinal injuries, and dislocations of major joints (other than the shoulder). Referral to see an orthopedist as an outpatient within 24 to 48 hours is recommended for any growth plate or intra-articular fractures that have more than 2 to 3 mm of displacement and for fractures of the lower extremity long bones, as long as the extremity is neurovascularly intact and pain is adequately controlled. Physeal injuries begin healing quickly; therefore, urgent orthopedic referral is important to ensure adequate reduction of any displaced fractures within a safe time period. Referral for outpatient orthopedic follow-up after initial ED management is recommended for (1) most nondisplaced Salter–Harris type I fractures, (2) nondisplaced upper extremity, foot, and phalangeal fractures, (3) incomplete, nondisplaced fractures of the lower extremity long bones, and (4) reassessment of reduced routine dislocations of the minor joints and shoulder (Table 119.1).
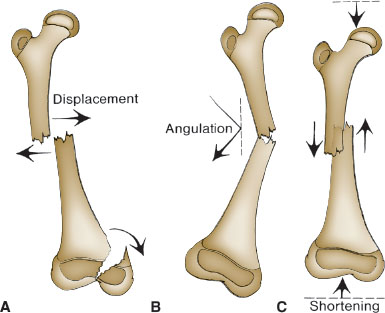
FIGURE 119.5 Diagrammatic representation of fracture deformities: displacement (A), angulation (B), and overriding with shortening (C).
TABLE 119.1
INDICATIONS FOR ORTHOPEDIC REFERRAL
Disposition
Open fractures, those associated with neurovascular compromise, those at high risk for the development of compartment syndrome, or fractures requiring intravenous medication for pain control should be admitted to the hospital for further orthopedic management. Non/minimally displaced fractures, well-reduced fractures, as well as successfully reduced dislocations of the minor joints and shoulder, may be discharged home after immobilization. Discharge instructions should include guidelines for pain control such as elevation and ice/cold pack application to the injured extremity and the use of medications at home, including oral narcotics if necessary. In addition, written instructions should review signs and symptoms of neurovascular compromise, infection, compartment syndrome, and other emergent reasons to return to medical attention.
COMPLICATIONS OF FRACTURES: OPEN FRACTURES AND COMPARTMENT SYNDROME
Goals of Treatment
Rapid identification of a potential open fracture or compartment syndrome is important for urgent orthopedic consultation. Open fractures have an increased risk of infection; therefore, early wound management and prophylactic antibiotics in the ED are vital. Compartment syndrome, if not identified and treated, can progress to irreversible muscle and nerve damage. Early consultation with orthopedics is necessary for fasciotomy.
CLINICAL PEARLS AND PITFALLS
• The laceration associated with an open fracture should not be closed in the ED, even if the fracture is nondisplaced.
• Antibiotics should be administered as soon as possible to a patient with an open fracture to minimize risk of infection.
• Compartment syndrome associated with a fracture can occur in the forearm, hand, leg, or foot, with the leg being the most common fracture location.
• The fractures associated with compartment syndrome do not need to be severe.
• Pain out of proportion to the injury or increasing pain after analgesics, especially with passive extension, is one of the earliest signs of compartment syndrome.
• Compartment syndrome may present not only shortly after the fracture is sustained, but may also occur after reduction and casting. Therefore, neurovascular status must be checked in the injured extremity after casting.
• Fasciotomy should be considered when clinical symptoms of compartment syndrome are present and/or when compartment pressures measured in the injured extremity are within 30 mm Hg of the patient’s diastolic blood pressure or the mean arterial pressure.
Current Evidence
A fracture is considered to be “open” when the injury results in disruption of the skin and underlying soft tissues overlying the fracture, thus providing a communication between the fracture and the outside environment. The organisms found to be contaminating an open fracture at the time of presentation do not represent the microbes that will eventually cause infection; therefore, wound cultures are of minimal utility. Most open fracture infections are caused by gram-negative rods and gram-positive staphylococci; however, clinicians should be mindful of a rising frequency of infections caused by methicillin-resistant Staphylococcus aureus. While there is consensus supporting the administration of antibiotics as soon as possible to minimize risk of infection, there are variable recommendations on the optimal regimen.
Children with compartment syndrome may present with only one associated sign or symptom, with pain being the most common presentation. In one study of compartment syndrome with tibial shaft fractures, adolescents (14 years and older) had an increased risk of compartment syndrome compared with younger children.
Clinical Considerations
Clinical Recognition
Open fractures typically occur due to a high-energy mechanism; therefore, a complete examination to identify other potentially life-threatening injuries is imperative. A fractured extremity should be carefully examined for the presence of an open wound, potentially signifying an open fracture. However, it is not always obvious if the injury is an open fracture or if it is a laceration that does not communicate with the fracture. Operative exploration by the orthopedist may be necessary to determine this.
Compartment syndrome develops when there is an accumulation of intracompartmental pressure resulting in obstruction of venous outflow and then increased pressure in the nonelastic compartment. If untreated, small arterioles and capillaries are eventually occluded, resulting in ischemia with irreversible muscle and neurovascular tissue damage. Compartment syndrome must be suspected with any fracture or blunt tissue injury when there is pain out of proportion to the injury or if the pain is increasing, despite analgesic administration. The patient may also complain of paresthesias and pain with passive extension. On physical examination the patient may have pallor and pulselessness of the injured extremity, although these may be late findings.
Triage Considerations
Children presenting with a concern for an open fracture or compartment syndrome should be evaluated immediately in the ED with urgent orthopedic consultation.
Clinical Assessment
For open fractures, the wound should be carefully examined and considered in the context of the fracture location. With compartment syndrome, the extremity may be pale and the muscular compartments may be swollen and feel hard and tense. The pulses may be diminished or absent and the limb may have paralysis or muscle weakness. Children may present with only a single sign or symptom of compartment syndrome.
Management
Open wounds should be cleaned and a sterile dressing applied. The fracture should be immobilized. Prophylactic intravenous antibiotics should be administered, and tetanus prophylaxis should be given according to the usual guidelines. Current antibiotic recommendations are for the administration of early, systemic, wide-spectrum antibiotic therapy directed at gram-positive and gram-negative organisms. A commonly recommended regimen is for a first-generation cephalosporin (e.g., cefazolin) with the addition of an aminoglycoside (e.g., gentamicin) for larger open fractures (skin laceration >1 cm with significant soft tissue damage and contamination). As an alternative to aminoglycosides, a third-generation cephalosporin or other agent with activity against gram-negative bacteria may be selected. For injuries at high risk for anaerobic infection (e.g., occurring on a farm), clinicians should add ampicillin or penicillin. Urgent orthopedic consultation is necessary for surgical debridement, irrigation, and definitive care of the wound and fracture.
If there is suspicion for compartment syndrome, compartment pressures in the injured extremity should be obtained; however, this may be difficult in an awake young child, especially if less than 5 years old. Compartment pressures >30 mm Hg have been used to diagnose compartment syndrome. Newer approaches suggest that compartment pressures should be interpreted in the context of systemic blood pressures. Compartment pressures within 30 mm Hg of either the diastolic blood pressure or the mean arterial pressure are concerning for compartment syndrome. Urgent orthopedic consultation is necessary if there is any concern for compartment syndrome, which may require treatment with fasciotomy.
Disposition
All children with open fractures or with concern for/diagnosis of compartment syndrome should be admitted to the hospital for ongoing orthopedic care given the high risks for infection and neuromuscular injury.
MULTIPLE TRAUMA
CLINICAL PEARLS AND PITFALLS
• Shock is uncommonly caused by blood loss from a fracture, except in the setting of extensive pelvic fractures or multiple long bone fractures; therefore, the presence of other injuries should be evaluated if shock is present.
• After the initial trauma evaluation and resuscitation, a thorough secondary survey is important to identify other possible orthopedic as well as nonorthopedic injuries.
• Thoracic and lumbar spine fractures are challenging to diagnose by physical examination in the setting of multisystem trauma. If the injury mechanism or examination is concerning for possible spinal injury, radiographs should be obtained and careful immobilization maintained.
In the setting of multisystem trauma, fractures may be common and sometimes are the most obvious injury, but they are rarely life-threatening. The usual trauma evaluation and resuscitation protocol should be followed for any child with concern for multisystem trauma and/or a severe mechanism of injury. After the child has been stabilized, the injured extremity should be immobilized. For unstable pelvic injuries with associated bleeding, wrapping the pelvis tightly in a sheet or the application of an external fixator device may help tamponade the bleeding.
PHYSICAL ABUSE
CLINICAL PEARLS AND PITFALLS
• Spiral fractures and metaphyseal–epiphyseal injuries in nonambulatory children are highly suspicious for nonaccidental trauma (Fig. 119.6).
• onaccidental trauma should be considered for children with a fracture in the absence of a history of substantial trauma, or if any of the following are present:
• Multiple fractures, which may be in various stages of healing
• Delayed presentation with evidence of bone healing at time of ED visit
• Presence of rib fractures
• Femur fracture in a nonambulatory child
• Midshaft humeral fracture (less than 3 years old)
• History inconsistent with the developmental stage of the child
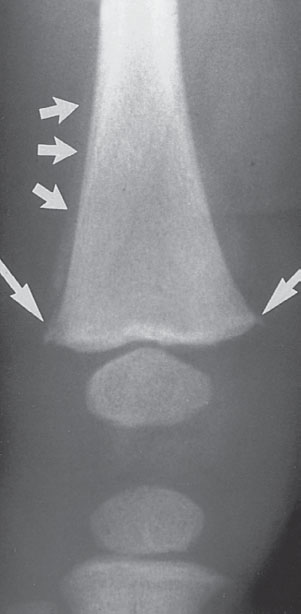
FIGURE 119.6 Radiograph of the right knee of a 3.5-month-old victim of physical abuse. The metaphyseal corner fractures (large arrows) are considered diagnostic of abuse. Also evident is periosteal new bone formation (small arrows), proof of a significant delay between injury and medical evaluation.
TABLE 119.2
FRACTURES STRONGLY SUGGESTIVE OF PHYSICAL ABUSEa
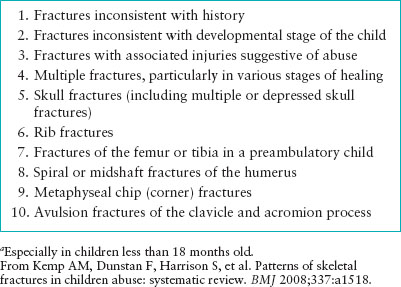
Among all childhood fractures, nonaccidental trauma accounts for a relatively small proportion of these injuries. However, of children who have been investigated for abuse, up to a third of these children have skeletal fractures (Table 119.2). These fractures may be occult, and usually occur in infants and toddlers. The presence of multiple fractures occurs more often with nonaccidental trauma. If there is suspicion for nonaccidental trauma as the cause of the fracture, a child protection team should be consulted for further evaluation and management, including the determination of need for a skeletal survey to assess for other occult fractures (see Chapter 95 Child Abuse/Assault).
PATHOLOGIC FRACTURES
A fracture that occurs through abnormal bone is considered a pathologic fracture (Figs. 119.7 and 119.8). The predisposing condition may not become apparent until after the fracture occurs. Bony tumors, hereditary diseases, metabolic disorders, neuromuscular disease, and infections can cause focal or generalized bone weakness, making it more prone to fracture. Urgent orthopedic consultation should be obtained for all pathologic fractures with other specialists consulted based on the suspected underlying disease process (Table 119.3).
TABLE 119.3
DIFFERENTIAL DIAGNOSIS OF PATHOLOGIC FRACTURES
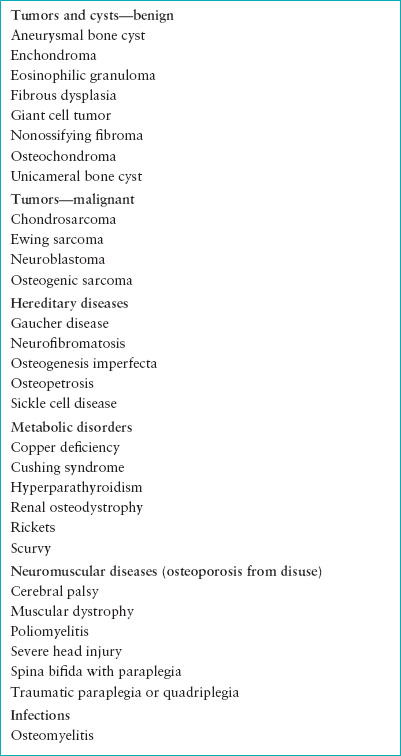

FIGURE 119.7 Radiograph of the pelvis and femur of an 18-month-old girl with osteogenesis imperfecta. There is a healing fracture of the right femur (large arrow), as well as an acute fracture of the left femur (small arrow).
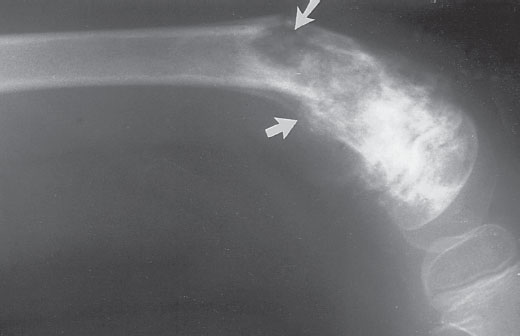
FIGURE 119.8 Radiograph of a 5-year-old girl with an osteosarcoma of the left femur showing an acute pathologic fracture (arrows). Amputation was ultimately necessary.
INJURIES OF THE UPPER EXTREMITIES
Injuries of the Shoulder and Humerus
Clavicle Fractures and Acromioclavicular Joint Injuries
Goals of Treatment. Fractures of the clavicle can be divided into three categories: fractures of the shaft, the medial end, and the lateral or distal portion. Injuries to the lateral aspect of the clavicle must be distinguished from acromioclavicular (AC) joint injuries. Recognition of the type of injury and location of the fracture dictates whether the fracture requires any advanced imaging, orthopedic consultation, and operative repair. The majority of fractures of the clavicle heal without complication and with full recovery of strength and range of motion. Injuries to the medial and lateral aspects of the clavicle include dislocations and physeal injuries; true medial dislocations are rare, but are important to recognize given the potential for vascular injury.
CLINICAL PEARLS AND PITFALLS
• Clavicle fractures in children less than 2 years (excluding the newborn period), particularly of the lateral end of the clavicle are uncommon, and should raise concern for possible nonaccidental trauma.
• The newborn or preverbal child who cries upon being picked up under the arms should be evaluated for possible clavicular fracture.
• Patients with sternoclavicular fractures and dislocations following blunt-force trauma to the chest, may present with referred pain to the shoulder and neck. A careful examination is critical, as posteriorly displaced sternoclavicular fractures may cause damage to the underlying neurovascular and airway structures.
• Complications in the healing of shaft fractures, such as nonunion, malunion, and refracture, can result in chronic pain, deceased range of motion, weakness, or cosmetic deformity.
Current Evidence. The clavicle is the most frequently fractured bone in children, and management considerations vary by the location of fracture (medial, shaft, or distal), age of patient, and degree of displacement. Clavicle fractures may occur in newborns as a result of birth trauma, and in ambulatory children and adolescents secondary to a fall onto the shoulder or an outstretched hand, or from a direct blow to the clavicle. Indications for operative management of clavicle fractures are evolving. While skeletally immature patients have a high rate of fracture healing and good remodeling, recent evidence in the adult literature suggests there may be superior outcomes in patients treated operatively for completely displaced midshaft fractures. Skeletally mature adolescents, with their higher activity level and functional expectations, may also potentially benefit from an interventional approach, thus challenging the traditional nonoperative approach that has been the standard in this age group.
Clinical Considerations
Clinical recognition. Children may present with shoulder pain and cradling of the injured arm, however not uncommonly, these fractures can go unnoticed until a large callus forms and then it gradually remodels over the next 6 to 12 months. The most common fracture type in younger patients is a greenstick fracture of the midshaft, attributable to the thick periosteum of this part of the bone, which is protective against significant angulation and displacement. Older children and adolescents are at higher risk for complete displacement, which is suggested on physical examination by a lowering of the affected shoulder, local swelling, and point tenderness. Medial injuries to the sternoclavicular joint, suggested by localized pain and swelling or a palpable anterior or posterior displacement, are typically physeal injuries secondary to the strong ligaments that anchor the clavicle to the sternum and the relative weakness of the physis. The lateral aspect of the clavicle is anchored by the coracoclavicular and AC ligaments, and thus, fracture through the physis is more common than dislocation (Fig. 119.9). Lateral physeal separation presents clinically as pain with all movements of the shoulder. Typically, the proximal fracture fragment is displaced superiorly, and the radiographic appearance suggests AC separation. However, the periosteum remains whole inferiorly with its ligamentous connections intact. With severe displacement, the skin may be tented over the AC joint. Special note should be made of the “floating shoulder,” an unstable fracture resulting from a glenoid neck fracture combined with an ipsilateral clavicle fracture, such that there is no stable bony connection between the upper extremity and the trunk.
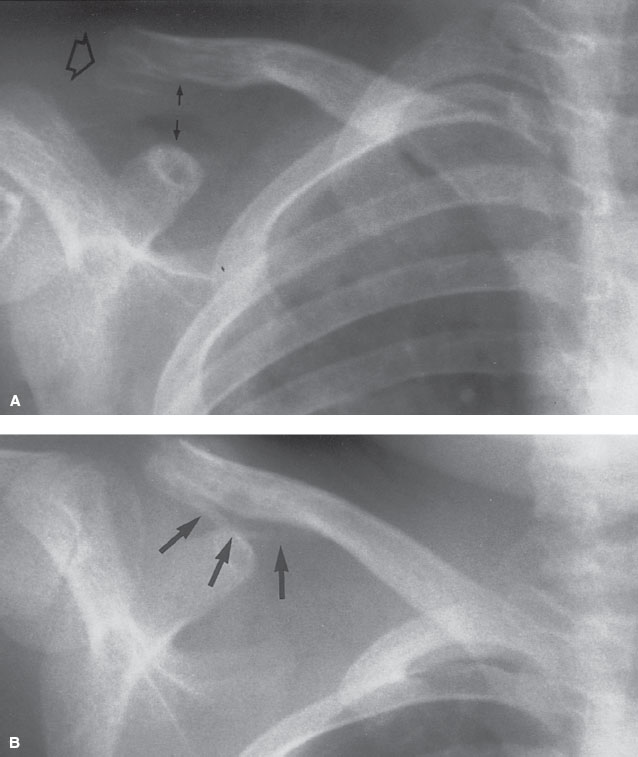
FIGURE 119.9 Radiograph of the right clavicle of a 5-year-old child. A: A lateral clavicular fracture (open arrow) and widening of the space between the clavicle and the coracoid process (small arrows) are evident on the initial film. B: The pattern of new bone formation (arrows) seen on the follow-up radiograph demonstrates that the periosteum and the ligaments have remained intact inferiorly.
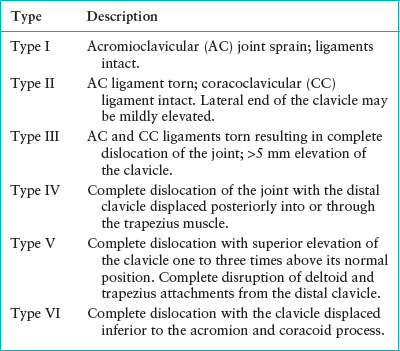
In skeletally mature patients presenting with lateral clavicular pain, particularly young adults suffering blunt trauma such as contact sports, the emergency clinician should also consider AC joint injuries rather than physeal injuries. These injuries, classified by the Rockwood modified classification system range from low-grade (Rockwood I and II) AC joint sprains to high grade (Rockwood III, IV, V, and VI) from progressive increases in force, which result in AC ligament rupture, and then sprain and rupture of the coracoclavicular ligaments (Table 119.4).
Triage considerations. Infrequent, but serious, complications of clavicle fractures include brachial plexus injury, pneumothorax, vascular injury, and tracheal compression. Consequently, any patient with evidence of respiratory distress or neurovascular compromise requires immediate treatment and consultation. More commonly, symptom control for a suspected clavicle fracture with a sling and pain medication is the primary recommendation. With severe AC joint injuries or a forceful mechanism, examination for related cervical spine injuries or secondary neurovascular compromise should be assessed upon presentation.
Clinical assessment. In the setting of a suspected clavicle fracture, the physical examination should include both the shoulder and the arm to evaluate for possible vascular or brachial plexus injury. Visual inspection and palpation of the clavicle for deformity or crepitus should indicate the location of the fracture. Examination for an AC injury should include visual inspection for localized bruising and swelling as well as palpation of the joint during flexion and extension of the shoulder and distraction of the arm as it is placed in adduction. If the injury is not severe and/or the diagnosis is uncertain, the Bell–van Riet test for isolated AC joint pathology is felt to be the most sensitive. For this test, the affected arm is passively raised in full adduction to 90 degrees and crossed in front of the patient toward the contralateral shoulder while maintaining full extension. The patient then attempts to elevate the arm against resistance. If this maneuver results in focal pain at the AC joint and inability to maintain the arm in the adducted and elevated position, this likely indicates an unstable AC joint.
TABLE 119.4
ROCKWOOD CLASSIFICATION OF ACROMIOCLAVICULAR JOINT INJURIES
Management. Plain radiographs with dedicated clavicle views are diagnostic in the majority of clavicular injuries (Fig. 119.9). However, radiographic visualization of medial displacement can be difficult, as this is the last physis of the body to close, and is rarely visible radiographically before age 18. Therefore, special views (e.g., the cephalic tilt view) or advanced imaging with CT may be necessary for the identification of posteriorly displaced sternoclavicular fractures (Fig. 119.10). Radiologic examination in these cases aims to identify any orthopedic injury as well as potentially lethal complications of trauma to the mediastinal structures that lie posteriorly, including the aorta and trachea. Initial imaging for suspected AC joint injury should allow for comparison of the joints either through a single anteroposterior view, which includes both AC joints, or separate radiographs of each AC joint to allow for comparison. Sensitivity for detecting injuries is increased if the x-ray is taken with the arm in internal rotation; however, stress views are no longer recommended.
Most clavicle shaft fractures in children are nondisplaced, minimally shortened or angulated, and are well treated with nonoperative management due to the ability of pediatric bones to remodel. Treatment of shaft fractures typically involves immobilization in either a sling and swathe or a simple sling for 3 weeks followed by 3 weeks of restriction from sporting activities, or until pain resolves. The figure-of-eight splint, an alternative method of immobilization, can be more uncomfortable and cumbersome than the simple sling, and without demonstrated benefit in outcomes. For newborns and toddlers, the child can be put into a long-sleeved shirt with the distal sleeve of the injured side pinned to the shoulder area of the shirt of the contralateral side.
Indications for consultation with an orthopedic surgeon for operative fixation include open fractures, impending open fractures secondary to skin tenting, and neurovascular compromise. Relative indications for operative fixation and/or orthopedic referral include fractures in multitrauma patients, floating shoulder injuries, comminuted fractures, displacement ≥2 cm in the midshaft, and shortening ≥1.5 cm. Nondisplaced fractures of the lateral end of the clavicle are generally treated with conservative measures with analgesia and sling immobilization with good outcomes. Displaced lateral clavicle fractures are often treated operatively, due to the high rates of nonunion. Posterior sternoclavicular fracture displacement is rare in the pediatric population, representing <5% of all sternoclavicular dislocations. Surgical treatment is necessary if closed reduction fails or if there is concern for potential compromise to underlying mediastinal structures.
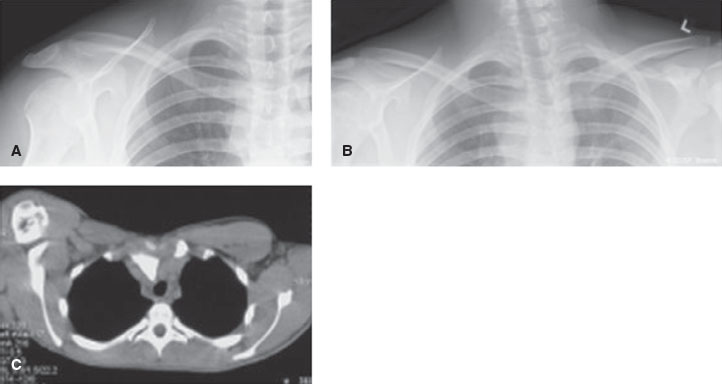
FIGURE 119.10 Three images of a patient with sternoclavicular dislocation. A: Apparent normal anteroposterior (AP) view of the clavicle. B: Serendipity view demonstrating asymmetry of the right sternoclavicular joint indicative of a posterior dislocation. C: CT scan showing posterior sternoclavicular dislocation on the right. (From Waters PM, Bae D, eds. Pediatric hand and upper limb surgery: a practical guide. Philadelphia, PA: Lippincott Williams & Wilkins, 2012, with permission.)
Management of AC joint injuries varies by severity. Typically, types I to III are nonoperative and patients are treated with rest, ice, analgesics, and support or immobilization with a sling; however operative repair of type III separations may be indicated to improve functional outcomes in children and adolescents. Types IV to VI are severe and require orthopedic evaluation and surgical treatment; emergent evaluation is required in the setting of neurovascular compromise.
Disposition. The majority of children with clavicle fractures or injuries to the AC joint can be discharged home. Fractures or injuries requiring operative intervention, including open fractures, those with substantial skin tenting, severe AC joint dislocation or any neurovascular compromise should be seen by orthopedics for possible admission.
Shoulder Dislocation
Goals of Treatment
Traumatic dislocations of the shoulder usually result from an indirect force, which overcomes the supports provided by the muscles and ligaments. This is an extremely painful injury so the initial goal of treatment is to manage the pain and expedite reduction of the shoulder dislocation after radiographs have been obtained. Postreduction radiographs should be obtained to evaluate for possible fractures after reduction.
CLINICAL PEARLS AND PITFALLS
• Complications of shoulder dislocation include fracture of the humeral head (Hill–Sachs lesion), tearing of the anteroinferior glenoid labrum with or without associated bony injury (Bankart lesion), and neurovascular injuries (Fig. 119.11).
• Due to its close association with the glenohumeral joint, the axillary nerve may be injured with shoulder dislocation, resulting in motor and sensory defects, with an estimated incidence from 19% to 55%.
Current Evidence
Anterior shoulder dislocation is the most common joint dislocation seen in the pediatric ED, and accounts for greater than 90% of shoulder dislocations. Shoulder dislocation is rare in infants, but becomes increasingly common through adolescence following physeal closure. In the skeletally immature child, fracture of the proximal humerus is more common than dislocation due to the anatomy of the physis, which largely runs external to the shoulder capsule. Shoulder dislocations are associated with a 70% to 90% recurrence rate.
Intravenous sedation and analgesia has been the mainstay of pain control for shoulder reduction; however, adult literature supports the use of intra-articular injection of lidocaine as an adjunct or possible alternative method of pain control. Although no studies in strictly pediatric populations exist, consideration of intra-articular lidocaine may be worthwhile in skeletally mature adolescents for its added benefits of shorter procedure time and potentially reduced cost.
Clinical Considerations
Clinical Recognition. The patient with a shoulder dislocation usually presents with substantial pain, holding their injured arm supported by the uninjured arm. There is often an obvious abnormality with loss of the usual rounded contour of the shoulder with the dislocation.
Triage Considerations. The patient should be given adequate pain medication, and the injured upper extremity should be placed in a sling. This injury warrants an expedited triage somore definitive management with shoulder reduction can proceed in a timely fashion.
Clinical Assessment. Findings on physical examination of an anterior dislocation include a palpable defect just inferior to the acromion, with loss of the usual rounded contour of the shoulder. On palpation, there is displacement of the humeral head most commonly anterior to the glenoid fossa, and the arm is held in abduction with external rotation. Posterior dislocations are rare, and may present with the arm held in adduction with slight internal rotation, a flattened appearance anteriorly, and prominent coracoid process. Inferior dislocations are the rarest form of shoulder dislocation, and the patient will often present with the arm maximally abducted and adjacent to the head. The complete examination should include assessment of distal neurovascular status, as injury to the axillary nerve may occur with anterior dislocations.
Management. In order to define the direction of displacement, an additional axillary (Y) view, should be obtained along with standard views (anteroposterior and axillary) of the shoulder. Treatment of anterior dislocation through closed reduction can be accomplished by numerous techniques (see Chapter 141 Procedures section on Closed Reduction of Dislocations). Pain management is fundamental for a successful reduction. A wide range of approaches have demonstrated efficacy from procedural sedation to analgesia with mild sedation to local intra-articular lidocaine injections. The neurovascular examination should be repeated postreduction. In addition, repeat radiographs are recommended after reduction to confirm anatomic placement as well as to look for any traumatic fractures such as Hill–Sachs deformities, Bankart lesions, and greater tuberosity fractures (Fig. 119.11). The Hill–Sachs deformity is a cortical depression in the humeral head caused by the glenoid rim at the time of dislocation. This deformity may destabilize the joint and result in recurrent dislocation. A Bankart lesion is an avulsion of a bony fragment during anterior dislocation when the glenoid labrum is disrupted; this lesion is felt to be the primary lesion in recurrent anterior instability.
Patients should be placed in a sling and swathe to stabilize the joint at discharge, with resumption of full activity typically within 2 to 3 weeks. Given the high rates of chronic shoulder instability and recurrent dislocation, orthopedic outpatient follow-up is recommended within 1 week after discharge. Furthermore, given the infrequency of posterior and inferior dislocations, urgent orthopedic consultation in the ED is recommended for these injuries prior to reduction.
Disposition. Once the shoulder has been reduced, the patient may be discharged provided there is no neurovascular compromise. Indications for surgery include irreducible dislocations, displaced greater tuberosity fractures, and large bony glenoid lesions. Since traumatic shoulder dislocations in adolescents have a high rate of persistent instability, orthopedic follow-up is recommended for monitoring of instability and appropriate physical rehabilitation.
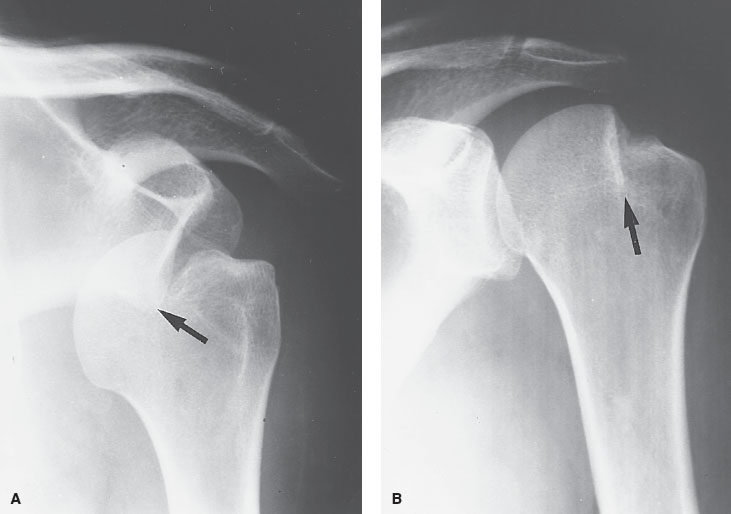
FIGURE 119.11 Hill–Sachs deformity with anterior humeral dislocation. A: AP shoulder demonstrating an anteroinferior dislocation of the humerus with impaction between the inferior glenoid rim and the opposing humeral head (arrow). The impaction produces the articular defect that has been referred to as the hatchet deformity (Hill–Sachs defect). B: Postreduction, AP shoulder. After repositioning the humeral head within the glenoid fossa, the residual effect of compression of the articular surface is clearly identified (arrow). (From Yochum TR, Rowe LJ, eds. Yochum and Rowe’s essentials of skeletal radiology. 3rd ed. Philadelphia, PA: Liwppincott Williams & Wilkins, 2004.)
Injuries of the Scapula
CLINICAL PEARLS AND PITFALLS
• Scapula fractures are uncommon and generally associated with a high-energy mechanism of injury, and as such, are associated with other thoracic or potentially life-threatening injuries.
Scapula fractures are typically seen after injuries of significant force, such as a fall from a height, a motor vehicle collision or other severe direct blow (Fig. 119.12). The emergency clinician should assess for other possible associated injuries including clavicle fractures, rib fractures, pneumothorax, thoracic vertebral fractures, and fractures of the humerus. Fractures of the body and neck of the scapula are generally well visualized on plain radiographs; however, adequate definition of glenoid injuries may require a CT scan. Fracture management is often conservative, with a sling and swathe, or a shoulder immobilizer for patient comfort, graduating to gentle range-of-motion exercise after 2 weeks. Orthopedic consultation is recommended given the infrequency of this injury and its association with other injuries. Complications are not common except for possible malunion or functional impairment arising from associated thoracic injuries.
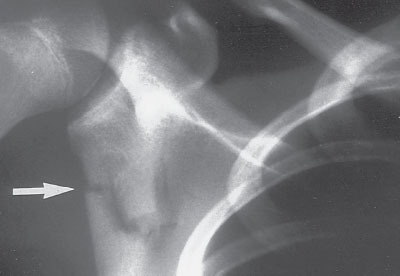
FIGURE 119.12 Radiograph of a 13-year-old boy who sustained an isolated right scapular fracture as the result of a skateboarding accident (arrow).
Injuries of the Humerus
CLINICAL PEARLS AND PITFALLS
• Humeral fractures are associated with high-energy direct blows; any fracture with minimal trauma should raise suspicion for pathologic fracture or abuse.
• Children in early adolescence are particularly high risk for proximal humerus physeal injuries due to the rapid growth and relative weakness of this portion of the bone.
• Humerus fractures may result in radial nerve injury, which may be identified by numbness of the dorsum of the hand between the first and second metacarpals and decreased motor strength with wrist and thumb extension and forearm supination.
• Orthopedic consultation is indicated for any humeral shaft fractures with rotational deformity or angulation greater than 15 to 20 degrees.
Proximal Humerus Fractures
Injuries to the proximal humerus or humeral physis occur commonly after a fall on outstretched hand (FOOSH) (Fig. 119.13). Caution should be exercised in the evaluation of the infant patient, as these fractures may also be sustained in the setting of birth trauma and physical abuse. On examination, the child may hold the arm in abduction and extension, with focal tenderness to palpation, localized swelling, and occasionally shortening of the affected extremity. Routine radiographs are generally sufficient for diagnosis, and comparison views may be helpful in distinguishing a fracture from the normal physeal line. The vast majority of injuries to the proximal physis are Salter–Harris types I and II. In the young infant, plain radiographs may prove inadequate to evaluate the humeral head as it is primarily cartilaginous, and therefore the distinction between a fracture and a dislocation cannot easily be determined. Ultrasonography or MRI may be necessary to make this diagnosis.
Proximal humerus fractures in skeletally immature children and adolescents are traditionally treated nonoperatively and have a tremendous capacity for remodeling. As much as 50 degrees of angulation in the proximal humerus may heal without fracture reduction in the ED. Nonunion and malunion are rare, except in adolescents with significantly displaced or angulated fractures. Adolescents with significantly displaced fractures (greater than 20 to 50 degrees) may be candidates for operative fixation, although data on whether this improves outcomes are limited. Management is typically with a sling, sling and swathe, splint, or hanging cast for several weeks. Orthopedic follow-up after discharge is recommended.

FIGURE 119.13 Impacted proximal right humeral fracture with approximately 25 degrees of angulation in a 3-year-old child. Full remodeling can be anticipated.
Humeral Shaft Fractures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







