Chapter 47 Meningitis and encephalomyelitis
Infections of the cranial contents can be divided into those which affect the meninges (meningitis) and those which affect the brain parenchyma (encephalitis). Chronic, insidious or rare infections are beyond the scope of this chapter, which will focus on acute bacterial and viral causes of meningitis and encephalomyelitis.
BACTERIAL MENINGITIS
GENERAL POINTS
The bacterial organisms are usually not confined to the brain and meninges and frequently cause systemic illness, for example, severe sepsis, shock, acute respiratory distress syndrome, and bleeding disorders such as disseminated intravascular coagulation.1,2
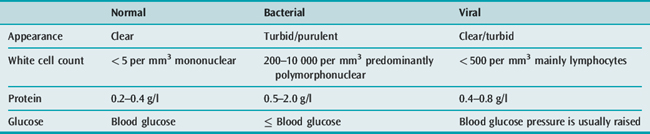
These features raise the possibility of an undiagnosed cerebral mass lesion which, in turn, could cause cerebral herniation if lumbar puncture is performed. A computed tomography (CT) brain scan is required prior to CSF examination in order to explore this possibility and lessen but not obviate the risk of cerebral herniation. Even if the CT brain scan is normal, ICP may still be raised. The importance of performing a safe CSF examination must be balanced against the need to commence immediate treatment in each individual patient.3,4
AETIOLOGY
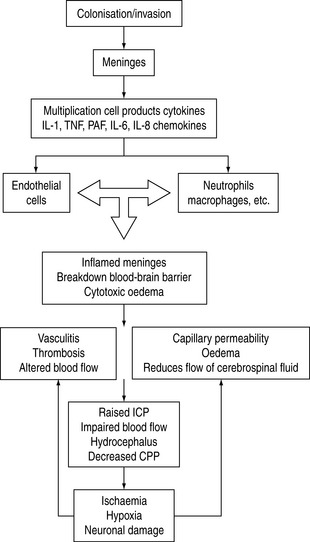
The main causes of meningitis are spread by droplet infection or exchange of saliva. Meningitis may occur when pathogenic organisms colonise the nasopharynx and reach the blood–brain barrier. Meningitis can occur as a result of infection in the middle ear, sinus or teeth, leading to secondary meningeal infection. Most bacteria obtain entry into the CNS via the haematogenous route. As the organisms multiply, they release cell wall products and lipopolysaccharide, and generate a local inflammatory reaction which in itself also releases inflammatory mediators. The net result of the release of cytokines, tumour necrosis factor and other factors is associated with a significant inflammatory response. Vasculitis of CNS vessels, thrombosis, cell damage and exudative material all contribute to vasogenic and cytotoxic oedema, altered blood fiow and cerebral perfusion pressure. Later on infarction and raised ICP occur.5
The inflammatory events seen with infection are summarised in Figure 47.1.
ORGANISMS
Until the advent of the meningitis vaccination programme, H. infiuenzae type B was the most common cause of bacterial meningitis. Recently S. pneumoniae and N. meningitidis have been considered the main causes, although one study suggested that Listeria monocytogenes is the second most common isolate in adult population. The occurrence of pneumococcal strains which are resistant to penicillin has also influenced the epidemiology of meningitis.6
IMMUNOCOMPROMISED HOSTS
In the immunocompromised patient with meningitis (e.g. human immunodeficiency virus: HIV), fungal viral and cryptocococal meningitis should be considered.7
CLINICAL PRESENTATION
It is important to identify from the history reported about preceding trauma, upper respiratory tract infection or ear infection. Symptoms may develop over hours or days. Specific infections relate partly to an individual’s age.
INVESTIGATIONS
The patient with suspected bacterial meningitis requires immediate blood cultures and should be given empirical intravenous (IV) antibiotics if there is likely to be any delay in further assessment (Table 47.1).
MANAGEMENT
Antibiotics should be started as early as possible and broad-spectum coverage is recommended until bacterial identifcation is made (Table 47.2). The selection of antibiotics is influenced by the clinical situation in conjunction with known allergies or local patterns of antibiotic resistance and the CSF findings. Delays in administering antibiotics are a significant risk factor for a poor prognosis. In the absence of a known organism, empirical choice for antibiotics has been complicated by the development of resistant strains. Penicillin G, ampicillin and third-generation cephalosporins are typical first-line agents. Until recently, ampicillin was appropriate for pneumococcal, meningococcal and Listeria infections. The emergence of resistant strains influences local antibiotic practice. If there is a history of recent head injury, a broad-spectrum cephalosporin may be indicated with vancomycin. Discussions with local microbiology services are recommended. If the CSF examination identifies the organism, then specific regimens can be prescribed (Table 47.3).
Table 47.2 Empiric antibiotics for meningitis
| Indication | Antibiotic | Dose |
|---|---|---|
| <50 years | Ceftriaxone or cefotaxime | 2–4 g q 24 h 2 g q 4 h |
| >50 years or impaired cell immunity | Ceftriaxone or cefotaxime | 2–4 g q 24 h 2 g q 4 h |
| Cefotaxime + ampicillin or penicillin G | 2 g q 4 h or 3–4 MU q 4 h | |
| Drug-resistant Streptococcus pneumoniae | Ceftriaxone + rifampicin | 2–4 g q 8 h 2 g q 4 h |
| or vancomycin | 0.5 g q 6 h | |
| Neurosurgery shunts trauma | Ceftazidime + nafcillin or | 2 g q 8 h 2 g q 4 h |
| Vancomycin + aminoglycoside | 0.5 g q 6 h 2 mg / kg q 8 h | |
| (gentamicin 5–7 mg/kg stat) |
Table 47.3 General recommendation for known organisms*
| Organism | Antibiotic | Second line or allergy |
|---|---|---|
| Streptococcus pneumoniae (Penicillin-resistant) | Ceftriaxone + vancomycin or rifampicin | Vancomycin + rifampicin |
| Streptococcus pneumoniae (Penicillin-sensitive) | Penicillin G | Ceftriaxone or chloramphenicol |
| β-haemolytic streptococcus | Penicillin or ampicillin | Cefotaxime or chloramphenicol or vancomycin |
| Haemophilus influenzae | Ceftriaxone or cefotaxime | Chloramphenicol |
| Neisseria meningitidis | Penicillin G | Ceftriaxone or chloramphenicol |
| Listeria monocytogenes | Ampicillin + gentamicin | Trimethoprim + sulfamethoxazole |
| Enterobacteriaceae | Ceftriaxone + gentamicin | Quinolones |
| Pseudomonas aeruginosa | Ceftazidime + tobramycin | Quinolones |
* Always check local sensitiviity as resistance patterns are variable.
It is more difficult to select an appropriate empirical antibiotic in the immunocompromised patient. When the organism has been identified and sensitivity results are available, it may be necessary either to change the antibiotic or to rationalise those being given.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree