![]() Suspected compartment syndrome
Suspected compartment syndrome
![]() Rising creatine phosphokinase (CPK) level without a source in the setting of trauma
Rising creatine phosphokinase (CPK) level without a source in the setting of trauma
CONTRAINDICATIONS
![]() Relative Contraindications
Relative Contraindications
![]() Overlying skin cellulitis
Overlying skin cellulitis
![]() Coagulopathy
Coagulopathy
RISKS/CONSENT ISSUES
![]() Pain (site of needle insertion)
Pain (site of needle insertion)
![]() Bleeding (local at needle puncture site)
Bleeding (local at needle puncture site)
![]() Infection (theoretical risk of iatrogenic infection)
Infection (theoretical risk of iatrogenic infection)
![]() General Basic Steps
General Basic Steps
![]() Sterilize field
Sterilize field
![]() Provide analgesia
Provide analgesia
![]() Zero apparatus
Zero apparatus
![]() Measure pressure in desired compartment
Measure pressure in desired compartment
LANDMARKS/RELEVANT ANATOMY
![]() The forearm consists of three compartments (FIGURE 54.1). All compartments are entered one-third of the way from the elbow to the wrist with the arm at heart level and in supination (palm up). At this level, the posterior border of the ulna is easily palpated, just distal to the elbow.
The forearm consists of three compartments (FIGURE 54.1). All compartments are entered one-third of the way from the elbow to the wrist with the arm at heart level and in supination (palm up). At this level, the posterior border of the ulna is easily palpated, just distal to the elbow.
![]() The volar (palmar) compartment contains the wrist and finger flexors. The needle entry is medial to palmaris longus tendon, 1 to 2 cm deep.
The volar (palmar) compartment contains the wrist and finger flexors. The needle entry is medial to palmaris longus tendon, 1 to 2 cm deep.
![]() The dorsal compartment contains the wrist and finger extensors. The needle entry is 1 to 2 cm lateral to the posterior ulna border, 1 to 2 cm deep.
The dorsal compartment contains the wrist and finger extensors. The needle entry is 1 to 2 cm lateral to the posterior ulna border, 1 to 2 cm deep.
![]() The mobile wad contains the brachioradialis and radial flexors of the wrist. Needle insertion is 1 to 1.5 cm into the muscle, which laterally overlies the radius.
The mobile wad contains the brachioradialis and radial flexors of the wrist. Needle insertion is 1 to 1.5 cm into the muscle, which laterally overlies the radius.
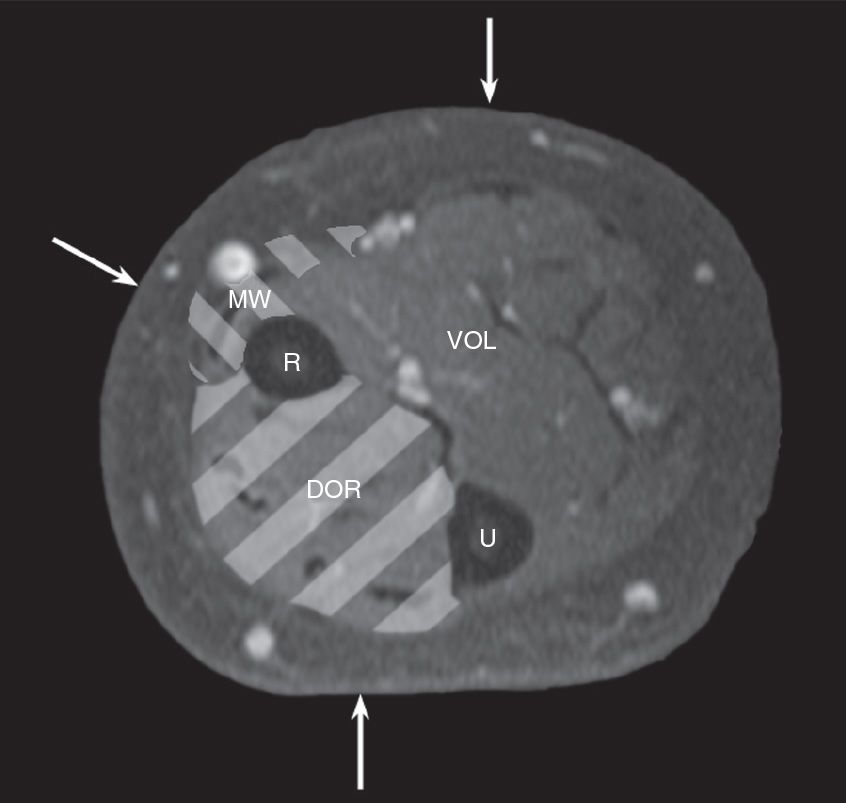
FIGURE 54.1 The three compartments of the forearm. R, radial bone; U, ulna bone; VOL, volar compartment; DOR, dorsal compartment; MW, mobile wad.
![]() The buttock contains three compartments: One containing the tensor fascia lata; one containing gluteus medius and minimus; and one containing the gluteus maximus.
The buttock contains three compartments: One containing the tensor fascia lata; one containing gluteus medius and minimus; and one containing the gluteus maximus.
![]() Landmarks vary from person to person
Landmarks vary from person to person
![]() In all cases, the needle should be at the point of maximal tenderness
In all cases, the needle should be at the point of maximal tenderness
![]() The thigh is composed of two compartments; the needle is easily passed into the point of maximal tenderness
The thigh is composed of two compartments; the needle is easily passed into the point of maximal tenderness
![]() The anterior contains the quadriceps and femoral neurovascular bundle
The anterior contains the quadriceps and femoral neurovascular bundle
![]() The posterior contains the hamstring group and the sciatic nerve, which gives rise to the common tibial and common fibular nerve
The posterior contains the hamstring group and the sciatic nerve, which gives rise to the common tibial and common fibular nerve
![]() The leg contains four compartments (FIGURE 54.2). All compartments are entered one-third of the way from the knee to the ankle with the leg at heart level.
The leg contains four compartments (FIGURE 54.2). All compartments are entered one-third of the way from the knee to the ankle with the leg at heart level.
![]() The anterior compartment contains the tibialis anterior, responsible primarily for dorsiflexion of the foot, and the toe extensors; this compartment is most commonly affected by compartment syndrome. The needle entry is 1 cm lateral to the anterior border of the tibia, 1 to 3 cm deep, while the patient is supine.
The anterior compartment contains the tibialis anterior, responsible primarily for dorsiflexion of the foot, and the toe extensors; this compartment is most commonly affected by compartment syndrome. The needle entry is 1 cm lateral to the anterior border of the tibia, 1 to 3 cm deep, while the patient is supine.
![]() The deep posterior compartment contains the tibialis posterior muscle (which inverts the foot) and the toe flexors. The needle entry is posterior to the medial border of the tibia, angled toward the posterior border of the fibula, 2 to 4 cm deep, with the patient supine.
The deep posterior compartment contains the tibialis posterior muscle (which inverts the foot) and the toe flexors. The needle entry is posterior to the medial border of the tibia, angled toward the posterior border of the fibula, 2 to 4 cm deep, with the patient supine.
![]() The superficial posterior compartment contains the plantar flexors of the foot—the soleus, gastrocnemius, and plantaris muscles, as well as the sural nerve. The needle entry is either side of the midline of the calf, 2 to 4 cm deep, with the patient prone.
The superficial posterior compartment contains the plantar flexors of the foot—the soleus, gastrocnemius, and plantaris muscles, as well as the sural nerve. The needle entry is either side of the midline of the calf, 2 to 4 cm deep, with the patient prone.
![]() The lateral compartment is located anterolaterally and contains the foot everters as well as the fibular nerve. The needle entry is just anterior to the posterior border of the fibula, 1 to 1.5 cm deep, with the patient supine.
The lateral compartment is located anterolaterally and contains the foot everters as well as the fibular nerve. The needle entry is just anterior to the posterior border of the fibula, 1 to 1.5 cm deep, with the patient supine.
TECHNIQUE
![]() Preparation
Preparation
![]() Choose the most appropriate method for compartment measurement
Choose the most appropriate method for compartment measurement
![]() Remove possible offending factors (i.e., cast, tourniquet)
Remove possible offending factors (i.e., cast, tourniquet)
![]() Identify point of maximal tenderness to palpation
Identify point of maximal tenderness to palpation
![]() Variety of tonometers are commercially available
Variety of tonometers are commercially available
![]() Alternatively, measurements can be made using an arterial-line assembly
Alternatively, measurements can be made using an arterial-line assembly
![]() Assemble materials
Assemble materials
![]() Arterial-line assembly, transducer, monitor, and stand
Arterial-line assembly, transducer, monitor, and stand
![]() An 18-gauge side-port needle or slit catheter
An 18-gauge side-port needle or slit catheter
![]() Set up the arterial-line transducer and apparatus as would be for inserting an arterial line
Set up the arterial-line transducer and apparatus as would be for inserting an arterial line
![]() Attach the side-port needle or slit catheter to the arterial-line assembly and flush
Attach the side-port needle or slit catheter to the arterial-line assembly and flush
![]() Zero the apparatus at the level of the compartment
Zero the apparatus at the level of the compartment
![]() Select your entry site and cleanse it with iodine solution or chlorhexidine. Allow to dry.
Select your entry site and cleanse it with iodine solution or chlorhexidine. Allow to dry.
![]() Administer local anesthesia and/or systemic analgesia as appropriate (avoid injection of muscle or fascia as this can affect measurements)
Administer local anesthesia and/or systemic analgesia as appropriate (avoid injection of muscle or fascia as this can affect measurements)
![]() Insert the needle into your selected compartment, perpendicular to the skin
Insert the needle into your selected compartment, perpendicular to the skin
![]() For fractures, insert at level of the fracture (±5 cm)
For fractures, insert at level of the fracture (±5 cm)
![]() Feel the “pop” as you enter the compartment through the deep fascia
Feel the “pop” as you enter the compartment through the deep fascia
![]() Verify placement by gently compressing the compartment distal to the needle
Verify placement by gently compressing the compartment distal to the needle
![]() Record the mean pressure (allow needle to equilibrate)
Record the mean pressure (allow needle to equilibrate)
![]() Remove the needle from the compartment, inspect and flush as needed
Remove the needle from the compartment, inspect and flush as needed
![]() Repeat the measurement of the same compartment
Repeat the measurement of the same compartment
![]() Cover puncture site with a clean, dry dressing
Cover puncture site with a clean, dry dressing
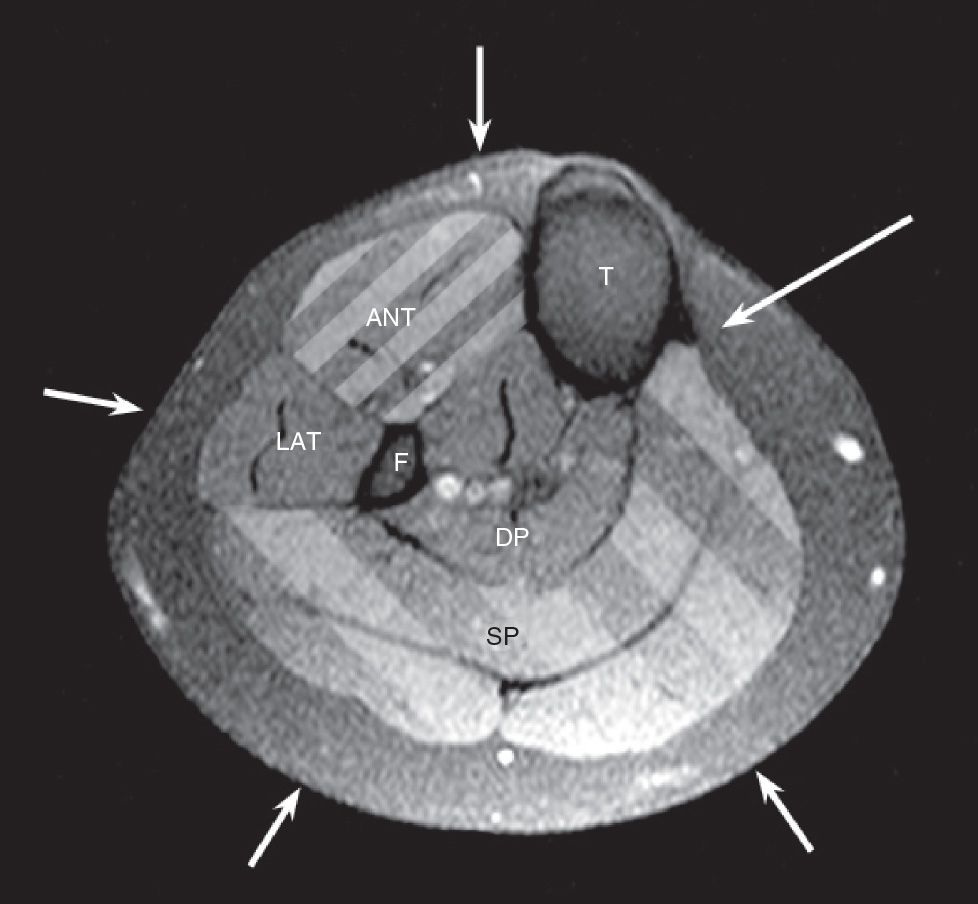
FIGURE 54.2 The four compartments of the leg. T, tibial bone; F, fibula bone; ANT, anterior compartment; LAT, lateral compartment; DP, deep posterior compartment; SP, superficial posterior compartment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


