Fig. 3.1
Sinus arrest
3.4 Atrioventricular Block
Atrioventricular block occurs when the conduction of the atrial impulse to the ventricles slows down or is blocked (paroxysmal or permanently), even though the AV junction is not physiologically refractory.
In the presence of a high atrial rate (e.g., atrial tachycardia or AF), the term AV block is correct only if the ventricular rate is lower than 60 bpm.
There are three anatomical sites of block: (1) above Hisian (inside the AV node), (2) intra-Hisian (inside the His bundle), and (3) infra-Hisian (distal His bundle or bundle branches).
The identification of anatomical site is relevant, as the distal blocks are those with the worst prognosis.
3.4.1 First-Degree AV Block
Every single atrial impulse is followed by a QRS complex, but the PR interval is greater than 200 ms. The block is usually above the AV node, even if there may be a wide QRS complex caused by a coexisting bundle-branch block. In general it is not associated with heart disease, and is usually secondary to increased vagal tone or is drug related (β-blocker or digoxin), although sometimes it can be associated with myocardial ischemia, infiltrative myocardiopathies, myocarditis, Addison disease, or congenital heart disease (septal defect, Ebstein). Prognosis, however, is benign, and no treatment is required. An exception can be the occurrence of a first-degree AV block in aortic valve endocarditis resulting from an abscess of the interventricular septum.
3.4.2 Second-Degree AV Block
Conduction from the atria to the ventricles is intermittent. There are two types of second-degree AV block.
Type I, also known as Mobitz I or Luciani-Wenckebach, involves progressive increase of the PR interval and consequent shortening of the RR interval until a nonconducted P wave develops. The morphology of the QRS complex is normal. The site of the block is usually at or above the AV node [15]. Etiology mainly includes digoxin intoxication, myocardial ischemia (inferior myocardial infarction), excess calcium deposits such as occur in aortic stenosis, or renal insufficiency. It can be also observed in both trained athletes and normal persons during sleep, attributable to increased vagal tone [16–18]. Prognosis is excellent if asymptomatic, while the onset of symptoms such as syncope or heart failure may require the placement of a definitive pacemaker.
Type II (Mobitz II) shows a sudden block of a P wave with a ratio of 3:2, 4:3, and so forth. PP and RR intervals are regular (Fig. 3.2). The block is intra- or infra-Hisian, and tends to progress toward complete AV block with prolonged ventricular pause and syncope [19]. Guidelines favor permanent pacing even in asymptomatic patients with type II block [20].
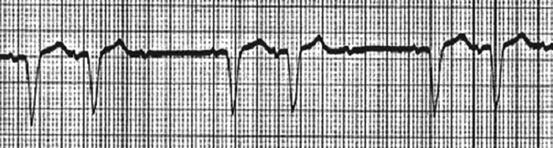
Fig. 3.2
II degree–Mobitz 2 AV block (with intraventricular delay)
3.4.3 Atrioventricular Block with 2:1 Conduction
This condition is characterized by an intermittent block with a P/QRS ratio of 2:1, thus having features of both Mobitz I and II. Block can be at any nodal site and intra- or infra-Hisian, the severity depending on the resultant ventricular rate. In an asymptomatic patient a 2:1 block with a coexisting bundle-branch block is an indication for pacing, assuming that the block is infranodal [21].
3.4.4 Advanced AV Block
In advanced AV block, two or more consecutive P waves are blocked with a P/QRS ratio of 3:1, 4:1, and so forth (Fig. 3.3). In everyday practice this term is also used for low-rate permanent AF.
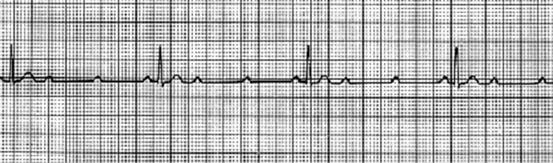
Fig. 3.3
Advanced (3:1) tipo II AV block
3.4.5 Low-Rate Atrial Fibrillation
The absence of recognizable P wave, irregular RR intervals, and narrow or wide QRS complexes characterizes low-rate AF. Causes are usually drugs (antiarrhythmic, digoxin, β-blockers, Ca2+ antagonists), especially in elderly patients with impaired renal and/or liver function, vagal hypertone (young subjects), or impaired AV conduction.
Treatment consists in ensuring hemodynamic normality using drugs (atropine followed by amines) or transcutaneous or transvenous pacing in symptomatic bradycardia.
3.4.6 Third-Degree AV Block
The inability of P waves to conduct to the ventricles (complete block of AV conduction) characterizes third-degree AV block. There is no relationship between P waves and QRS complexes, which are escape beats. Narrow QRS escape rhythms, with regular RR and a frequency between 40 and 60 bpm, are secondary to blocks within the AV node. Wide QRS escape rhythms with frequency between 40 and 20 bpm are secondary to infra-Hisian blocks.
In patients with AF and complete AV block a regular ventricular rate is observed, because of junctional (usually at about 35 bpm) or infra-Hisian escape rhythm.
Third-degree AV block can be secondary to pharmacologic treatments (digoxin, β-blockers, Ca2+ antagonists, quinidine, procainamide) or sclerodegenerative phenomena of conduction fibers, or may occur during the acute phase of myocardial infarction. Prognosis is more favorable if associated with inferior myocardial infarction (supra-Hisian block, narrow QRS escape rhythm, and generally spontaneous resolution), while the prognosis is worse in anterior myocardial infarction (infra-Hisian block and wide QRS escape rhythm, generally associated with a wider area and less reversibility of ischemic injury).
Less common causes include infectious diseases (myocarditis, Lyme disease, Chagas disease), rheumatic etiology (Reiter syndrome, scleroderma, rheumatoid arthritis), infiltrative disease (amyloidosis, sarcoidosis, multiple myeloma), electrolyte disorders, and iatrogenic factors (cardiac surgery, radiofrequency ablation) (Fig. 3.4).
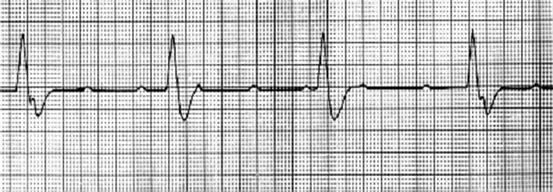
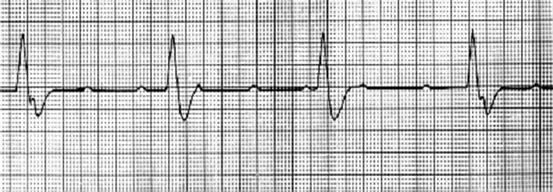
Fig. 3.4
III degree AV block with wide QRS (infra-hisian) escape
3.4.7 Interventricular Block
Left bundle-branch block (LBBB) is a rare finding in the young population, and when present should raise the suspicion of an underlying heart disease. Incidence increases with age [22] and is associated with various causes of heart disease (hypertensive, ischemic, valvular, idiopathic dilated cardiomyopathy). Prognosis depends on the severity of the underlying disease.
Left anterior hemi-block (LAHB), more frequent in the adult male population, is associated with hypertension and ischemic heart disease. Progression to LBBB or complete AV block is uncommon [23].
Left posterior hemi-block (LPHB) is a rare isolated finding because of both the short course and double vascularization of the left posterior fascicle.
Right bundle-branch block (RBBB) as an incidental ECG finding is not often linked to heart disease, but may be associated with systemic hypertension, pulmonary heart disease, or ischemic heart disease.
Bifascicular block commonly indicates the association of an interruption or delay in impulse conduction along both sets of left bundle branch, or along the right branch and one of the two sets of left bundle branch.
RBBB + LAHB, a more common condition, shows a progression to complete AV block in less than 6 % of patients, while RBBB + LPHB, less frequent, has a greater progression toward complete AV block (close to 75 %).
Patients with bifascicular block associated with first-degree AV block (especially infranodal, when the HV interval, documented during invasive electrophysiological evaluation, is >100 ms) have a higher risk for developing complete AV block, and some authors recommend permanent cardiac stimulation [24]. The diagnosis of trifascicular block can be made on surface ECG only in the presence of alternating bundle-branch block (LBBB alternating with RBBB, or RBBB + LAHB alternating with RBBB + LPHB).
3.4.8 Atrioventricular Dissociation
AV dissociation is present when atrial activity is independent from ventricular activity, both occurring at regular rates. AV dissociation is not synonymous with AV block; in fact while patients with AV block also have an AV dissociation, patients with AV dissociation may not have an AV block, for example when an escape junctional (or ventricular) rate is higher than the sinus rate in the absence of retrograde ventricular-atrial conduction.
Elderly patients with degenerative cardiac disease are more likely to have AV dissociation [25].
Treatment depends on the causes, and ranges from antiarrhythmic drug treatment to permanent pacemaker placement.
3.4.9 Conduction Disturbances during Acute Myocardial Infarction
Sinus node dysfunction in the course of myocardial infarction may be secondary to the occlusion of the circumflex artery or the right coronary artery. The bradycardia that follows may favor escape rhythms with narrow QRS, which originate at the junction or in the His bundle and have a heart rate of about 50–60 bpm becoming stable over time, whereas escape rhythms with wide QRS originate from the Purkinje fibers with a heart rate below 40 bpm, are less stable, and may evolve to asystole. The AV block that occurs in the early stages of myocardial infarction is generally secondary to hypervagotonia and is reversible with atropine, while blocks occurring later are frequently related to ischemia of the AV node.
Second-degree type I AV block during inferior myocardial infarction tends to resolve spontaneously within 48 h and does not require invasive treatment unless there is hemodynamic compromise.
Second-degree type II AV block is more likely to progress to complete AV block, and occurs more frequently in anterior myocardial infarction, although it can also occur in inferior myocardial infarction because of occlusion of a large posterior descending artery.
Complete AV block, which is present in 8–13 % of patients with myocardial infarction, occurs in both inferior and anterior myocardial infarction, and can be preceded by fascicular blocks or bundle-branch block with second-degree AV block. It is associated with a higher incidence of ventricular fibrillation/tachycardia, pulmonary edema, and in-hospital mortality [26].
3.4.10 Cardiac Arrest and Sudden Cardiac Death
The incidence of sudden cardiac death (occuring within 1 h from the onset of cardiac symptoms) is variable, depending on the varying prevalence of coronary disease in different countries [27]. In the USA there are 300,000 cardiac deaths annually, with a total annual incidence of 1 in 1,000 individuals [28].
Ventricular fibrillation is the first rhythm detected in 75–80 % of cases, while in the remaining 20–25 % extreme bradycardia or pulseless electrical activity are causes of cardiac arrest.
Bradyarrhythmic cardiac arrest is secondary to the inability of cardiac automatism to emerge and replace the sinus node or normal function of the AV junction.
Cardiac arrest is more common in advanced cardiac disease, generally as a consequence of extracellular potassium accumulation (secondary to hypoxemia, acidosis, shock, or renal insufficiency), which reduces myocellular automatism.
Pulseless electrical activity is an electrical stable cardiac rhythm in the absence of any effective myocardial contraction. The primary form is generally the terminal event of a severe cardiopathy or expression of acute myocardial ischemia, and the secondary form is a severe expression of a sudden failure in venous return, such as in pulmonary embolism, cardiac tamponade, or acute cardiac prosthetic valve dysfunction.
Reversible causes such as hypovolemia, hypoxia, cardiac tamponade, pneumothorax, acidosis, and hyperkalemia must be detected and corrected. Pharmacological support involves the use of intravenous epinephrine or atropine (the latter, however, is not effective in infra-Hisian AV block).
External cardiac pacing can be useful, although “asystolic” patients still have a poorer prognosis, regardless of the effectiveness of the stimulation [29].
3.5 Treatment
Sinus node dysfunction generally does not require treatment if asymptomatic. When needed, parasympatholytic drugs (atropine 0.5 mg intravenously, repeatable) can acutely increase the automaticity of the sinus node and improve sinus atrial conduction. Sympathomimetic drugs (theophylline per os) are less frequently used for long-term treatment because of their low efficacy and frequent side effects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







