Chapter 29 Metabolic Emergencies
The endocrine system is instrumental in regulating metabolism, tissue function, growth, development, moods, and emotions. Additionally, it works to maintain homeostasis in response to physiological stress.1 Dysfunction of one endocrine gland can affect the physiology of the entire body.2 Disruption in the production, supply, or use of hormones or electrolytes can result in a medical emergency that requires prompt assessment, diagnosis, correction, and identification of the precipitating cause. Figure 29-1 shows the location of the major endocrine glands.
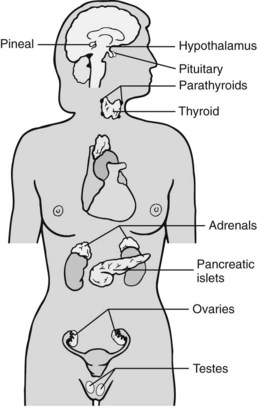
Fig. 29-1 Location of major endocrine glands.
(From Lewis, S. L., Heitkemper, M. M., & Dirksen, S. R. (2007). Medical-surgical nursing: Assessment and management of clinical problems (7th ed.). St. Louis, MO: Mosby.)
Diabetic Emergencies1–4
• Type 1, formerly called insulin-dependent diabetes or juvenile-onset diabetes, results from an absolute insulin deficiency.
• Type 2, previously referred to as non–insulin-dependent diabetes or adult-onset diabetes, is characterized by insulin resistance, increased hepatic glucose release, impaired glucose storage, and eventual insulin deficiency. Type 2 is the more prevalent form and tends to be progressive, eventually requiring a second oral drug or insulin.
Hypoglycemic Emergencies2,3
Etiology
Hypoglycemia is the most common acute complication of diabetes. Normal blood glucose levels range from 80 to 120 mg/dL (4.4 to 6.6 mmol/L). Sources vary, but hypoglycemia is defined as a blood glucose level less than 60 to 70 mg/dL and severe hypoglycemia is defined as a blood glucose level less than 40 mg/dL. How quickly the serum glucose decreases can influence the patient’s symptoms; if glucose levels drop too quickly in relation to the body’s compensatory ability, the patient may become symptomatic at levels of 60 to 80 mg/dL.2
Patients at risk for hypoglycemia may be taking4:
• Sulfonylureas (first generation: tolbutamide; second generation: glipizide, glyburide; third generation: glimepiride)
• Meglitinides including repaglinide (Prandin) and nateglinide (Starlix)
• Intensive insulin therapy regimens due to type 1 diabetes
• Long-acting oral hypoglycemic agents, such as chlorpropamide (Diabenese), due to type 2 diabetes4
Other causes of hypoglycemia include the following:
• Insufficient food intake including inadequate caloric intake or missed meals (most common cause)
• Too much insulin (includes unintentional and intentional overdoses of insulin or oral hypoglycemic agents)
• Sulfonylurea potentiation of insulin action in the liver
• Increased exercise or activity
Oral hypoglycemic agents that do not cause hypoglycemia3,4:
• Biguanides (metformin [Glucophage]): Decreases hepatic production of glucose and increases insulin sensitivity. Risk: Lactic acidosis.
• Thiazolidinediones (rosiglitazone [Avandia], pioglitazone [Actos]): Increases sensitivity to insulin in peripheral tissue. Risk: Hepatotoxicity.
• Alpha-glucosidase inhibitors (acarbose [Precose], miglitol [Glyset]): Decreases gastrointestinal glucose absorption. Risk: Diarrhea.
Presentation
Mild
In mild hypoglycemia, adrenergic symptoms are the predominant findings:
However, these symptoms are masked (“hypoglycemic unawareness”) in patients:
• With long-standing diabetes (because diabetes neuropathy affects the autonomic system)
• Who have had recent severe episodes of hypoglycemia (because of diabetic autonomic neuropathy, there is loss of the typical autonomic response)
• Who are taking beta-blocker medications (these drugs block the typical epinephrine response).
• Who are alcoholics (inhibition of gluconeogenesis by alcohol)
Moderate
Moderate hypoglycemia is characterized by neuroglycopenic symptoms as a result of insufficient glucose to the brain.3,5
Treatment
Treatment of Hypoglycemia in the Conscious Patient
• Measure the serum glucose level. A fingerstick blood glucose test is adequate to begin treatment.
• Obtain a laboratory analysis of serum glucose for confirmation of the meter reading. However, do not delay treatment while awaiting laboratory results if the patient is symptomatic.
• Administer 15 to 20 g of a rapid-acting oral glucose preparation (Table 29-1).
• If the serum glucose level does not improve within 15 minutes, administer a second dose of carbohydrates orally. (Sympathetic nervous system symptoms should resolve quickly but neurogenic symptoms may continue for 1 hour or longer even if blood glucose levels are greater than 100 mg/dL.)
• After an increase in serum glucose, follow with oral complex carbohydrate administration (usually lasting less than 2 hours). A complex carbohydrate snack or meal eaten soon after blood glucose begins to rise will decrease the risk of recurrent hypoglycemia.
TABLE 29-1 TREATMENT OF HYPOGLYCEMIA
| Each of the following contains 15 g of carbohydrates: |
Treatment of Hypoglycemia in the Semiconscious or Unconscious Patient
• Measure the blood glucose level (as previously discussed).
• Administer 50% dextrose, 25 to 50 mL intravenously for adult patients. In children, administer 25% dextrose; administer 10% to 12.5% dextrose to neonates and infants.
• Consider continuous infusion of 5% dextrose in water (D5W) or 10% dextrose in water (D10W) to maintain serum glucose within the normal range as prescribed. Cerebral edema is a rare but possible complication, especially in children.
When Intravenous Access Is Not Readily Available
• Administer glucagon 1 mg intramuscularly (0.5 mg in children ages 3 to 5 years; 0.25 mg in children less than 3 years).
• Glucagon should be prescribed for all individuals at significant risk of severe hypoglycemia and caregivers or family members of these individuals should be instructed in its administration. Glucagon administration is not limited to health care professionals.
Hyperglycemic Emergencies
Diabetic Ketoacidosis2,3,5–7
Etiology
• Blood glucose over 250 mg/dL
• pH less than 7.3 (metabolic acidosis)
• Serum HCO3 less than 15 to 20 mmol/L
DKA usually is limited to type 1 diabetic patients, but under conditions of extreme stress, it may occur in those with type 2 diabetes.2
Signs and Symptoms3
• Volume depletion: dry skin and poor skin turgor, dry mucous membranes
• Acute mental status changes from drowsiness to coma
• Acetone on the breath (fruity-smelling breath)
• Kussmaul respirations (rapid, deep breathing): the body is attempting to compensate for the metabolic acidosis by blowing off carbon dioxide
• Abdominal pain without rebound tenderness, diminished bowel sounds
Diagnostic Procedures
• Measure the serum glucose level. A fingerstick blood glucose test is adequate to begin treatment. (Obtain serum glucose to validate.)
• Test for glucose and ketones in urine.
• Obtain urinalysis (infection is a frequent precipitant of DKA).
• Obtain a complete blood count with differential, electrolytes, blood urea nitrogen (BUN), creatinine, phosphate, and amylase.
• Obtain a chest radiograph, 12-lead electrocardiogram (ECG), and blood cultures as indicated.
Therapeutic Interventions
Although the condition requires emergent intervention, correction that occurs too rapidly may result in cerebral edema, hypoglycemia, or hypokalemia.2
Fluid Replacement
• Restore intravascular volume and renal perfusion. Volume losses in DKA can be extensive. Total body fluid deficits average 6 L (adults) or 100 mL/kg of body mass. The exact rate will depend on the patient’s condition and response. Begin fluid replacement before initiating insulin therapy or electrolyte replacement.
• Administer normal saline at 1 to 2 L per hour over the first 1 to 2 hours and then at 100 to 500 mL per hour for adults. For pediatric patients, replace 20 mL/kg of body mass in the first hour. More aggressive fluid replacement is indicated if the patient is in hypovolemic shock.
• Change intravenous (IV) solution to 0.45% saline if hypovolemia has been reversed and the serum sodium level is still high or normal.
Reverse Ketonemia and Hyperglycemia and Administer Insulin
• Administration of IV insulin is recommended; injected insulin is absorbed erratically in the presence of hypovolemia. The treatment of choice for moderate to severe DKA is regular insulin by continuous IV infusion.
• Give an IV bolus of 0.1 units of regular insulin per kilogram of body mass and then start a continuous IV infusion at 0.1 unit/kg per hour.8 Prime the tubing and discard the first 30 to 50 mL of the insulin–normal saline solution because insulin binds to plastic.
• Measure serum glucose hourly. Too rapid a decrease in serum glucose will increase the risk of cerebral edema. Many institutions have implemented insulin protocols to guide the titration of the insulin infusion according to glucose levels. When serum glucose falls to 250 mg/dL, consider changing the IV fluid to a dextrose-containing solution (e.g., D5W/0.45% saline) and decreasing the insulin according to physician order to maintain a serum glucose level of 150 to 200 mg/dL. Depending on the insulin type, subcutaneous insulin therapy must be initiated 1 to 4 hours before discontinuation of the IV insulin infusion to avoid recurrence of hyperglycemia and ketogenesis.
Replace Electrolytes
• Measure serum electrolytes at the time of patient arrival and every 2 to 4 hours thereafter. In most cases the serum potassium level initially will be elevated. Fluid resuscitation, insulin therapy, and acidosis correction reduce extracellular potassium levels.
• Once serum potassium is less than 5 mEq/L, begin IV potassium replacement to keep blood levels between 4 and 5 mEq/L. If the initial serum potassium is less than 3.3 mEq/L, delay insulin therapy and start potassium replacement immediately.
• Begin potassium replacement only after it has been established that the patient has adequate urine output and is not in renal failure.
• Phosphate replacement also may be necessary.
• Sodium bicarbonate can be given intravenously if the arterial pH is 7 or less.
Hyperosmolar Hyperglycemic Syndrome or State2,3,5,7
Formerly known as hyperosmolar hyperglycemic nonketotic coma, hyperosmolar hyperglycemic syndrome (HHS) accounts for 10% to 20% of hyperglycemic emergencies and is associated with a 10% to 60% mortality, depending on the severity of the precipitating illness2 (Table 29-2).
TABLE 29-2 COMPARISON OF DIABETIC KETOACIDOSIS AND HYPEROSMOLAR HYPERGLYCEMIC SYNDROME PATIENT PRESENTATIONS
| FEATURE | DIABETIC KETOACIDOSIS | HYPEROSMOLAR HYPERGLYCEMIC SYNDROME |
|---|---|---|
| Patient’s age | Usually <40 years | Usually >60 years |
| Duration of symptoms | Usually <2 days | Usually >5 days |
| Glucose level | Usually <600 mg/dL | Usually >600 mg/dL |
| Sodium level | Likely to be low or normal | Likely to be normal or high |
| Potassium level | High, normal, or low | High, normal, or low |
| Bicarbonate level | Low | Normal |
| Ketone bodies | At least 4+ in a 1 : 1 dilution | <2+ in a 1 : 1 dilution |
| pH | Low, usually <7.3 | Normal |
| Serum osmolality | Usually <350 mOsm/kg | Usually >350 mOsm/kg |
| Cerebral edema | Often subclinical, occasionally clinical | Rapid glucose decline increases the risk |
| Prognosis | 3% to 10% mortality | 20% to 60% mortality |
| Subsequent course | Ongoing insulin therapy usually required | Insulin therapy often not required |
| Diabetes mellitus | Most commonly seen with type 1 | Most commonly seen with type 2 |
Diagnostic Procedures
• Hyperglycemia greater than 600 mg/dL
• Elevated plasma osmolality greater than 315 mOsm/kg
• Serum bicarbonate greater than 15 mEq/L
• Arterial pH within normal limits
Therapeutic Interventions.2,3
Treatment is similar to DKA (see above), though less insulin is needed.
Replace Fluids
• The average fluid deficit is 9 to 12 L. Begin fluid resuscitation with 1 L of normal saline over the first hour to restore blood pressure and urine output. Change to 0.45% saline at 5 to 15 mL/kg per hour if the serum sodium level is normal or high.
• Insert an indwelling urinary catheter to strictly monitor intake and output. Incorporate urinary losses into fluid replacement calculations.
Serum Glucose Reduction
• Administer insulin: The goal of insulin therapy in patients with HHS is to reduce serum glucose levels by around 50 to 70 mg/dL per hour.
• When the blood glucose drops to 300 mg/dL, change to a dextrose-containing IV solution such as D5W/0.45% saline. Adding dextrose to IV fluids reduces the risk of cerebral edema associated with rapid decreases in serum glucose levels.
Pituitary Emergencies
Diabetes Insipidus6

 cup regular soda (avoid in patients with renal failure)
cup regular soda (avoid in patients with renal failure) cup orange juice (avoid in patients with renal failure)
cup orange juice (avoid in patients with renal failure) cup apple juice
cup apple juice oz box of raisins
oz box of raisins







