Chapter 12
Manual therapy and influence on pain perception
By the end of the chapter the reader should have an appreciation of:
• MT in the context of biopsychosocial management of MSK pain
• the effects of MT on local tissue, spinal and supraspinal pain mechanisms
• the effects of pleasant touch on pain
• the effects of treatment-related pain on pain perception
• the effects of MT on motor control
INTRODUCTION
Manual therapy (MT) is considered to be a complex intervention from a clinical trials perspective (Dieppe 2004), so it is difficult to design methodologies that evaluate the specific effects, actions and interactions of the process. Although MT has non-specific effects, including placebo, it has a sound physiological basis to support its undoubted clinical effectiveness (Hoving et al 2006, UK BEAM 2004a). In the same way that movement is universal to the human condition, manually applied touch has an impact at every level of our physiology. Manually guided or passively produced movement influences local tissue healing, selectively influences afferent neurological stimulus, influences spinal and supraspinal moderation of afferent information, provides an experience of pain or pleasure, conveys an emotional context to physical sensation and signals actual or perceived threat. Consequently, establishing the precise elements of interventions that will target our patients’ specific needs and expectations is a combination of intuition, expert knowledge and refined communication with the patient. This highly attuned work means that MT can never be applied as a ‘one size fits all’ approach, which may account for the varying results in research trials.
THE RATIONALE OF MANUAL THERAPY
Manual therapies could conceivably boast the longest tradition in analgesic history, being reportedly undertaken in the earliest writings on medicine (Mattick & Wyatt 2000). While the magnitude of analgesic effect of MT may be less than, for instance, surgery or pharmaceutical opiates, it is a ubiquitous approach to MSK pain that can offer immediate pain relief (Wright 1995), improvements in tissue healing (Zusman 2010), reductions in anxiety and fear of movement (Gifford 2000), pleasurable and rewarding tactile stimulation (Leknes & Tracey 2008), increased motivation to replicate pain-relieving movement (Schultz 2002), and a window of opportunity to relearn pain-free movement memories through repetition and active involvement in the rehabilitation process (Zusman 2004, 2005). MT is associated with some minor adverse events (treatment soreness, which actually may be a component of its effect), but major adverse events are rare (Carnes et al 2010), and clinical and cost effectiveness are acceptable (UK BEAM 2004b). It is not surprising that MT approaches to pain relief continue to be undertaken by therapists with large proportions of MSK pain patients.
MANUAL THERAPY IN A BIOPSYCHOSOCIAL CONTEXT
We all move and to move is to change place, position or posture. The positions we adopt to allow full function are three-dimensional and continuously adapting to the functional demands placed on us. Naturally, the body cannot always immediately change to accommodate these demands and consequently short- and long-term dysfunction can result. In a system that continuously changes position and demands the acquisition of new and challenging positions, the integrated control of movement can be compromised. When movement has become dysfunctional, the body receives prompts to that effect (pain, restriction) and a change in state is registered. We unconsciously register that we are not moving efficiently and the value of this information is assessed and we adopt strategies to address this situation (cessation, adaptation). We can learn to reduce the pain by changing some aspect of the way we move and with time new movement patterns occur. If we have been unable to improve our movement and reduce pain, we may seek assistance from an expert in movement dysfunction such as a manual therapist (McCarthy 2010).
Movement dysfunction is a complex situation that must be considered in a biopsychosocial context. Our bodies are continuously moving from one starting position of movement to another. The point at which this process is considered dysfunctional is dependent on the perception of the individual (Pincus & Morley 2001). The psychological perspective of the individual and inter-related societal influences have a huge bearing on just when function is considered to have become dysfunctional. For some the body has become dysfunctional only as they undergo anaesthesia prior to surgery, for others when they develop an inkling that something is not quite right. Thus, the presentation of MSK dysfunction is incredibly variable.
Patients are people undertaking a therapeutic process of change to address a perceived problem. Thus, all patients have a perception that something is problematical, so we must assess them from a biopsychosocial perspective. Each patient will present with a biopsychosocial profile that will need to be carefully interpreted to allow the successful tailoring of intervention. Carefully weighted intervention, which targets important aspects of the patient profile, will optimally influence the patient’s perception of their problem. In other words, we cannot afford to look at a patient from only one perspective. The ability of our clinical examination to weigh the relative value of each domain of a patient’s biomechanical, physiological, psychological and social profile is vital for our practice (McCarthy 2010).
The model in Fig 12.1 shows the necessity of considering the psychological and social influences on patients attending with painful symptoms. Let us imagine a patient who has restricted movement of their L5/S1 lumbar motion segment, with this physiological impairment leading to the symptom of pain in the back. A manual therapist would quickly recognize this causal relationship, but a skilled manual therapist will evaluate the psychosocial influences on the perception, cause and maintenance of symptoms before instigating a strategy to change the symptoms. If, for example, the patient has had an excellent response to previous MT, has low levels of fear of movement and appropriate beliefs regarding causality, has a social environment encouraging recovery, and has no maladaptive coping strategies, the priority for treatment would be to address the biomechanical stressors and physiological impairment of the region. The techniques and explanations used would teach the patient that the local movement restriction was indeed minor as it responded to just a few seconds of stretching. The patient would learn that a simple stretch could reduce pain and limitation, and learn how to replicate this stretch as required. Any fear of movement would be reduced and self-efficacy facilitated, leading to reduced likelihood of reoccurrence. However, if the psychosocial influences on the patient were the opposite, treating the biomechanical stressors and physiological impairment would have an unpredictable, possibly deleterious, effect on symptoms.
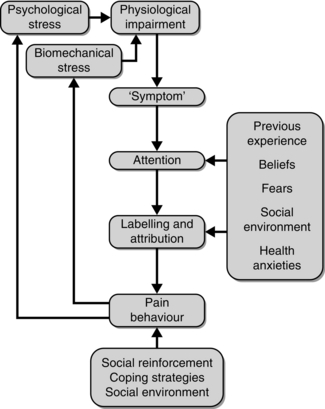
Fig. 12.1 Model of symptom, attention and stress in MSK pain. Reprinted from Watson, P.J. 2002, Psychophysiological models of pain, in Placebo and nocebo. Pain management. Muscles and pain Topical Issues in Pain, 4., CNS Press, Falmouth, UK, with permission.
The influence of the MT approach may become more predictable once maladaptive psychosocial influences have been addressed and when there is a realistic expectation that MT will be effective. Thus, addressing the physiological impairments in the absence of an appreciation of the patient’s psychosocial influences on perception will lead to unpredictable responses at best. By the same token, simply addressing the psychosocial influence on symptom perception without considering the physiological impairment of MSK dysfunction can also lead to unpredictable responses. Establishing how we accurately weigh and target the predominant barriers to recovery in our patient’s profile is our biggest challenge for the future of diagnostic practice (Billis et al 2007a,b, 2010, McCarthy 2003, McCarthy & Cairns 2005, McCarthy et al 2004, 2006).
There are many presentations of MSK dysfunction which suggest that a mechanically focused intervention may be the optimal strategy for treatment, for instance when the dysfunction has a strong relationship to the positions the body is held or moved into. Some of these appear to be more dominantly influenced by movement control than the psychosocial influences underpinning them. The quest to identify who is most suited to MT as opposed to other conservative therapies is currently being undertaken by researchers around the world (Childs et al 2004, 6, 7, 8), but patients make this judgement every day, based on their perceptions and expectations.
Healthcare behaviour has been compared with the interaction between child and mother in response to the child hurting itself (Gifford 2000). Firstly, the child will seek help from someone trustworthy; they will then receive attention and a diagnosis (mother has a look). Subsequently, they will receive reassurance and treatment (mother explains that it is nothing serious and rub it better) and finally be distracted from the pain and reactivated (mother makes the child laugh and sends them off to fetch the sweets). This process reduces fear, provides pleasant alternative stimulus (touch), reduces attention on the pain and focuses the attention on a task that can be achieved leading to reward. It will be very familiar to manual therapists and those who have experienced MT. MT is an interaction between patient and practitioner that involves the use of touch, specific movement, learning and reward. The interpretation of its effectiveness will be wholly governed by the biopsychosocial influences on the patient and practitioner. Untangling the individual components of this complex interaction is difficult and while our understanding of some underlying mechanisms is developing, their interactions are far from fully established.
Patients seek the intervention from manual therapists when their strategies for ameliorating pain and dysfunction have not met their own expectations. Thus, patients attend some time after their painful dysfunction has first been perceived. This is more than enough time for the nervous and therefore MSK systems to have adapted physiologically to the painful afferent stimuli (DeLeo 2006, Ren & Dubner 1999). MT approaches influence physiological processes within the higher centres of the central nervous system. It can help our management of the patient when we have even a basic understanding of the mechanisms involved.
MECHANISMS OF PAIN RELIEF THROUGH MANUAL THERAPY
In conjunction with a detailed examination of the specific biomechanical and physiological impairments of a MSK dysfunction, the manual therapist has several ways to alter the perception of pain at their disposal (Table 12.1).
Table 12.1
Theoretical processes in pain relief with manual therapy
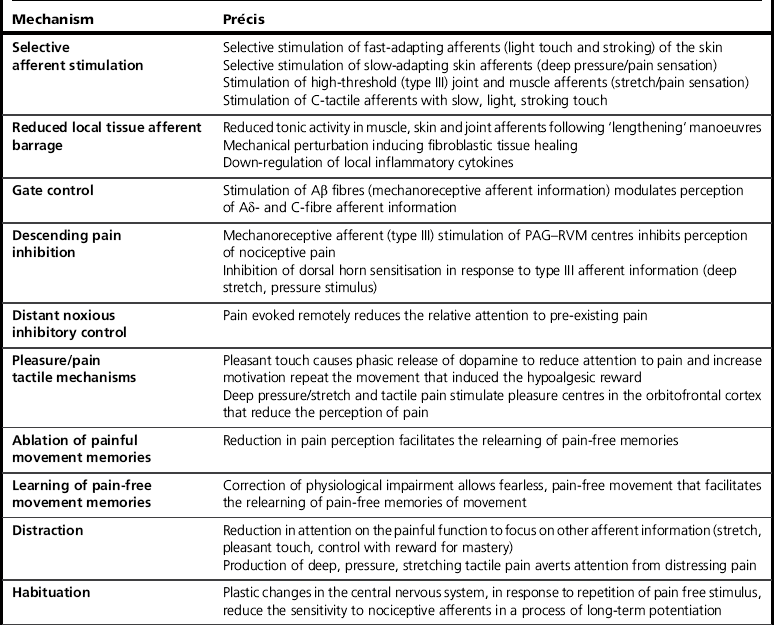
PAG, periaqueductal grey, RVM, rostral ventromedial medulla.
The somatosensory system
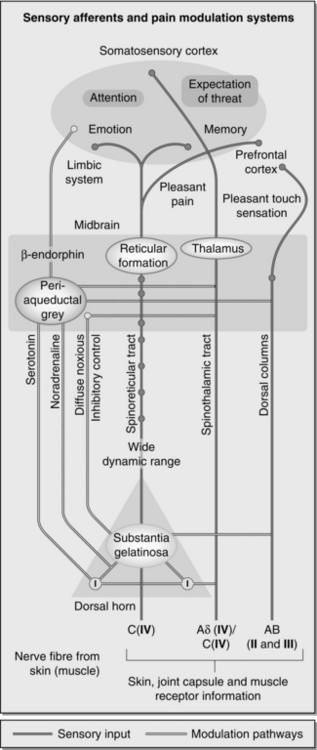
The skin, joints and muscles are supplied with receptors to allow the interpretation of movement and nociceptive stimuli (Fig. 12.2). Skin mechanoreceptors can be categorized based on the type of stimulation to which the receptor responds, the speed with which they adapt to stimulus and the size of their field of reception (Box 12.1). The neuroanatomy of our skin, the first contact receptor for tactile stimulus, allows clear distinction between deep and superficial stimuli.
Joints and ligaments also have mechanoreceptors (Table 12.2). Type I receptors, found infrequently in ligaments, are slowly adapting receptors with a low threshold and continuous firing, even at rest. Type II receptors are dynamic with rapid adaptation and a low threshold to stimulus, thus they convey information at the beginning of joint motion. Type III receptors are also dynamic-type receptors with a high threshold and slow adaptation providing sensation at the extremes of movement. These fibres can also transmit some nociceptive stimuli at extremes of deformation (Wyke 1972). Type IV receptors are free nerve endings in the tissues and are responsible for the majority of nociceptive sensation (Michelson & Hutchins 1995). Thus, placing a joint towards the end of range of motion to conduct MT influences specific skin, joint capsule and ligament receptors that are not activated in a neutral (loose-packed) position.
Table 12.2
Mechanoreceptors in joint capsules and ligaments (Wyke 1972)
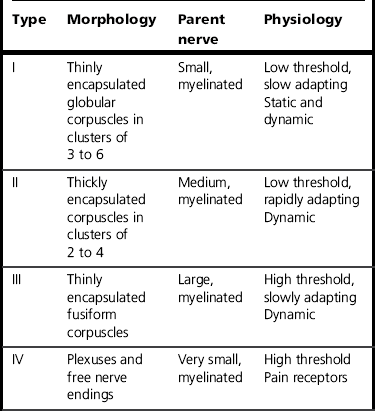
Reprinted from Wyke, B., 1972, Articular neurology, Physiotherapy, 58(3); 94–99, with permission from Elsevier.
Muscles are richly innervated with mechanoreceptors, classified as above (Mense 2003). Muscle spindles (Type Ia and II) are extremely sensitive to length changes in the muscle and have an efferent innervations (gamma motor neurons) in order to dynamically respond to changes in muscle length. In contrast, Golgi tendon organs are high threshold and insensitive to small muscle length changes but do respond to forceful muscle contraction and extreme stretch stimulation (Mense 2003). In a gross simplification of a very intricate process, mechanoreceptors join with nociceptors in an afferent system, transmitting information to the cerebral cortex.
Aβ afferents transmitting mechanoreceptive information terminate mainly in laminae III to V, which is projected to the primary (S1) and secondary somatosensory (S2) cortex via the dorsal-medial lemniscal pathway. In addition, pleasant touch (slow, light stroking of the skin, distinct to discriminatory touch) is transmitted in unmyelinated, slow C fibres known as C tactile afferents (Liu et al 2007). This afferent information projects to the limbic system. While this information does not provide discriminative information, it does facilitate the evaluation of the emotional attachment to touch (Andrew 2010). This ‘valuation’ of tactile afferent information occurs predominantly in the orbitofrontal cortex, an area that processes sexual and affective components of pain/pleasure sensations (Leknes & Tracey 2008). Finally, excessive mechanical as well as chemical and thermal stimuli activate nociceptive C and Aδ fibres (for their neuroanatomy and function refer to Chapters 5 and 6).
The gate control theory
The gate control theory (Melzack & Wall 1965) proposed that the information transmitted in the larger and faster Aβ afferents can reduce the passage of nociceptive information conveyed by Aδ and C fibres at the level of the dorsal horn. This mechanism was found to be mediated by inhibitory interneurons, which synapse with primary afferents and second-order wide dynamic range (WDR) neurons within the cord. They can exert a suppressing influence on the firing thresholds of post-synaptic second-order cells (Giordano 2005).
It must be noted that a significant proportion of small-diameter afferents can be excited with stimulation of Aβ receptors (Schweinhardt et al 2006), particularly in the presence of substance P and other sensitizing chemicals. For mechanisms leading to nociceptive contribution of non-noxious stimuli, refer to Chapter 6. In these circumstances, movement within the normal range of a joint or muscle can stimulate sensitized (previously silent) small-diameter joint nociceptors (Type IV) simultaneously to the higher threshold fibres (Type III) (Wright et al 2002). Thus, the gate control theory is able to explain some of the immediate pain-relieving effects from mechanoreceptor stimulation, but it does not fully cover the pain modulation that is commonly observed as an effect of MT. This is because MT does something much deeper than that.
Hypoalgesia mediated by the central inhibition
Over the last 20 years there has been significant investigation of the effects of MT-induced mechanoreceptive afferent barrage on the perception of nociceptive pain (Schmid et al 2008). A number of authors have demonstrated MT-induced hypoalgesia concurrent to up-regulation of noradrenergic fight or flight system responses. For example, Vicenzino et al (1998) demonstrated the excitatory effects of cervical mobilization techniques on sympathetic function (respiratory and heart rate). There has been a strong assertion that descending pain mechanisms associated with the noradrenergic/serotinergic systems result in immediate followed by longer lasting reduction in pain perception (Schmid et al 2008, Sterling et al 2001, Vicenzino et al 1998, Wright 1999).
With regard to MT-induced hypoalgesia, the periaqueductal grey (PAG) and rostroventromedial medullary (RVM) centres of the brain stem are likely to be important components of the descending pain inhibition systems (Close et al 2009, Schmid et al 2008, Sterling et al 2001, Vicenzino et al 1998, Wright 1999; see Chapter 6). There are distinct areas within the PAG that mediate transmission of nociceptive information. Afferent stimulation of the dorsal PAG elicits a fight or flight reaction, with sympatho-excitation leading to a modulation of pain that is effectively instantaneous (Wright 1995). The dorsal PAG mediates a noradrenergic mechanism, which specifically influences cortical perception of nociceptive pain and induces an inhibition of substance P release from the terminals of nociceptive fibres at the peripheral source of pain (Pertovaara 2006). The ventral PAG facilitates recuperative behaviour through an opioid/serotinergic-mediated pathway. Typically this response is observed 20–45 minutes post MT treatment (Close et al 2009, Schmid et al 2008, Sterling et al 2001, Vicenzino et al 1998, Wright 1999).
These systems have been shown to be bidirectional and thus are able to inhibit or facilitate nociception, in response to the importance of the stimuli via ON and OFF cells within the RVM (Close et al 2009, Heinricher et al 2009). For example, nocioceptive thresholds can be raised (reducing perception of pain) during feeding and micturition (via OFF cell activation) and lowered in the presence of acute inflammation (via ON cell activation) as attention is focused toward the most functionally important stimulus. The response of both OFF and ON cells, and therefore descending mediation, can be diminished in the presence of chronically painful, inflammatory conditions (Pinto-Ribeiro et al 2008).
Numerous investigators have demonstrated that high-threshold mechanoreceptive afferent barrage, be it from the spine (Bretischwerdt et al 2010, George et al 2006, Ruiz-Saez et al 2007), peripheral joints (Slater et al 2006, Vicenzino et al 2001), muscles (Bretischwerdt et al 2010) or nerves (Beneciuk et al 2009), can result in clinically meaningful reductions in nociception (Schmid et al 2008). This reduction in pain perception has been measured both locally to the site of MT and in sites distant to the areas receiving MT (Bretischwerdt et al 2010, Cleland et al 2005).
Recent work has suggested a more selective response to MT in terms of its extent of effect and its mediation of particular nociceptive afferent information (Beneciuk et al 2009, George et al 2006, Willett et al 2010). A study undertaken by George et al (2006)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree