GENERAL PRINCIPLES
The anatomy of the pediatric musculoskeletal system is unique and reflects the active growth and development that occurs during childhood. Fracture classification, treatment approach, and types of complications are directly related to this unique anatomy. In general, both injury patterns and treatment approaches in children in whom closure of the physes (growth plates) has already occurred is similar to those of the adult. Therefore, the major focus of this chapter is directed at injuries occurring in the prepubescent child with open physes. In addition, diseases specific to children that cause nontraumatic musculoskeletal complaints are covered.
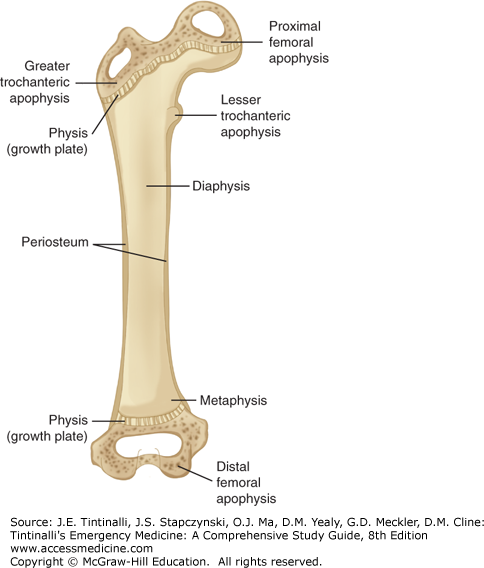
The long bones of children consist of discrete anatomic areas. The physis is an area of growth cartilage and may occur at one (e.g., the phalanges) or both (e.g., the tibia and the femur) ends of a long bone. The area of bone between a physis and the adjacent joint is termed the epiphysis. An apophysis is an outgrowth of bone, usually with its own ossification center in childhood that often serves as a point for muscle or ligament attachment. The midshaft of a long bone is referred to as the diaphysis. The metaphysis of a long bone represents the area between the diaphysis and the physis (Figure 140-1; see chapter 267, “Initial Evaluation and Management of Orthopedic Injuries”).
FIGURE 140-1.
The anatomy of the pediatric long bone as demonstrated by the femur. Longitudinal growth occurs at the physes (growth plates) located at either end. Bony prominences that serve as sites of muscular or ligamentous attachment are known as apophyses (e.g., greater trochanteric apophysis).
The long bones of children are less dense and more porous than the long bones of adults. Pediatric long bones respond to mechanical stress by bowing and buckling rather than fracturing through and through, as in adults. The periosteum of the diaphysis and the metaphysis is thick in children and is continuous from the metaphysis to the epiphysis, surrounding and protecting the mechanically weaker physis. The weakness of the physis is in part related to the reduced oxygen tension found in the hypertrophic zone of the physis. This hypertrophic zone is the location of frequent fractures within the physis. The physis is also sensitive to alterations in the blood supply, and physeal injuries can result in growth disturbance. Compression forces alone may also affect bone growth. This is particularly true when compression forces are applied to the epiphyseal side of the physis. The injury to bone growth caused by compression results from interruption of the epiphyseal circulation to the reproductive cells of the physis.
The growth of the musculoskeletal system and its response to injury are influenced by the growth of muscle and connective tissue. The ligaments of children are stronger and more compliant than in adults, and ligaments tolerate mechanical forces better than the weaker physes. Therefore, apophyseal detachments or epiphyseal fractures are much more common than ligamentous injuries during childhood.
FRACTURE PATTERNS
The Salter and Harris classification system (see Figure 267-7) is based on the relationship of the fracture line to the physis and the prognosis for growth disturbance.
Salter-Harris Type I Fractures Type I physeal injuries occur when the epiphysis separates from the metaphysis. The cleavage is through the hypertrophic cell zone of the physis, with the reproductive cells of the physis remaining with the epiphysis. There are no associated fragments of bone, as the thick periosteal attachments surrounding the physis remain intact. The epiphysis may, however, displace from the metaphysis. Type I injuries have a low incidence of growth disturbances.
Suspect a Salter-Harris type I injury when there is point tenderness over a physis. Radiographic findings are typically subtle or absent, and soft tissue swelling or a joint effusion may be the only abnormality. Epiphyseal displacement can usually be appreciated on x-rays in one or more views (Figure 140-2); however, in the absence of epiphyseal displacement, the diagnosis is a clinical one.
Treatment of most type I fractures consists of immobilization of the suspected fracture using an appropriate splint, cold compresses, and elevation to limit swelling. Refer to an orthopedic surgeon for monitoring of bone growth disturbances. Type I fractures of the distal fibula (which happens to be the most common fracture site for type I) are exceptions because they are not associated with growth arrest and can be followed by a primary care physician after splinting.
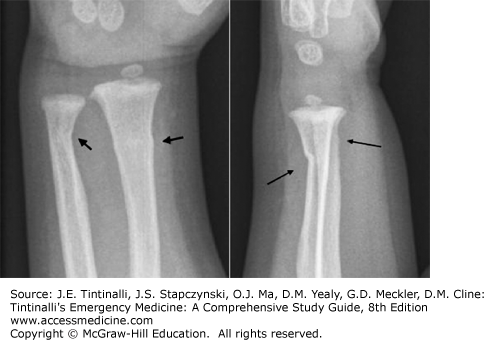
Salter-Harris Type II Fractures In a type II injury, the fracture line extends a variable distance along the hypertrophic cell zone of the physis and then out through a piece of metaphyseal bone. The periosteum overlying the metaphyseal fragment remains intact, whereas the periosteum on the opposite side of the fracture is torn away from the diaphysis while remaining adherent to the epiphysis. Growth is preserved because the reproductive layers of the physis maintain their position with the epiphysis and the epiphyseal circulation. Diagnosis is made radiographically by noting a triangular-shaped fragment of metaphysis that is not associated with discernible injury to the epiphysis (Figures 140-3 and 140-4).
Treatment of a type II fracture consists of closed reduction of any displacement followed by immobilization in a splint or cast, ice, elevation, analgesia, and orthopedic follow-up.
Salter-Harris Type III Fractures Type III physeal injuries are intra-articular. The fracture line extends intra-articularly from the epiphysis, through the hypertrophic zone of the physis, with the cleavage plane continuing along the physis to the periphery. The prognosis for subsequent bone growth relates to the preservation of circulation to the epiphyseal bone fragment; however, the prognosis is usually quite favorable.
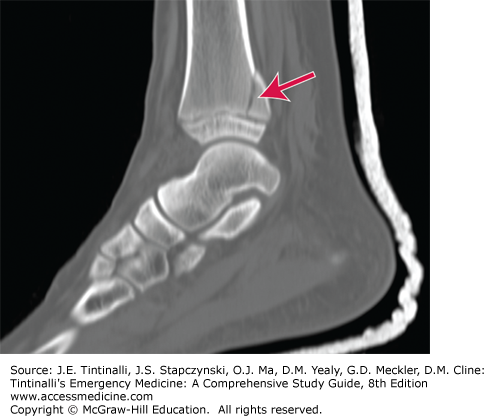
The diagnosis of a type III injury is made radiographically and is based on the appearance of an epiphyseal fragment not associated with an apparent metaphyseal fracture. There may or may not be an associated periosteal injury (Figure 140-5). Occasionally, additional imaging with CT or MRI is used to better evaluate the extent of fracture and articular surface involvement. Treatment requires orthopedic consultation and follow-up, as open reduction may be required in some cases to ensure proper alignment of the articular surface.
FIGURE 140-5.
An x-ray of a Salter-Harris type III fracture of the distal tibia, also known as Tillaux’s fracture. Note the intra-articular component extending through the growth plate and the medial epiphysis of the tibia. [Reproduced with permission from Strange GR, Ahrens WR, Schafermeyer RW, Wiebe RA: Pediatric Emergency Medicine, 3rd ed. McGraw-Hill, Inc., 2009. Fig 38-8.]
Salter-Harris Type IV Fractures In type IV injuries, the fracture line originates at the articular surface and extends through the epiphysis, the entire thickness of the physis, and continues through the metaphysis (Figure 140-6). The risk of growth disturbance with this type of fracture is significant, and reduction must be precise.
The diagnosis of a type IV injury is made radiographically upon identification of epiphyseal and metaphyseal fragments. Treatment is typically open surgical reduction and internal fixation.
Salter-Harris Type V Fractures Type V injuries typically involve the knee or ankle and are the result of a profound compressive force transmitted to the physis, resulting in crushing of the chondrocytes in both the reserve and proliferative zones. Displacement of the epiphysis is usually only minimal despite the significant damage to the physis.
The diagnosis of a type V injury may be difficult initially, leading to a lack of appreciation of the severity of the injury. An initial diagnosis of a sprain or a type I physeal fracture may prove incorrect in view of subsequent development of premature growth arrest during follow-up. Radiographs may appear normal or may demonstrate focal narrowing of the physeal plate. There is also typically a joint effusion. The history, however, should point to a type V injury, as these injuries are typically associated with a significant mechanism. Treatment consists of casting and orthopedic monitoring in anticipation of bone growth arrest.
Compressive forces often result in a bulging or buckling of the periosteum rather than a more complete fracture line. Cortical, or torus, fractures are so named to describe prominence or bulging of the bony cortex, usually involving the metaphysis. These are also called buckle fractures.
A simple torus fracture will not produce a visible deformity to the shape of the extremity; however, there is typically soft tissue swelling and point tenderness over the bony injury. In children who are not obese, the torus fracture is occasionally palpable as a ridge over the metaphyseal area of the long bone.
Radiographically, the torus fracture may be subtle. Carefully inspect the contour of the metaphyseal flare. Any asymmetry, bulging, or deviation of the cortical margin indicates a torus fracture. Soft tissue swelling is also usually evident (Figure 140-7). Torus fractures are not associated with angulation, displacement, or rotational abnormalities, so reduction is not necessary. Treat by splinting in a position of function with primary care or orthopedic follow-up within 1 week. Simple torus fractures of the distal radius can need splinting, but orthopedic follow-up is not necessary.
A greenstick fracture is characterized by cortical disruption and periosteal tearing on the convex side of the bone, with an intact periosteum on the concave side of the fracture. Greenstick fractures are more stable and somewhat less painful than complete fractures because the area of intact periosteum limits bony displacement (Figure 140-8).
The need for reduction is determined by the degree of angulation of the fracture, the age of the child, and the anatomic location of the injury.
Plastic deformities, also referred to as bowing or bending fractures, are almost exclusively limited to the forearm and lower leg long bones. Usually, a bowing injury is noted in combination with a complete fracture of the other bone of the forearm or lower leg. The cortex of the diaphysis of the long bone is deformed, but the periosteum along the entire diaphysis is preserved.
Plastic deformity is usually obvious clinically, which should guide the inexperienced clinician who may think that in the absence of an obvious fracture the x-ray appearances are normal.
Proper interpretation of the radiographs requires an awareness of the normal shape of the long bones involved because fracture lines and disruptions in the periosteum are absent. Comparison films of the uninvolved extremity are not typically necessary. Prompt orthopedic consultation is required for any plastic deformities, as proper reduction and realignment are essential. Reduction usually requires completion of the fracture and restoration of proper alignment.
See chapter 148, “Child Abuse and Neglect” for a complete discussion of child abuse.
UPPER EXTREMITY INJURIES
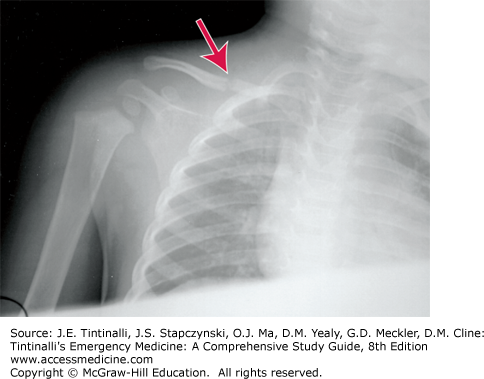
Clavicle fractures occur during two distinct time frames: the newborn period and childhood. Fractures of the clavicle in the newborn usually result from birth injury (Figure 140-9). Risk factors include high birth weight and shoulder dystocia. The infant may demonstrate upper extremity palsy secondary to a brachial plexus injury or may have “pseudoparalysis” of the extremity secondary to pain. Although many clavicle fractures are detected at birth, the diagnosis may be delayed, especially if the fracture is nondisplaced. An ED visit may be made when the newborn is not moving one arm during the first week of life, or when a parent notices a small “lump” or callus at the clavicle during the first 2 to 3 weeks of life. Clavicle fractures in the newborn do not need specific treatment. Pain control and careful handling of the baby are usually all that are required.
Clavicle fractures outside of the newborn period usually result from accidental injury in a mobile child. However, clavicle fractures in the nonambulatory child should raise the possibility of abuse. The most common mechanism of injury is either a fall onto an outstretched hand or onto the lateral side of the shoulder. The clavicle may fracture in three general sites: the diaphysis, medial end, or lateral end.
