
Maxillofacial Injuries
Katie Sprinkel and Stephen Colucciello
There is substantial regional variation in the etiology of facial trauma, and in the developed world interpersonal violence has surpassed motor vehicle collisions (MVCs) as the most common cause of facial fractures (1). The use of seat belts as restraint devices in vehicles has been repeatedly shown to result in a decreased incidence of facial lacerations and fractures, whereas the protective effect of airbags is less clearly established in facial trauma (2). Other causes include falls, sports injuries, and gunshot wounds, with gunshot wounds and MVCs resulting in the highest injury severity (1). The most frequently fractured facial bones in descending order are the nasal bones, orbital floor, zygomaticomaxillary complex, maxillary sinuses, and mandibular ramus (1).
CLINICAL PRESENTATION
The presentation of maxillofacial trauma depends largely on the mechanism of injury; understanding the mechanism of injury can aid in predicting the severity and risk for associated injuries. Patients who sustain significant blunt trauma (e.g., MVC) often suffer multiple injuries, and their initial evaluation and stabilization should follow a standard trauma protocol. Neglecting potentially serious chest, abdominal, or pelvic injuries in the multiple-trauma patient with distracting facial deformity is a dangerous error. Facial injuries in women in particular are a marker for intimate partner violence, which is underreported and should be investigated when taking the patient’s history. Studies estimate between 1/3 and 2/3 of women who present with facial trauma are victims of intimate partner violence (IPV), and the most common injuries are to the midface (3). Overall, assaults most frequently involve young males as the perpetrators with alcohol being the main contributing factor. Mandibular, orbital floor, nasal, and zygomaticomaxillary complex fractures most commonly result from assault, whereas MVCs tend to cause more complex midface injury patterns (1).
Victims of penetrating maxillofacial trauma are less likely to have serious injuries to distant organ systems but may experience injury to the globe, brain, or neck. High-velocity injuries have a high rate of airway compromise, with nearly a third requiring urgent airway control, either intubation or a definitive surgical airway (4). The emergency physician must be particularly attuned to both central nervous system (CNS) and vascular injury in penetrating trauma as well.
Airway compromise and management of hemorrhage are the most urgent concerns in maxillofacial injury. Airway problems can result from a posteriorly displaced tongue, dislodged teeth, oral hemorrhage and vomitus, or injury to the soft tissues surrounding the airway. A decision for definitive airway control is based on the patient’s level of consciousness, severity of injury, risk for aspiration or airway obstruction by delayed edema, and hematoma formation (5). Clinicians who elect to perform blind nasotracheal intubation should be aware of the rare risk of intracranial placement of the endotracheal tube (6). The risk of delayed airway compromise has prompted some authors to recommend intubating patients who present with significant intraoral blood or moderate-sized hematomas in the neck or face, although definitive support in the literature is lacking (7). For patients who require transfer for definitive care, the emergency physician should consider the risk of developing airway compromise en route to the trauma center and complications may increase with the length of transport. When in doubt, it is best to obtain a definitive airway prior to transport. Given the significant vascularity of facial structures, maxillofacial trauma may infrequently result in enough blood loss to cause hypotension and, rarely, exsanguination. The incidence of severe hemorrhage ranges from 1% to 11%, with the highest incidences occurring in patients with midfacial fracture (8,9). The tamponade effect of the facial musculature combined with the relative accessibility for direct pressure makes life- threatening hemorrhage in adults relatively uncommon.
DIFFERENTIAL DIAGNOSIS
The sometimes dramatic appearance of facial trauma may distract the examining physician from more serious injuries. Once the airway is ensured and brisk facial bleeding controlled, other life threats must be quickly and systematically excluded. Then, the emergency physician should attempt to specifically address bony and soft tissue facial injuries.
Brain injury is the most common associated injury, occurring in up to 79% of patients with single facial fracture, and 88% of patients with two or more facial fractures (10). Previously, some suggested that facial fractures may decrease the risk for intracranial injury. Recent evidence supports the contrary, noting that patients with facial fractures, especially involving the midface, actually have an increased risk of traumatic brain injury (10). This link suggests that the clinician should have a low threshold for performing head computed tomography (CT) in patients with any facial fracture, especially those who have altered mental status, neurologic deficit, or perhaps a worrisome mechanism of injury. The converse is also true. In one study, 10% of comatose blunt trauma victims had significant unsuspected facial bone fractures that were diagnosed by routine facial CT (11).
The incidence of concomitant cervical spine fracture in the setting of facial fracture is not insignificant, reports range from 1% to 8% with that number increasing with number of facial fractures (10,11). The use of the Nexus or Canadian Cervical Spine Rules provides evidence-based guidelines for cervical radiography and the presence or absence of a facial fracture alone should not determine the need for cervical spine imaging unless it is considered a “distracting injury.” See Chapter 28, “Cervical Spine Fractures” (12). There is some data to suggest that facial fracture is a risk factor for injury to the carotid or vertebral vessels, which is more frequent in blunt trauma than previously recognized. Recent guidelines recommend imaging (CT angiography) to screen for cerebrovascular injury if the patient has displaced midface or complex mandibular fractures (13).
Loss of vision is another significant concern, occurring in as high as 6% of maxillofacial trauma. Visual testing and red color perception are the most useful tests but not always possible in the unconscious patient. Pupillary size and shape, reactivity to light, lid lacerations and globe tension to palpation may also reveal important clues to ocular or periorbital injury (14,15).
ED EVALUATION
Aside from airway concerns, maxillofacial injuries are seldom life threatening. However, other organ system injuries carry significant morbidity and potential mortality. After resuscitation and addressing significant injuries to other organ systems, the emergency physician should perform a thorough and directed examination of the face. Anatomic complexity, swelling, lacerations, pain, and altered level of consciousness pose challenges to an optimal physical examination. A systematic approach can help surmount these challenges.
A complete history, including specifics about the mechanism of injury, should be obtained, ensuring that certain injuries are not overlooked. High-yield general questions include the presence of loss of consciousness, facial numbness, weakness, and visual disturbances. Specifically, for periorbital injuries, the emergency physician should ask about blurred vision, pain on extraocular motion, and diplopia. Monocular diplopia indicates a problem with the lens or retina in a single eye; binocular diplopia that involves eye movement suggests nerve palsy, muscle injury, or entrapment. For midface and jaw injuries, ask about dental malocclusion and trismus.
The emergency physician should begin with inspection and evaluate the patient from multiple perspectives. This should include both the “bird’s eye view” as well as the “worm’s eye view,” which involves inspection from above and below to reveal subtle facial asymmetries. Loss of contours, edema, ecchymosis, and hemorrhage are clues to soft tissue and underlying bony injuries (eFig. 23.1). Facial elongation in the frontal plane can occur with high-grade Le Fort fractures (“donkey” facies) (16). Ecchymoses around the eyes (raccoon eyes) and over the mastoid areas (Battle’s sign) are associated with basilar skull fractures. Raccoon eyes, which usually take several hours to develop, are nonspecific and may be associated with nasoorbitoethmoid (NOE) injuries, Le Fort, orbital, and frontal bone fractures. Facial function is tested by examining the muscles of facial expression. Patients should be asked to close their eyes tightly, raise their eyebrows, purse their lips, smile, and frown. Fractures of the temporal bone may be associated with a posttraumatic Bell palsy with weakness of the facial muscles on the affected side (16). Difficulty with opening and closing the mouth may be secondary to jaw muscle spasm, or it is less commonly associated with fractures of the mandible, zygoma, or maxilla. Evaluating extraocular motions is just as important as testing facial function. Inability to gaze upward or downward, exophthalmos, or enophthalmos can be associated with periorbital fractures. Pain with extraocular movements suggests an occult periorbital fracture. The eye examination should encompass visual acuity, examination of the anterior chamber and pupil, extraocular motions, ptosis, periorbital sensation, and the swinging flashlight test to assess for a Marcus Gunn pupil (see Chapter 25). The ear canal is inspected for any lacerations or clear fluid leak that may represent cerebrospinal fluid (CSF). Using an otoscope, the tympanic membrane is examined for evidence of rupture or hemotympanum, seen as a purplish bulge of the membrane. This finding is associated with basilar skull fracture and fractures of the mandibular condyles. The external ear is examined for otohematomas, which can result in chronic deformity called “cauliflower ear.” In the nose, the most important findings include septal hematoma and CSF rhinorrhea. A septal hematoma is a bluish colored, bulging septal mass that is tender and boggy to palpation.
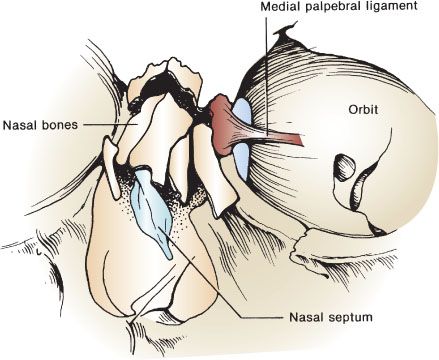
FIGURE 23.1 Nasoethmoidal fractures.
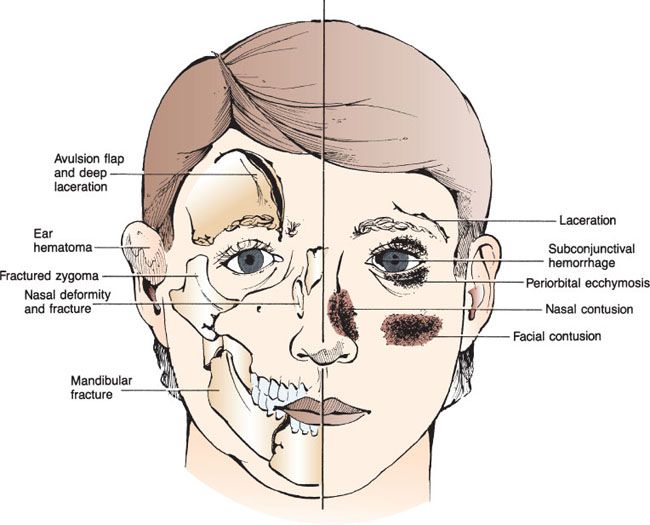
eFIGURE 23.1 Superficial facial injuries provide important visual clues to underlying soft tissue and bony injuries.
The emergency physician should consider testing bloody nasal discharge for CSF. A drop of the bloody fluid containing CSF will demonstrate a target or “halo sign” when placed on a paper towel or bed sheet, because the CSF migrates farther and faster than blood. This test can produce false-negative results with non-CSF fluids mixed with blood, whereas glucose and β-2 transferrin testing are more specific for CSF (10).
Palpation is another important part of the physical examination. The entire face should be palpated for tenderness, step-offs, bony crepitus, and subcutaneous air (often present with fractures involving the sinus). Facial stability is tested by placing a gloved hand in the patient’s mouth, grasping the hard palate, and rocking back and forth while the other hand simultaneously palpates the central face. The physician should be careful to not rock the teeth themselves if dental trauma exists, as dental avulsion may occur.
The final part of the examination of the face is a test for sensation. The branches of the trigeminal nerve are commonly disrupted or contused during facial injury and can cause sensory deficits to the face. The V1 branch of the trigeminal nerve is particularly susceptible to injury in the supraorbital notch. Damage to this nerve can result in anesthesia of the upper nose, eyebrow, and forehead. The infraorbital nerve can be disrupted as it courses through the floor of the orbit and is frequently damaged with orbital or zygomatic fractures. This results in ipsilateral numbness of the lower eyelid, side of the nose, upper lip, gums, and hard palate. Finally, the mental nerve can be injured when there is a mandibular injury resulting in ipsilateral anesthesia to the chin. The presence of facial anesthesia does not necessarily confirm a facial fracture; contusion to the nerve alone can produce similar numbness.
While plain radiographs (e.g., a Waters view, or occipitomental view, for midface fracture) may be effective as a screening tool for some facial fractures, there has been a gradual shift away from this modality (17). Ultrasound has been shown to have diagnostic value, recognizing its limitations with nondisplaced and complex fractures, especially in posterior orbital floor and mandibular condyle where sensitivity is especially low. Data is most impressive for nasal bone fractures, with a sensitivity of 90% to 100% and specificity of 98% to 100% with ultrasound (18). CT, however, is the gold standard for imaging in cases where there is concern for facial fracture with superior sensitivity, speed, cost, and utility in surgical planning (17). Interestingly, several studies have shown that the noncontrasted head CT ordered primarily for ruling out intracranial trauma, has the added advantage of evaluating for orbital, maxillary, and zygomatic fractures, citing sensitivities of 90% to 100% (19,20). The decision to add facial CT to a patient already undergoing head CT can be augmented by specific physical examination findings. Aid in the decision to add a facial CT to a patient’s planned head CT may come from the knowledge that 12% of trauma patients who require a head CT will have facial fractures as well as the fact that complicated orbital fractures may not be fully delineated on isolated head CT (21).
KEY TESTING
• Airway assessment and attention to hemorrhage take precedent, vision-threatening injury should also be evaluated with an ocular examination.
• If suspicion for facial fracture exists based on physical examination, facial CT is the gold standard imaging modality (17).
• Ultrasound shows promise in the diagnosis of facial fracture, in particular there is data showing nasal bone fractures, orbital fractures, anterior maxillary wall, and zygomatic arch fractures can be readily detected (18).
• Head CT should be strongly considered in any patient with facial fracture given the high incidence of concomitant intracranial injury.
• Facial fracture is also a marker of increased risk for cervical spine fracture in trauma, adherence to clinical decision rules is appropriate to determine need for cervical spine imaging.
• CT angiography (16-slice scanner) is recommended to screen for cervical vessel injury with displaced midface and complex mandible fractures (13).
ED MANAGEMENT
Fractures, bleeding, edema, and foreign bodies (such as loose teeth) may occlude the airway and distort anatomy minutes to hours after injury. Thus, it may be prudent to prophylactically secure the airway in patients with evidence of progressive swelling using rapid-sequence orotracheal intubation or an awake intubation. In patients with significant facial trauma, equipment for “backup” cricothyrotomy should be readily available as several factors may qualify them as “difficult airways.” These factors should be assessed prior to any intubation attempt, including the potential for poor mask seal precluding effective bag-valve-mask ventilation, cervical spine immobilization, and loss of normal landmarks with bony, soft tissue, and vascular injury.
The patient’s position on the stretcher dramatically affects the airway. Sitting up and leaning forward is the “position of life” as it clears the airway of blood and displaces any fractured bones or loose tissue forward. The patient can even self-suction blood with one or two Yankauer suction catheters. However, this position is not an option if there is significant concern for cervical spine injury.
Maxillofacial trauma can compromise the airway at the nasal, oropharyngeal, or laryngeal level. If collapse of the nasal airway results from posteroinferior displacement of maxillary fractures, definitive control may be achieved by pulling the face forward using anterior traction on the maxilla (38). The maxillary arch should be grasped above the front teeth to avoid pulling them out of their loosened sockets. If a prolapsed tongue is occluding the oropharyngeal airway (often seen in central mandibular fractures), the tongue can be pulled forward with a traction suture or towel clip. Maxillofacial trauma may also occur in conjunction with direct trauma to the neck, causing airway collapse at the level of the larynx. Cricothyrotomy is possible if the level of injury is above the larynx. In patients with injuries at or inferior to the larynx, endotracheal intubation under direct laryngoscopy may be attempted, but emergency tracheostomy may be necessary. If tracheal injury is inferior to a level at which tracheostomy will provide an adequate airway, emergent consultation with an ENT or thoracic surgeon is warranted (22).
Once the airway is secure and breathing is stabilized, the “C” of the trauma ABCs must be addressed. Although some patients with maxillofacial trauma may be hypotensive, isolated facial injuries rarely cause shock (8). Hemodynamic compromise should be ascribed to other injuries until proven otherwise. The blood supply to the face involves both branches of the external and internal carotid arteries with several anastomoses between each. Generally, if there is ongoing hemorrhage, direct pressure should be applied both internally to the anterior nares and externally where indicated. Immediate manual reduction of fracture fragments or dislocations may also slow the bleeding. If there is continued blood loss despite these maneuvers, particularly if there is massive nasopharyngeal bleeding, hemorrhage control may be achieved by using posterior nasal packing with either gauze, Foley catheter, or a commercially available nasal balloon (8). Care should be taken with posterior nasal packing to avoid the risk of intracranial placement. The McKesson prop, which is a rubber stopper placed in between the upper and lower teeth to push the midface upward, has also been proposed as a temporizing measure to tamponade bleeding from severe midface fractures (17). Seldom, with maxillary fractures, the posterior pharynx may need to be packed after endotracheal intubation. If hemorrhage continues, arterial ligation or embolization should be pursued (8).
Frontal Bone Fractures
The frontal bone is the strongest bone in the face, consisting of a thick anterior wall that can tolerate as much as 2200 lb of force, and a relatively thin posterior wall. Two-thirds of frontal bone fractures involve both anterior and posterior tables, and given the tremendous amount of force required to break these bones, the incidence of concomitant intracranial and other facial injury is high. These fractures also carry significant potential for infection (23). Therefore, patients with known or strongly suspected frontal bone fractures should undergo head CT scanning and meticulous evaluation for associated injuries, including orbital, nasal, and ethmoid fractures (24).
Frontal sinus injuries are often not obvious; suspicion is based on mechanism of injury (person’s head hits the dash of a car or assault with a heavy blunt object such as a brick). On inspection, the emergency physician should look for any depression of the forehead. Glabellar depression indicates fracture of the anterior wall of the frontal sinus. The presence of subcutaneous air indicates sinus disruption, and the supraorbital rims should be palpated for step-off or deformity. Palpation with a sterile gloved finger can help detect fractures that underlie open wounds. Though rare, posterior wall fractures may result without an anterior wall fracture (24). When testing sensation, it is important to realize that numbness in the distribution of the supraorbital nerve (forehead) may herald an occult fracture. CSF rhinorrhea, if present, indicates involvement of both the posterior wall and meninges (24). Some patients may present with postnasal drip as CSF may preferentially enter the oropharynx. Finally, all patients with frontal bone fractures deserve a thorough ophthalmologic examination due to high rate of concomitant injury.
Although plain films such as Waters and Caldwell views of the face can screen for fracture, if there is significant concern for fracture, axial and coronal CT is indicated to delineate the status of the posterior table and the nasal frontal outflow tract (14). Pneumocephalus is another significant finding which indicates dural violation (25).
Repair of the anterior wall of the frontal sinus can often be delayed; however, fracture of the posterior table requires urgent neurosurgical consultation. When the frontal sinus is fractured, prophylactic antibiotics are generally given. Commonly prescribed antibiotics include first-generation cephalosporins, erythromycin, trimethoprim–sulfamethoxazole, and amoxicillin-clavulanate. However, choice of antibiotics and when to start them is often left to the consultant. In addition, the presence of CSF rhinorrhea associated with frontal bone fractures usually prompts antibiotic prophylaxis by the consultant, although there has been conflicting evidence to the utility of this practice.
Orbital Fractures
Trauma to the orbital regions may range from simple soft tissue swelling around the eye to blindness. Immediate blindness from trauma is rare and is generally permanent, but delayed loss of vision is possible (15). A majority of blindness results from globe rupture; however, damage to the optic nerve (directly or indirectly) and retinal detachment can also lead to a loss of visual acuity. In addition, direct ocular trauma can produce a traumatic iritis. Injuries occurring as a result of trauma to the globe are discussed in detail in Chapter 25.
Fractures of the orbit are either “pure” or “impure.” Pure fractures affect only the internal orbit without orbital rim involvement, whereas impure fractures include the orbital rim. The blow-out fracture (eFig. 23.2) is a pure internal orbital fracture, usually involving the floor and medial portion of the orbit (24). These fractures occur with either direct force to the orbital rim or when a blunt force strikes the globe. Blow-in fractures consist of fractures and collapse of the orbital roof, which are strongly indicative of intracranial injury. If the fracture propagates to the orbital apex, it can place the optic nerve in jeopardy. This is called orbital apex syndrome and is an emergency if there are clinical or radiographic signs of optic nerve impingement (23).
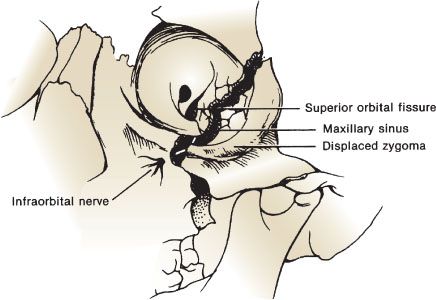
FIGURE 23.2 Zygomaticomaxillary complex fractures.









