MUSCULOSKELETAL EMERGENCIES
MARK D. JOFFE, MD AND JOHN M. LOISELLE, MD
GOALS OF EMERGENCY CARE
Nonfracture related orthopedic emergencies often pose a diagnostic dilemma for even the most experienced clinician due to indolent courses and lack of distinguishing signs and symptoms. The pediatric emergency clinician is challenged to make the diagnosis and institute early therapy as outcomes often correlate with the time to institution of treatment after symptoms begin. The time to antibiotic administration and time to surgery are key goals for these disorders. A systematic approach utilizing appropriate laboratory testing, imaging, and orthopedic consultation will most often detect these conditions. Certain conditions such as septic arthritis of the hip must be diagnosed at the time of the initial visit so that surgical intervention combined with timely antibiotic therapy can minimize the likelihood of poor outcomes such as growth retardation or irreparable joint dysfunction. When unrecognized or untreated, other orthopedic conditions may lead to prolonged pain, chronic functional disorders, or a delay in the ability to return to normal activity.
KEY POINTS
 A normal plain radiograph does not rule out significant disease or pathology.
A normal plain radiograph does not rule out significant disease or pathology.
 Referred pain or the inability of the young child to localize pain can obscure the diagnosis.
Referred pain or the inability of the young child to localize pain can obscure the diagnosis.
 Trauma is too often assumed to be the cause of symptoms when skeletal infection is present.
Trauma is too often assumed to be the cause of symptoms when skeletal infection is present.
 Presence of fever and significant elevations in inflammatory markers are useful when considering infectious etiologies.
Presence of fever and significant elevations in inflammatory markers are useful when considering infectious etiologies.
 Provocative physical exam testing is helpful in distinguishing certain overuse injuries.
Provocative physical exam testing is helpful in distinguishing certain overuse injuries.
 Cultures should be obtained from the blood and potentially infected areas when there is concern for musculoskeletal infection.
Cultures should be obtained from the blood and potentially infected areas when there is concern for musculoskeletal infection.
RELATED CHAPTERS
Signs and Symptoms
• Injury: Shoulder: Chapter 38
Clinical Pathways
• Fever in Children: Chapter 88
Medical, Surgical, and Trauma Emergencies
• Infectious Disease Emergencies: Chapter 102
OSTEOMYELITIS
CLINICAL PEARLS AND PITFALLS
• Refusal to move a limb or pseudoparalysis may be a sign of osteomyelitis
• Up to 40% of children with osteomyelitis will be afebrile
• Radiographs are helpful in evaluating for alternate diagnoses but do not rule out osteomyelitis when obtained early in the course of the illness
• Osteomyelitis is frequently associated with septic arthritis in neonates
• Pathogens or etiology of musculoskeletal infection vary by age of the patient
• Staphylococcus aureus is the most common organism in all ages
• Magnetic resonance imaging (MRI) is the imaging study of choice
• Patients with sickle cell disease are at risk for Salmonella osteomyelitis
• Inflammatory markers are elevated in up to 90% of cases of osteomyelitis
• CRP is the most effective inflammatory marker in monitoring the response to therapy
• The lower extremity accounts for up to 70% of cases of osteomyelitis in children
Current Evidence
Osteomyelitis is an inflammation of the bone and bone marrow that is most commonly of infectious origin. Infection is confirmed by the presence of two of the following: pus on an aspirate of the bone, clinical findings consistent with the diagnosis, positive blood or bone aspirate cultures, and consistent findings on medical imaging. Osteomyelitis is more common in boys, with the highest incidence found among infants and preschool age children. Younger age and underlying disorders are associated with an increased risk for contracting osteomyelitis, as well as for the particular pathogens involved.
Bacteria gain entrance to the bone through one of three routes: hematogenous, direct spread from adjacent infection, or inoculation through a penetrating wound. Hematogenous spread is the most common route of infection in children. A transient bacteremia is believed to be the initiating event in the infection. Bacteria enter the bone at the level of the metaphysis where the predominant vascular supply is located. The sluggish blood flow within the microvasculature of the marrow predisposes to infection. Local trauma has been suggested as a possible cause of microthrombotic events further predisposing bone to infection. This is supported by an association of trauma with the occurrence of osteomyelitis and the preponderance of infections occurring within the long bones, especially those of the lower extremities. In sickle cell patients, microinfarcts within the more tenuously supplied area of the diaphysis may explain the increased occurrence in this region of the bone. As infection progresses, pressure increases and organisms penetrate up through the cortex to the subperiosteal space.
Differences in the underlying bony structure in the neonate and young infant predispose them to a higher incidence of multifocal osteomyelitis and concomitant septic arthritis. The thin cortex allows easier penetration to the subperiosteal space. The periosteum is less adherent in these ages and less effective in limiting the spread of infection. Transphyseal vessels, which are present through the first 18 months of life, allow bacteria to gain access to the adjoining epiphysis and joint space.
A less common source of osteomyelitis in children is penetration of the periosteum by adjacent infections such as a cellulitis or abscess. Inoculation of the bone from stepping on a nail, surgical instrumentation, or intraosseous line placement provides a third means for infection to gain entrance to the bone.
Goals of Treatment
Early recognition and treatment of osteomyelitis prevents the spread of infection and minimizes the risk of poor outcomes such as growth disturbance, abscess formation, sepsis, chronic osteomyelitis, or even death. The time to initiation of antibiotic administration from onset of symptoms or arrival to medical care is a key objective of care. Empiric antibiotic treatment is based on the patient’s age, Gram stain of an aspirate if performed, the likely means of contracting the infection, and underlying comorbidity. The ultimate choice of antibiotic and the length of treatment are dictated by the offending organism which is identified through appropriate cultures. Although acute operative intervention is rarely necessary, timely consultation of orthopedic surgery facilitates bone aspiration when indicated and the initiation of treatment.
Clinical Considerations
Clinical Recognition
The infant or child with osteomyelitis typically presents with fever, localized musculoskeletal pain, or pain with movement. Trauma is not an obvious explanation for the symptoms. The absence of fever does not rule out the presence of osteomyelitis.
Triage Considerations
The patient with limp or localized musculoskeletal symptoms is often triaged as urgent. Those with a question of neurovascular compromise, severe pain, or who appear systemically ill should be evaluated more immediately. These patients should have their degree of pain documented and should receive analgesics on arrival.
Initial Assessment/H&P
Physical signs of osteomyelitis are age dependent and recognition requires patience and diligence on the part of the clinician. The older child is more likely to have localized infection and is more capable of expressing or identifying a site of localized pain and point tenderness. The neonate or young infant may present with a pseudoparalysis of the affected limb. Another common, although nonspecific, finding in this age group is paradoxical irritability in which the infant exhibits pain or distress upon handling and is more comfortable when left alone.
Fever and pain are highly sensitive findings but are not universally present. Fever is described in up to 90% of children with osteomyelitis upon presentation and may be quite elevated. Signs of pain may include limp, refusal to bear weight, or a decreased range of motion when a limb is involved. Erythema and swelling are less frequent but can also be observed at the site, and usually suggest more advanced periosteal involvement.
Osteomyelitis typically follows an indolent course and is less likely to present with the acute onset of symptoms that is more typical of traumatic injuries. A history of minor trauma is common and often coincidental in an active child. A history of sickle cell disease, prior surgery or skeletal manipulation places the patient at higher risk for osteomyelitis.
Management/Diagnostic Testing
In addition to clinical findings, the diagnosis of osteomyelitis depends on culture results. A blood culture and bone aspirate should be obtained in suspected cases of osteomyelitis before the initiation of antibiotics. Isolation of the causative organism is important not only for diagnosis, but also in antibiotic selection and determining the length of therapy. Reports of positive blood cultures in the setting of osteomyelitis range from 30% to 57%. An organism is recovered from a bone aspirate in 51% to 90% of cases. The combination will identify a pathogen in 75% to 80% of cases. Bone aspirates may remain positive for several days after antibiotic use, whereas blood cultures are often sterile within 24 hours of the initiation of antibiotics.
Laboratory tests vary in sensitivity. The white blood cell (WBC) count rises in only one-third of the cases of osteomyelitis, whereas both the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are elevated in more than 90% of the cases. The latter tests are useful in diagnosis and in monitoring the response to therapy. The CRP peaks at 2 days and gradually returns to normal over 7 to 10 days of appropriate therapy. The ESR may remain elevated for several weeks despite adequate treatment. In the setting of a low clinical suspicion for osteomyelitis, a normal CRP, ESR, and plain radiograph suggests an alternative diagnosis.
The plain radiograph is useful both in detecting early signs of osteomyelitis and excluding other diagnostic possibilities. The earliest radiographic changes suggestive of osteomyelitis include deep soft-tissue swelling with elevation of the muscle planes from the adjacent bone. These may be seen as early as 3 to 4 days after the onset of symptoms. Lytic bone changes are not detectable until 10 to 14 days. Periosteal elevation, when present, is not generally visible until 10 to 21 days after infection (Fig. 129.1). A negative radiograph in the first 10 days of illness does not rule out osteomyelitis. When suspicion remains high in the setting of a negative radiograph, further imaging studies should be obtained. The triple-phase technetium bone scan has a reported sensitivity and specificity of more than 90%, and is the test of choice when osteomyelitis is suspected but a specific site of concern cannot be identified by physical examination or when multiple foci of infection are possible. MRI is also highly sensitive in detecting osteomyelitis and does not expose the child to ionizing radiation. In addition, MRI provides a higher degree of detail than the bone scan (Fig. 129.2). This is useful in detecting suspected complications of osteomyelitis such as a subperiosteal abscess or bone sequestrum. Many orthopedic surgeons prefer this high degree of resolution to guide a bone aspirate or biopsy. Both imaging studies commonly require sedation of the young child, but the bone scan is not as affected by small movements. A bone aspirate preceding a bone scan or MRI does not alter the results and should not be delayed because of this concern.

FIGURE 129.1 Periosteal activity in distal fibula in child with Staphylococcus aureus osteomyelitis; day 20 of illness.
Organisms responsible for osteomyelitis vary according to age of the patient, the route of infection, and any underlying comorbid conditions. S. aureus is the most common pathogen across all age groups accounting for 70% to 90% of cases. The incidence of community-acquired methicillin-resistant S. aureus (CA-MRSA) has increased dramatically in most areas of the United States. Some studies have found over 70% of cases due to MRSA. Osteomyelitis due to MRSA has been associated with a longer duration of fever, extended hospitalization, and increased frequency of complications. Group A β-hemolytic streptococcus and Streptococcus pneumoniae are the next most common organisms isolated in childhood osteomyelitis and together account for 10% of cases outside of the neonatal period. The frequency of Kingella kingae has been increasing and is most commonly reported in the toddler and preschool age group. It is difficult to culture and the increased incidence may be due to improved success in identification through polymerase chain reaction (PCR) and improved culture techniques. It is a gram-negative organism and therefore resistant to vancomycin and clindamycin, but sensitive to cephalosporins and β-lactam antibiotics. Bacterial isolates from neonates younger than 2 months include S. aureus, group B streptococcus, and Escherichia coli (Table 129.1).
Certain groups are at risk for particular organisms. Patients with sickle cell disease have a high incidence of osteomyelitis caused by salmonella. Pseudomonas aeruginosa is a common organism found in osteomyelitis of the foot, often resulting from a nail penetrating a sneaker.
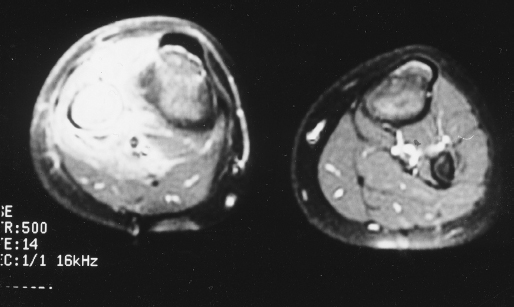
FIGURE 129.2 Magnetic resonance imaging of osteomyelitis of the proximal right fibula.
TABLE 129.1
INITIAL ANTIBIOTIC THERAPY: OSTEOMYELITISa
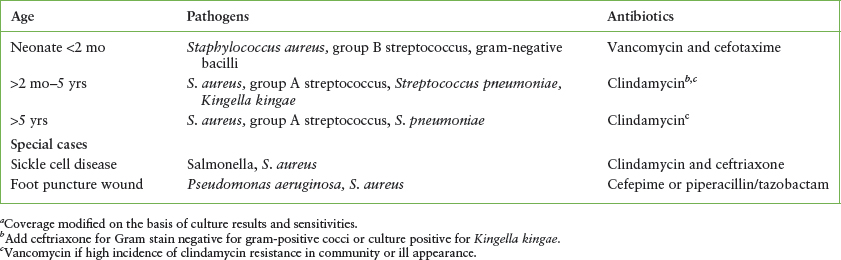
Clinical Indications for Discharge or Admission
Initial therapy for osteomyelitis includes hospital admission with intravenous antibiotics and pain control. Empiric antibiotic therapy is based on the predominant organisms in each age group, local sensitivity patterns, the mechanism of infection, and Gram stain results. Clindamycin is the treatment of choice for osteomyelitis outside of the neonatal age range when MRSA is suspected. Vancomycin may be indicated for empiric treatment when the incidence of clindamycin resistance in the community is high or the patient is critically ill. Definitive treatment is ultimately based on the identification and sensitivity of recovered isolates. A third-generation cephalosporin or the addition of an aminoglycoside is indicated in the neonatal age group. Suggested agents are listed in Table 129.1. Early aggressive antibiotic therapy frequently prevents the need for surgical intervention. The duration of hospitalization is determined by the organism involved, the clinical response to treatment, and decreasing CRP levels.
SEPTIC ARTHRITIS
Goals of Treatment
The presence of bacterial pathogens within the articular capsule presents a true surgical emergency. Delay in the identification and treatment of an infected joint in a child can result in severe and permanent sequelae. Early initiation of treatment can preserve normal function of the joint and prevent destruction or ischemic changes due to excessive pressure buildup from the infection. Improved outcomes are associated with reduced time to initiation of antibiotic therapy and time to surgery for the septic hip. The urgency associated with this diagnosis has given rise to the maxim, “The sun should never rise or set on a septic hip.” The evaluation focuses on distinguishing septic arthritis from more benign causes of joint pain that do not require invasive forms of identification and treatment.
CLINICAL PEARLS AND PITFALLS
• Resistance or pain with movement of the joint is the principal clinical finding
• A septic hip is held in abduction and external rotation
• Inflammatory markers can be helpful in distinguishing inflammatory from infectious etiologies
• Ultrasound cannot distinguish an inflammatory effusion from an infectious one, but the lack of a joint effusion can rule out septic arthritis
• Fever is more common with septic arthritis than transient synovitis
• Lyme disease most commonly manifests as monoarticular arthritis of the knee and most children are still able to ambulate
• Arthrocentesis is the definitive means of identifying septic arthritis
Current Evidence
Bacteria gain entry to the joint space through one of three means. The highly vascular synovium is most commonly infected through hematogenous seeding. The role of local injury in predisposing joints to infection by this means is unclear. Organisms from adjacent areas of infection may invade the joint, or direct inoculation can occur through penetrating injuries. Infection secondary to penetrating objects may be delayed from the actual time of injury so that external wounds may be small or healed at the time of presentation. Adjacent osteomyelitis is present in up to 10% of cases.
Eighty to 90% of septic joints occur in the lower extremities. The knee and hip are most commonly affected. The same distribution is found in the preambulatory child. Infections involve only a single joint in greater than 90% of cases. Multifocal infections are more common in neonates and infections with Neisseria species.
Pressure elevation within the minimally distensible joint capsule can compromise vascular flow, resulting in ischemic injury to the bone and cartilage. This is a particular concern in the hip, where avascular necrosis of the femoral head is a well-described complication of septic arthritis. Prognosis is worse in children younger than 1 year, with involvement of the hip joint, with delay to the initiation of therapy, and with infection by S. aureus.
Clinical Considerations
Clinical Recognition
Septic arthritis occurs in all ages. Pain is the most common presenting complaint in the child with a septic joint. Because of the predominance of septic arthritis in the lower extremities, the younger child often presents with a limp, abnormal gait, or inability to bear weight. Referred pain from the hip may manifest as groin, thigh, or knee pain. Swelling or redness of a joint is often a late finding but can be the primary reason for the patient to seek medical care. The neonate or young infant with a septic joint may display fever, asymmetric movement, or lack of movement of a limb. Recent traumatic events do not adequately explain these findings. Patients with a prior history of a rheumatologic condition or invasive procedures involving the joint are more likely to have an alternate cause for their joint pain.
Triage
Patients with complaints of joint pain and/or fever, limited range of motion of a joint, joint swelling or limp are typically categorized as urgent. The patient with severe pain, neurovascular compromise or ill appearance should be evaluated more emergently. Patients should have a temperature and pain severity documented and receive analgesics. With concern of septic arthritis, the child should be made NPO.
Initial Assessment/H&P
The history should focus on the location of joint pain, its duration, and relation to movement. Pain due to septic arthritis is typically constant or increasing over time. The clinician should inquire about local injuries that may identify a traumatic cause for the symptoms or penetrating injuries that may predispose to joint infection. A prior history of rheumatoid disorders, sickle cell disease, or joint surgery should be obtained. Sexually active teenagers are at risk for gonococcal arthritis. The presence of rash may suggest juvenile idiopathic arthritis or a viral etiology for the joint pain.
Range of motion around the affected joint is dramatically reduced. Any degree of movement causes great distress and is vigorously resisted. Many clinicians rely on this aspect of the evaluation more than any other in differentiating infection from alternative causes of joint pain.
Clinical signs are more subtle in the neonate or young infant with a septic joint. Nonspecific findings such as septic appearance, irritability, and pseudoparalysis of a limb are common presenting findings in these ages. Parents may note excessive irritability associated with diaper changes in the infant with a septic hip. The child with a septic hip will typically hold the lower extremity in abduction and external rotation in order to decrease intracapsular pressure (Fig. 129.3). Close observation, and isolated manipulation of each joint will help identify the particular area of involvement.
The skin surface should be closely evaluated for local signs of injury. Most involved joints will have obvious erythema, warmth, and swelling. The exception is the hip joint because of its deep-seated location. Swelling may be less obvious in the pudgy infant. Fever is a commonly associated sign but is absent in up to one-third of patients.

FIGURE 129.3 Five-month-old infant with septic arthritis of the right hip. Hip joint is held in flexion, abduction, and external rotation.
Management/Diagnostic Testing
The diagnosis of septic arthritis is confirmed by the identification of purulent fluid within the joint space. Arthrocentesis is a mandatory procedure in all suspected causes of septic arthritis. The decision to perform this procedure is based on the degree of clinical suspicion in combination with results of laboratory tests and imaging studies; none of these in isolation are 100% sensitive in detecting or excluding septic arthritis from other conditions. A sample of synovial fluid is often the only means of discriminating septic arthritis from less serious inflammatory processes.
The mean peripheral WBC count is generally elevated in children with septic arthritis, however, more than half of the patients will have a WBC count less than 15,000 per mm3. The ESR and CRP are more sensitive markers and are elevated in 90% to 95% of patients. In areas endemic for Lyme disease, serum for Lyme titers (IgM and IgG; two-tiered testing) should be obtained.
Plain radiographs may demonstrate signs of an effusion ranging from subtle blurring or displacement of fascial planes to complete dislocation of the joint. The main role of the radiograph in the evaluation is to exclude fractures or other bony abnormalities that may mimic septic arthritis. Ultrasound is most useful in evaluating the hip. It is much more sensitive than the radiograph in detecting a joint effusion. Some have suggested that the absence of an effusion on an ultrasound scan effectively excludes the diagnosis of septic arthritis. The ultrasound cannot, however, distinguish between infected and sterile inflammatory effusions. Ultrasound guidance is useful in performance of a needle aspiration of the hip joint.
The isolation of a bacterial pathogen provides a definitive diagnosis and directs subsequent management. Cultures of joint fluid and blood should therefore be performed on all patients with a possible septic joint. The yield of organisms can be increased by directly inoculating joint fluid into a blood culture bottle. When indicated, cultures from additional sites should be obtained to increase the potential isolation of a pathogen. Cultures of the joint fluid demonstrate the highest yield and are positive in 50% to 80% of cases. Blood cultures identify an organism in 15% to 46% of patients with septic arthritis and are positive in many cases in which the organism is not isolated from the joint fluid. Cervical or urethral cultures or urine PCR testing in sexually active adolescents with septic arthritis may identify Neisseria gonorrhoeae as the responsible organism. In 20% of cases, a causative organism is not recovered. Improved application of PCR techniques may increase the ability to identify pathogens in the future.
TABLE 129.2
INITIAL ANTIBIOTIC THERAPY: SEPTIC ARTHRITISa
A Gram stain should be performed on joint fluid, and it occasionally provides additional assistance in identifying both the presence of an infection and the infecting organism. Although elevation of the WBC count more than 100,000 per mm3 in the synovial fluid is considered strong evidence of infection, the actual counts are often much lower. Presence of purulent fluid, a positive Gram stain, and a highly elevated WBC count with a left shift in the synovial fluid are often used as indications for operative intervention when there is a concern of a septic hip. (See eBook link to Septic Arthritis Pathway.)
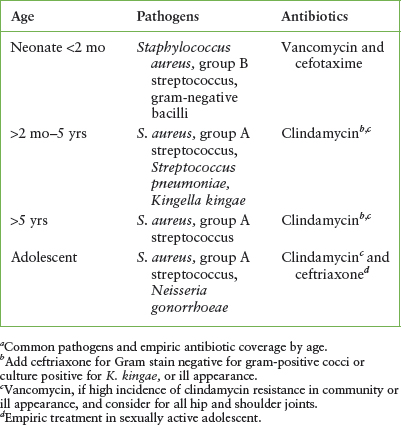
With few exceptions, bacteria found in septic arthritis are the same as those in osteomyelitis (Table 129.2). S. aureus is the most common reported isolate in all age groups. Prior to the introduction of the Hib vaccine, Haemophilus influenzae type b was the leading cause of septic arthritis in the 6-month-old to 5-year-old age group. Through immunization, this organism has now been essentially eliminated and surpassed in frequency by group A streptococcus and S. pneumoniae. S. aureus is also the predominant pathogen in neonatal patients. Gram-negative coliforms and Group B β-hemolytic streptococcus are also found in this age group. N. gonorrhoeae is found in neonates and is a frequent pathogen in sexually active teenagers. K. kingae is a fastidious gram-negative rod, susceptible to beta lactam antimicrobials, which has recently been isolated as a pathogen in numerous childhood bone and joint infections. It is found most commonly in children younger than 36 months. Neisseria meningitidis is a rare but reported cause of septic arthritis in children.
Clinical Indications for Discharge or Admission
The management of septic arthritis consists of hospitalization, parenteral administration of antibiotics (Table 129.2), and joint immobilization. Joint irrigation should be performed in selected cases. Empiric antibiotic therapy is dictated by the common organisms in the age group, local sensitivities, and by results of the synovial fluid Gram stain. Vancomycin or clindamycin is indicated depending on the incidence of clindamycin-resistant MRSA in the community; vancomycin should also be considered as part of the antimicrobial regimen for critically ill children. Gram-negative coverage should be added in neonates and adolescents. A third-generation cephalosporin should be added in patients with sickle cell disease because of susceptibility to salmonella infection.
Surgical intervention for joint irrigation is generally indicated for all cases involving the hip joint; infections in which large amounts of fibrin, debris, or loculations are found within the joint space; or when the patient fails to improve following several days of intravenous antibiotic therapy. Expeditious and aggressive management limits but does not eliminate potential sequelae of septic arthritis.
Lyme Arthritis
Lyme disease is a common cause of infectious arthritis in certain geographic locations within the United States. The infection is caused by the spirochete Borrelia burgdorferi which is transmitted through the bite of certain infected tick species. Arthritis is a manifestation of late disease and can occur 1 to 12 months following inoculation. Lyme arthritis is most often a monoarticular infection of the knee. If left untreated, symptoms can be episodic, lasting several days followed by several weeks to months without symptoms. Clinical and laboratory findings are similar to those for septic arthritis. Joint swelling is marked and out of proportion to the degree of pain. Fever is often absent and is generally low grade when present. Pain and limitation of movement of the affected joint is less than in septic arthritis, and patients are often able to ambulate despite the swelling. Infection can occur without a preceding known history of a tick bite or the classic skin manifestations of erythema migrans. Facial palsy or meningitis are more typical of early disseminated disease and therefore are rarely concurrent with arthritis. The ESR and CRP are elevated. When arthrocentesis is performed, the mean leukocyte count in synovial fluid is usually 10,000 to 25,000 cells per mm3 but can exceed 50,000 cells per mm3 with a neutrophil predominance. Routine cultures of synovial fluid are negative. In the appropriate clinical setting physical and laboratory findings may be sufficient to identify patients at low risk for septic arthritis and potentially avoid the need for arthrocentesis. Two-tiered diagnostic testing for Lyme arthritis is indicated in endemic areas. The first tier should include a serum enzyme-linked immunosorbent assay or immunofluorescence assay. Positive results should be confirmed by a Western immunoblot for IgG antibodies to B. burgdorferi. An IgM immunoblot assay is not necessary in late disease and may result in false-positive results. Negative serum IgG serology excludes Lyme as the cause of arthritis. Treatment for Lyme arthritis consists of a 4-week course of oral antibiotics. Doxycycline in a dose of 4 mg per kg per day divided twice daily with a maximum of 100 mg per dose is effective for children older than 8 years, whereas amoxicillin (50 mg per kg per day in three divided doses with a maximum of 1.5 g per day) is sufficient in younger children. Cefuroxime (30 mg/kg/day in two divided doses with a maximum of 1,000 mg daily) is an alternative for patients with penicillin allergy. Serum antibody titers remain elevated even after adequate antibiotic treatment and should not be used as a measure of success of treatment. Persistent or recurrent joint swelling may occur 2 months beyond the initiation of treatment. Although this may represent a local autoimmune response, experts recommend retreatment with a second 4-week course of oral antibiotics or a 2- to 4-week course of parenteral ceftriaxone.

FIGURE 129.4 Seven-year-old child with transient synovitis of the left hip. Hip joint is held in same position of comfort as in septic arthritis.
Transient Synovitis
Transient or toxic synovitis is a benign, self-limiting inflammatory condition of the hip. It afflicts males more frequently than females and is the most common cause of acute hip pain in children 3 to 10 years of age. The underlying cause is unknown, although a postinfectious inflammatory response has been suggested. Its presentation can mimic that of septic arthritis of the hip (Fig. 129.4), a distinction that is as crucial in management as it is difficult in diagnosis.
The onset of symptoms is abrupt with unilateral hip pain and limp. Fever is rare, occurring in less than 10% of cases, and when present, is usually low grade. Although patients complain of discomfort with movement of the limb, it is generally possible to gently maneuver the hip through a near full range of motion. This contrasts with the septic hip in which pain and spasm are more extreme, and patients resist a full range of motion. Additional signs of systemic illness are absent and, despite the label, the child is nontoxic appearing.
Laboratory tests are generally useful only in attempting to distinguish transient synovitis from more serious conditions. The WBC count, ESR, and CRP are generally normal or only slightly elevated. The mean WBC count, ESR, and CRP are significantly lower than in septic arthritis; however, sufficient overlap exists between values in transient synovitis and septic arthritis such that they do not reliably distinguish between the two conditions in individual patients. The Kocher criteria consist of a combination of clinical and laboratory variables which are commonly used as a clinical prediction tool to assist in distinguishing septic arthritis from transient synovitis. The four factors include a history of fever, nonweight bearing, ESR greater than 40 mm/hr, and WBC count greater than 12,000 cells/mm3.
Radiographs may demonstrate an effusion but principally serve to exclude pathologic osseous conditions. Ultrasound is more sensitive than plain films at detecting joint effusions, although accuracy declines in patients younger than 1 year of age. Reports of an effusion of the hip by ultrasound in transient synovitis vary from 50% to 95%. The clinician must use a combination of clinical, laboratory, and radiographic findings to determine which patients require further evaluation with needle aspiration of the hip. Although patients often report relief of pain following aspiration, the procedure is unnecessary except to exclude the presence of a bacterial infection. Synovial fluid, when obtained, is sterile. The synovial fluid WBC count is typically less than 50,000 cells per mm3.
Treatment occurs on an outpatient basis, and emphasizes rest and analgesics. Traction is of unproven benefit and is potentially harmful. Nonsteroidal anti-inflammatory medications are the first-line therapy for pain. Pain duration is typically 3 to 4 days but may last as long as 2 weeks. Exacerbations can occur if activity is resumed too early.
There is no evidence of serious sequelae resulting from transient synovitis. The relationship between transient synovitis and the subsequent development of Legg–Calvé–Perthes disease (LCPD) is unclear. Studies have been unable to demonstrate cause and effect. Some suggest that these patients are at increased risk for developing LCPD, whereas others believe only that the clinical presentations are similar. Recurrences of transient synovitis can occur up to several years later and are not associated with worse outcomes.
Penetrating Intraarticular Wounds
Penetrating intraarticular wounds are not specific to children, but they are injuries that the pediatric emergency physician must recognize and treat on an urgent basis in order to prevent serious and potentially permanent sequelae. Knees are the most commonly injured joints. Motor vehicle accidents and direct trauma from falls are the cause in the overwhelming number of cases. A penetrating joint injury commonly missed in the emergency department is the closed fist injury in which the patient strikes an opponent in the mouth. A tooth can disrupt the capsule of the metacarpophalangeal joint and introduce oral bacteria. Failure to recognize this injury can result in septic arthritis, osteomyelitis, and permanent joint damage.
An open joint may be detectable on direct visualization or by palpation through a periarticular laceration. Injuries that extend below the skin surface adjacent to a joint effusion should raise a high level of suspicion that the joint space has been violated. The presence of air in the joint on radiograph is diagnostic for joint penetration (Fig. 129.5). In less obvious cases, disruption of the joint capsule can be demonstrated by the saline load test. Arthrocentesis is performed through an uninjured site on the skin surface, and saline is injected. Extravasation of saline from the joint into the wound is diagnostic for penetrating injury. A volume of 60 mL of saline is generally adequate to evaluate knee joint integrity, 20 mL for elbow or ankle joints, and 1 to 2 mL for finger joints. The addition of a small amount (<0.1 mL) of methylene blue to the saline has historically been used to improve visualization of extravasated fluid, though it may not have clear benefit over saline alone. Clinical evaluation has poor sensitivity in identifying penetrating wounds compared with saline injection. Other studies have shown that the saline load test may also miss a significant number of joint disruptions. If a question still remains regarding the integrity of the joint after such testing, then further imaging studies or surgical exploration is necessary.

FIGURE 129.5 Intraarticular air in knee joint following penetrating injury sustained from fall on edge of stone.
Open wounds of the joint are considered contaminated and broad-spectrum antibiotics should be administered. Surgical intervention consists of vigorous irrigation and debridement, often in the operating room. Attention should be given to appropriate tetanus prophylaxis, splinting, wound dressing, and pain control while the patient remains in the emergency department.
The prognosis of penetrating intraarticular wounds is dependent on the degree of overlying soft-tissue injury and the extent of intraarticular damage. Infectious complications are the most common. Septic arthritis with a variety of both gram-positive and gram-negative organisms is an early and common outcome of inadequate early intervention. Delayed synovitis, often necessitating synovectomy, has been described after unidentified penetration of small foreign bodies.
OVERUSE SYNDROMES
Goals of Treatment
The treatment of overuse injuries strives to return the athlete rapidly and safely to full participation. Early diagnosis and initiation of appropriate therapy for overuse injuries will prevent recurrent or chronic injury as well as permanent damage to the growing musculoskeletal system.
CLINICAL PEARLS AND PITFALLS
• Initial therapy for overuse injuries includes rest, ice, and nonsteroidal anti-inflammatory medication.
• A change in biomechanics, exercise regimen, equipment, or strength and flexibility is necessary to avoid recurrence of overuse syndromes.
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