Fractures of the diaphysis usually occur in the middle third of the clavicle and are the most common of all clavicle fractures. Treatment is an arm sling/shoulder immobilizer or collar and cuff, as tolerated by the child. Even displaced and overlapping fractures tend to heal well with simple immobilization for 3 to 4 weeks. Complete healing and remodeling can take >1 year, and a small callus will become palpable in most cases if the fracture was displaced. Routine follow-up with the primary care physician is typically sufficient.
Fractures at the medial end of the clavicle are uncommon. Given the strong ligamentous attachment of the clavicle to the sternum, injuries to this area are usually epiphyseal disruptions. Orthopedic consultation is recommended for displaced fractures of the medial clavicle.
Fractures of the distal end of the clavicle are also uncommon in children and again more likely to be epiphyseal disruptions. Minimally displaced distal clavicle fractures only need immobilization with a sling or equivalent. Surgical reduction may be needed for more displaced fractures.
Fractures of the humerus are divided into three groups: fractures of the proximal humerus, fractures of the humeral diaphysis, and fractures of the condyles and supracondylar area. Supracondylar and condylar fractures are discussed as part of “The Pediatric Elbow” section below.
Fractures of the proximal humerus may occur at the physis or the proximal humeral metaphysis, and they have an extraordinary ability to repair themselves. Proximal humeral physeal fractures occur more commonly in adolescence because this area becomes relatively weak during this time due to rapid growth. Fractures of the proximal humeral metaphysis are more common in preadolescents. Treatment depends on the age of the child and degree of displacement and/or angulation. Orthopedic consultation is needed to determine the best approach. In general, the younger child can tolerate a greater degree of displacement. For slightly displaced fractures, treatment is conservative, with immobilization in a sling and orthopedic follow-up. Significantly displaced fractures of the proximal humerus in young teens (e.g., off-ended Salter-Harris type II fracture) may need fixation; however, most angulated fractures otherwise will remodel. Brachial plexus injuries can rarely occur when the distal fragment is displaced into the axilla.1
Fractures of the humeral diaphysis are uncommon in children. Direct trauma can cause a transverse fracture, and violent rotation can cause a spiral fracture. The fracture fragment may injure the radial nerve as it runs in the radial groove. Potential for healing is good, and treatment is usually immobilization in a long arm plaster splint and orthopedic follow-up. Closed reduction (or even open reduction and internal fixation) by orthopedics may be required for displaced fractures in the teenager. Transverse fractures tend to be more unstable than spiral fractures. Assess radial nerve function on initial examination and following any splinting (wrist extensors and supinators, sensation of dorsoradial hand, thumb, and second digits). Consider abuse in small children with fractures of the diaphysis of the humerus because of the significant force required to produce fractures in this area.
Compared with other fractures, elbow fractures in children are commonly missed in the ED. The radiologic diagnosis of elbow fractures is challenging because of the large cartilaginous component of the elbow.
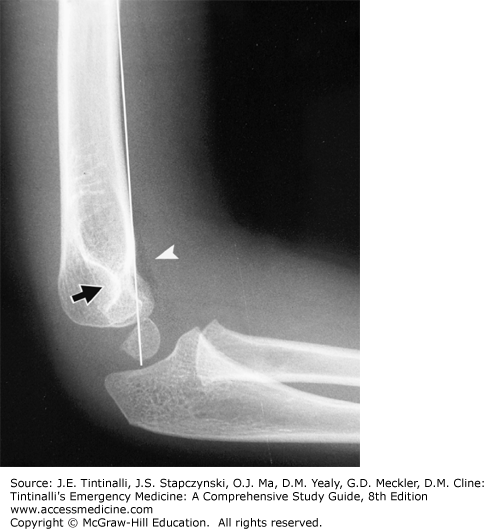
True lateral and anteroposterior radiographs of the elbow are essential to diagnose fractures (Figure 140-10).
FIGURE 140-10.
Anterior humeral line. A line drawn along the anterior cortex of the humeral shaft normally intersects the middle third of the capitellum. A normal radiographic teardrop is seen where the cortices of the olecranon and coronoid fossae come together (black arrow). A small normal anterior fat pad is visible (arrowhead). [Reproduced with permission from Schwartz D: Emergency Radiology Case Studies, © 2008, McGraw-Hill, New York.]
If the capitellum falls posterior to the anterior humeral line, an extension-type supracondylar fracture is a possible diagnosis. Other diagnoses to consider include lateral condyle fractures or, rarely, a transphyseal fracture. Additionally, the radius should point to the capitellum in all radiographic views (the radiocapitellar line) (Figure 140-11). If not, consider lateral condyle fracture, radial neck fracture, Monteggia’s fracture, or elbow dislocation.2,3
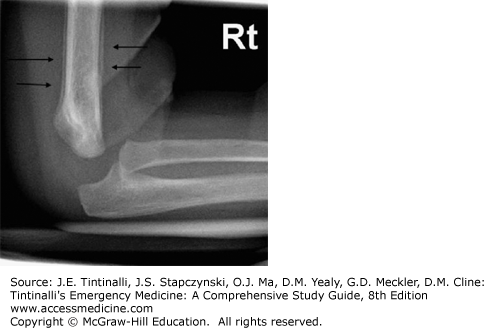
Lateral radiographs are also used to evaluate for subtle effusions when an occult fracture is suspected. An anterior fat pad may be normal and appears as a small drop of oil hugging the distal anterior humerus. An anterior fat pad that seems to protrude like a sail from the distal humerus may be pathologic (“sail sign”). A posterior fat pad is always pathologic and is evidence of a hemarthrosis from intra-articular injury.
Oblique views or CT scan can be obtained if there is clinical suspicion of fracture without clear radiographic findings on standard anteroposterior and lateral views.
It is important to identify the ossification centers around the elbow to avoid confusion with fracture. There are six ossification centers appearing at varying ages in the pediatric elbow. The mnemonic used over the years is CRITOE (capitellum, radial head, internal [medial] epicondyle, trochlea, olecranon, external [lateral] epicondyle). All of the ossification centers may be seen on the anteroposterior view of the elbow in the appropriately aged child, although the olecranon may be difficult to identify. On the lateral view, all are seen but the trochlea and external (lateral) epicondyle (CRIO).
Supracondylar fractures are the most common fractures in children <8 years old. The majority of supracondylar fractures occur in children from 3 to 10 years of age, with the peak incidence occurring between ages 5 and 7 years old. The extension type is by far the most common, accounting for 90% to 98% of cases. An extension-type supracondylar fracture is caused by a fall on an outstretched hand with the elbow hyperextended. A flexion-type fracture results from falling on a flexed elbow and is rare. The complications of a supracondylar fracture, although uncommon, range from transient neurapraxia to Volkmann’s ischemic contracture, with the most common being injury to the anterior interosseous nerve resulting in the “pointing finger sign.”
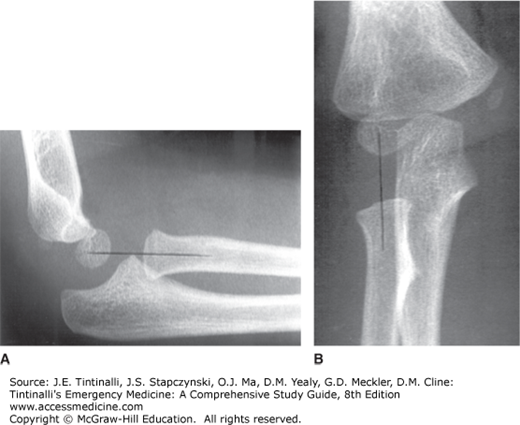
Classification of Supracondylar Fractures Classification of supracondylar fractures is based on the extent of fracture fragment displacement. Type I fractures have no displacement or angulation and may have an anterior or posterior fat pad sign as the only radiographic finding (Figure 140-12). Confirmation of a supracondylar fracture will be seen on later x-rays done at 2 to 4 weeks that will demonstrate periosteal reaction of the humerus (Figure 140-13). Type II fractures are angulated to varying degrees, but the posterior cortex of the humerus is intact (Figure 140-14). Type III fractures are completely displaced with no cortical contact (Figure 140-15). The distal fragment may be posteromedially (type IIIa) rotated and, as such, can impinge against the radial nerve or be posterolaterally (type IIIb) rotated. In posterolaterally displaced fractures, the brachial artery and median nerve are at risk for injury, and compartment syndrome can develop.1,4 If compartment syndrome is suspected (see chapter 278, “Compartment Syndrome”), emergency orthopedic consultation is needed. Traction and reduction are indicated if the hand is cool, pale, and pulseless. The simple absence of a pulse in an otherwise viable hand is a contraindication to manipulation in the ED.
FIGURE 140-14.
A. Clinical picture of a type II supracondylar fracture with marked soft tissue swelling in a child with a history of falling on an outstretched arm. B and C. Anteroposterior (AP) and lateral views of the elbow, demonstrating a supracondylar fracture with medial opening seen on the AP view and posterior displacement of the distal fragment identified on the lateral view. [A: Reproduced with permission from Shah BR, Lucchesi M, Amodio J, Silverberg M: Atlas of Pediatric Emergency Medicine, 2nd ed. © 2013, McGraw-Hill, New York. Fig. 19-33A. B and C: Image used with permission of Karen Black, BC Children’s Hospital, Vancouver.]
Treatment The level of displacement and the prereduction physical examination dictate treatment of pediatric supracondylar fractures. Type I supracondylar fractures are inherently stable. The goal of therapy is comfort and immobilization. Apply a double sugar tong splint or a long-arm posterior splint with the elbow at 90 degrees and the forearm in pronation or neutral rotation for 3 weeks. Arrange orthopedic follow-up within 2 to 7 days. While collar and cuff immobilization is used in some centers, it does not offer as good pain management as splinting.5,6 Type II and III fractures need orthopedic consultation in the ED for definitive management that typically includes operative pinning.7 Keep these patients fasting for anticipation of surgical intervention.
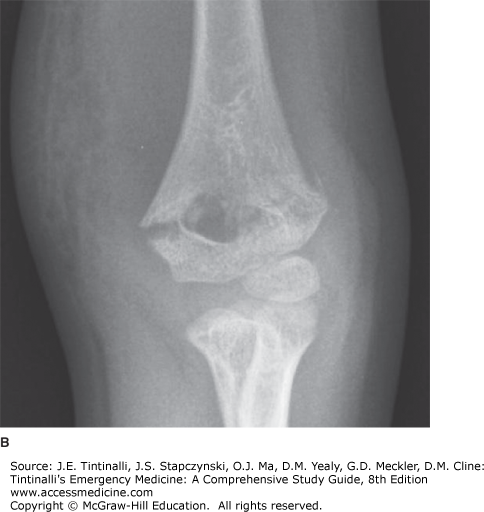
Lateral condyle fractures can be Salter-Harris type II (most common) or IV. The mechanism of injury is varus stress on an extended elbow with the forearm in supination. Swelling and tenderness are usually limited to the lateral elbow, and neurovascular injury is uncommon. Diagnosis can be made with standard anteroposterior and lateral views, but obtain an oblique view if clinical suspicion is high. Treatment is based on amount of displacement and articular congruence, but often requires open reduction and internal fixation as these fractures are transphyseal and intra-articular. Nonunion, malunion, osteonecrosis, cubitus valgus, and tardy ulnar nerve palsy are well-described complications, so orthopedic consultation is needed to determine the best treatment approach. Displacement can occur even within a cast or splint due to the pull of the forearm extensor tendons (Figure 140-16).
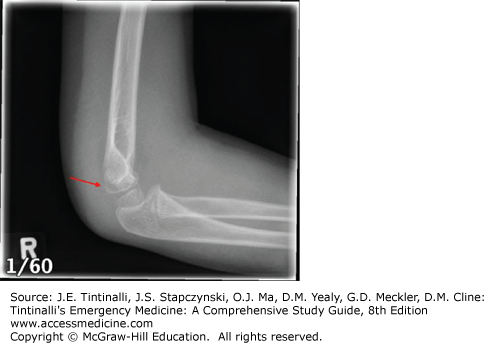
Fractures of the medial epicondyle tend to occur in older children, between the ages of 10 and 14 years old. They are not true Salter-Harris injuries, because the apophysis rather than the physis is involved. Simple fractures of the medial epicondyle are extra-articular injuries with limited soft tissue involvement, but nearly half of injuries are associated with elbow dislocation; in such injuries, the epicondyle can become entrapped in the joint.8,9 Fractures are classified by the amount of displacement and associated extremity injuries, and orthopedic consultation is needed to determine the best approach (Figure 140-17).
Most distal humeral transphyseal fracture injuries occur in children <2.5 years old. Recognition is both difficult and important, especially in infants, in whom this particular injury is often the result of child abuse. This injury is thought to result from a twisting mechanism that shears off the distal epiphysis and is an intentional injury (child abuse) until proven otherwise.
Olecranon fractures generally result from a fall on the elbow. Orthopedic consultation is best to guide treatment. If the fracture is displaced <5 mm, it should be immobilized in the most stable position, usually 45 degrees of elbow flexion, for 3 to 6 weeks. Open reduction and internal fixation are indicated for unstable fractures. Olecranon fractures occur in association with fractures of the radial head and neck. A “simple” olecranon fracture may be part of Monteggia’s lesion, so radial head position should be evaluated carefully.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree