Chapter 23 Minimizing Radiation Exposure
BIOLOGICAL EFFECTS OF IONIZING RADIATION
The use of x-ray, gamma, and positron ionizing radiation for patient diagnosis and treatment can be quite disconcerting to the patient, as well as the perioperative nurse responsible for the care of the patient. It is not uncommon for staff and patients to raise questions regarding the safety of procedures involving ionizing radiation. Radiation health effects have been studied extensively. Evidence of human radiation health effects comes from many sources, but primarily from the studies of the survivors of the atomic bombings in Japan, uranium miners, radium dial painters, and medical studies. The Japanese Life Span Study was designed to evaluate the late mortality effects of the radiation and other trauma received by the survivors of the Hiroshima and Nagasaki A-19 atomic bombs. The sample population consisted of approximately 100,000 persons, including those exposed near to ground zero, persons exposed at such distances from ground zero as to guarantee that little radiation was received, and nonexposed immigrants to the cities (Beebe et al, 1961). The information obtained from these studies indicates a linear increase in adverse health effects from relatively large doses of radiation. There is minimal evidence to support increased risk to people at lower levels of radiation.
Deterministic Health Effects
When a tissue or an organism is exposed to very high doses of radiation (hundreds of rad) in a short period of time, the primary effect is cellular death. This is a deterministic health effect. As a result, the organ or system loses its ability to function or dies. The severity of the effect is directly related to the dose; the greater the dose, the more damage occurs. Deterministic effects exhibit a threshold radiation dose. Doses received below the threshold are not associated with adverse health effects. For example, cataract formation is evident when the lens of the eye receives a dose of approximately 200 to 300 rad (2 to 3 Gy) of gamma radiation. Note that “no radiogenic cataracts resulting from occupational exposure to x-rays have been reported. From patients who suffered irradiation of the eyes in the course of x-ray therapy and developed cataracts as a consequence, the cataractogenic threshold dose is estimated at about 200 rads” (Cember and Johnson, 2009).
Stochastic Health Effects
In a medical facility the possibility of a radiation health care worker receiving a high acute dose of ionizing radiation is extremely unlikely because of the presence of a RSP involving dose monitoring, education, and dose-reduction strategies. The main concern is for those health care workers who receive chronic, low levels of radiation exposure over their working lifetime. There are many dose-response models that describe the relationship between radiation dose and health effects. For doses greater than 50 rem (500 mSv), there is a definite linear relationship between dose and additional cancer risk (NRC, 1996). Fifty rem (500 mSv) is 10 times higher than the current annual limit of 5 rem (50 mSv). Below 50 rem (500 mSv), there is no definitive relationship between dose and additional cancer risk. Because of the uncertainty in the dose-response relationship at doses below 50 rem (500 mSv), it is assumed that there is a linear zero threshold-dose response at the lower levels of radiation dose. This means that all radiation doses are assumed to have some adverse effect. This is a conservative assumption that serves as the basis for our radiation protection programs throughout the world. By incorporating the philosophy of maintaining exposures from levels of ionizing radiation as low as reasonably achievable, additional effort is made to minimize radiation doses to health care workers and members of the public.
Finally, teratogenic effects are developmental effects caused by intrauterine exposure to ionizing radiation. Irradiation of the developing fetus is a concern because of the rapidly dividing and developing cells. The risk to the fetus is a function of gestational age at the time of radiation exposure and the radiation dose. Based on this information, the risk from ionizing radiation to the fetus and children is higher than that for adults. The data to support a teratogenic effect come from experiments using animal models and from human populations exposed to very high doses of radiation such as the atomic bomb survivors. For humans the significant teratogenic effects observed included mental retardation, intrauterine growth retardation, and cancer development such as childhood leukemia. However, not all exposures to ionizing radiation cause these effects. For most diagnostic procedures involving ionizing radiation in which the fetal dose is less than 10 rem (100 mSv), very little data exist to support teratogenic effects in humans (Duke University, 2009; Edwards, n.d.). Even though there is very little evidence of teratogenic health effects below 10 rem (100 mSv), there is enough cause for concern that RSPs have established additional policies for the declared pregnant health care worker and the pregnant patient intended to further reduce the radiation dose to the fetus. The focus of this chapter is on the health care worker, and radiation safety policies for the declared pregnant health care worker will be discussed in greater detail later in this chapter.
RADIATION DOSE LIMITS
Based on the discussion regarding biological effects from exposure to ionizing radiation, it is prudent to explain radiation dose limits and how they are applied to protect individuals. Regulatory agencies have established specific limits of radiation dose for those working with ionizing radiation and for those considered members of the general public. Those individuals working with or around ionizing radiation that have been trained are considered occupational radiation workers. Individuals who work in or near areas where ionizing radiation is used, but are not directly involved in its use, are frequently referred to as ancillary personnel. Administrative staff, housekeeping, and maintenance staff may be considered ancillary personnel. These individuals may receive minimal training on radiation safety awareness. The term general public is applied to those individuals who are not directly working with ionizing radiation and who do not receive radiation safety training. Occupational radiation workers are limited to 5 rem (50 mSv) per year. Ancillary personnel and the general public are limited to 0.1 rem (1 mSv) in a year and less than 0.002 rem (0.02 mSv) in any hour. Annual dose limits in the United States are listed in Table 23-1 (NRC, 2009).
TABLE 23-1 Annual Dose Limits in the United States
| Total whole body dose (occupational) | 5 rem/year (50 mSv/year) |
| Lens of the eye (occupational) | 15 rem/year (150 mSv/year) |
| Skin (occupational) | 50 rem/year (500 mSv/year) |
| Extremities (occupational) | 50 rem/year (500 mSv/year) |
| Members of the general public and ancillary personnel | 0.1 rem/year (1.0 mSv/year) not to exceed 0.002 rem (0.02 mSv) in any hour |
From U.S. Nuclear Regulatory Commission: Occupational dose limits for adults, 10 CFR 20.1201, April 2009; U.S. Nuclear Regulatory Commission: Dose limits for individual members of the public, 10 CFR 20.1301, April 2009.
Declared Pregnancy Policy
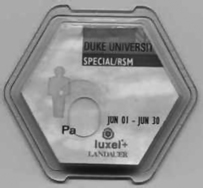
Work restrictions for the declared pregnant health care worker are required if there is a significant potential for the embryo/fetus to receive a dose in excess of the 0.5 rem (5 mSv) limit as a result of the external exposure of its mother and/or from intakes of radioactive material by its mother. The expectation is that the radiation dose would be received at an even rate over the entire gestation period. To accurately assess the fetal dose, it is recommended that the declared pregnant health care worker receive a fetal dosimeter, which should be worn at the abdomen at about waist level (Figure 23-1). If the worker wears an x-ray–shielding apron, the fetal dosimeter must be worn under the apron. The fetal dosimeter should be exchanged monthly for analysis. A facility may elect to purchase maternity lead aprons designed specifically for use by the pregnant health care worker. Most maternity lead aprons increase lead shielding from 0.5 mm to 1.0 mm in areas to protect the fetus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree