Fig. 64.1
Non-contrast head CT at initial presentation. There was no evidence of cerebral edema despite markedly impaired mental status
Broad-spectrum antibiotics consisting of vancomycin and cefepime were started given her leukocytosis and concern for possible aspiration pneumonia. Sputum culture grew pan-sensitive Streptococcus pneumonia and her antibiotic regimen was narrowed to cefepime at ICU day #2. Her initial Factor V level was undetectable (i.e. <5 %), but lactate level improved to 5.1 mmol/l. After initial improvement with aggressive fluid resuscitation, her creatinine rose to 1.86 mg/dl by 48 h. IV vitamin K was given with initial improvement in her INR to 1.2, but this began to rise again to 2.5 by ICU day #2. Approximately 48 h into her hospitalization, her neurologic exam worsened, and she was unable to follow commands. A repeat non-contrast head CT showed evidence of cerebral edema (Fig. 64.2).
Fig. 64.2
Non-contrast head CT at hospital day 2. The scan demonstrates evidence of diffuse cerebral edema with loss of the grey-white juncture and reduced sulcal folds throughout
Question
What intervention is now recommended?
Answer
Intracranial pressure monitoring for cerebral edema.
After infusion of 3 units of FFP and 5000 Units of recombinant FVIIa, a codman ICP monitor (DePuy Synthes, Raynham, MA) was placed by neurosurgery, which showed an initial ICP of 35 mmHg. Resumption of the propofol infusion improved the ICP to 6–15 (goal <20). In addition, target levels of serum sodium (>150 mg/dl), osmolality (>120 mOsm/l), and a pCO2 (25–30 mmHg) were met without additional treatment. Due to the history of recurrent illicit drug abuse and severe psychiatric disease, she was not felt to be a liver transplant candidate.
On hospital day 3, her ICP monitor registered an acute increase from <20 to 45 mmHg. Intravenous mannitol 60 g and hypertonic saline were initiated, despite serum sodium level of 151 and osmolarity of 336, respectively. Sedation was also increased with propofol. She then developed seizure-like activity with rhythmic twitching of her jaw and a pentobarbitol bolus with subsequent continuous infusion was given. Approximately 5 h later, her ICP dropped precipitously to 4 mmHg with a neurologic exam showing fixed, dilated pupils bilaterally. A repeat head CT showed worsening cerebral edema with blurring of the grey- white interface and early left uncal herniation. An EEG showed no seizure activity.
Due to the concern of possible brain herniation, her sedation was held. After 6 h of completely absent corneal, gag/cough reflex and with persistently fixed and dilated pupils, neurology assessed the patient as having a grim prognosis with high risk of brain death. A Technetium sulfur-colloid scan was proposed to confirm the absence of intracranial blood flow but due to her persistently poor hepatic function with an ALT of 2978 IU/l, INR 4.4 and concomitant multi-organ failure, her family elected to withdraw care and she passed away after extubation.
Acute liver failure (ALF) is defined as the sudden onset of severe liver injury resulting in coagulopathy (i.e. INR >1.5) and encephalopathy, in a patient with no prior history of liver disease. Most studies define ALF as injury onset in the past 26 weeks, but the majority of patients present with non-specific symptoms of malaise, lethargy, and nausea/vomiting for <8 weeks [1, 2]. APAP overdose is the most common cause of ALF in western countries accounting for nearly 50 % of consecutive adult cases (Fig. 64.3). Although the majority of the 60,000 annual APAP overdoses in the US are intentional and recover with supportive care, non-intentional APAP overdoses account for nearly 50 % of the >500 patients who progress to ALF each year [3]. Most non-intentional APAP overdose cases result from the ingestion of excessive quantities of over-the-counter products that contain APAP and/or prescription narcotic-APAP analgesic congeners taken over several days for various ailments. The frequency of alcohol abuse and psychiatric co-morbidity is similar in the intentional versus non-intentional APAP patients [3]. Although non-intentional overdose patients have more advanced encephalopathy at presentation, they have a similar rate of 3-week spontaneous survival as the intentional overdose patients (70 %).
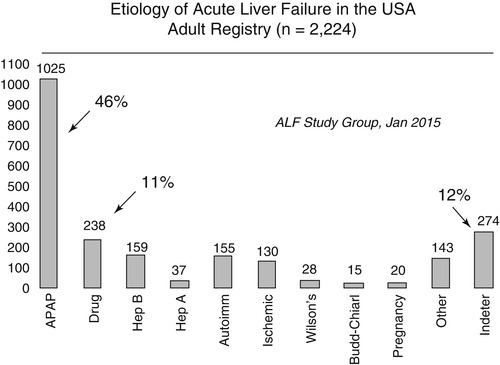
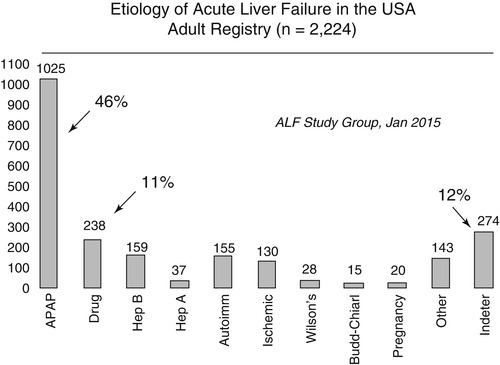
Fig. 64.3
Etiology of ALF in adults enrolled in the ALFSG from 1998 to 2014 (Figure courtesy of William M. Lee, MD and the Acute Liver Failure Study Group)
Principles of Management
Etiology of ALF
Due to the inability to reliably obtain a medication and medical history, all adults with ALF should have a serum APAP level checked. In addition, any suspicion of APAP-induced liver injury should lead to immediate treatment with n-acetylcysteine (NAC) (Table 64.1 Treatment of APAP-induced ALF) [4]. The Rumack-Matthew nomogram is helpful in determining the likelihood of APAP hepatotoxicity developing in patients with a single time point APAP overdose and should also be repeated 4 h after initial presentation. However, the nomogram should not be used to guide NAC treatment decisions in patients who inadvertently ingest excessive quantities of APAP over several days and have low or undetectable serum APAP levels at presentation. Patients with APAP overdose may initially have normal serum aminotransferase levels or only evidence of an isolated INR elevation or metabolic acidosis. However, the majority of patients with hepatotoxicity develop a serum ALT >1000 within 24 h of hospitalization and most of them have normal or only minimally elevated total bilirubin levels. The possibility of acute viral hepatitis (hepatitis A, B, C, and cytomegalovirus (CMV), Epstein-Barr virus (EBV), and herpes simplex virus (HSV)) should be excluded early on as well as potential hepatic ischemia due to underlying cardiopulmonary disease or volume depletion. A thorough diagnostic workup is recommended to identify treatable causes of ALF such as autoimmune hepatitis, Wilson’s disease, or acute HBV infection (Table 64.2).
Table 64.1
Recommended treatment of acetaminophen overdose
Oral treatments |
Within 4 h of APAP ingestion Ipecac syrup, 15 ml once; repeat in 20 min if needed to induce emesis Nasogastric lavage of pill fragments Activated charcoal, 1 g/kg body weight (max dose 50 g) Should be given before oral NAC |
Within 24 h of APAP ingestion and ability to tolerate oral intake Oral NAC to replete glutathione stores Oral NAC dosing: 140 mg/kg load followed by 70 mg/kg every 4 h for 17 doses or until INR <1.5a Give ondansetron/prochlorperazine or mix with carbonated beverage to improve GI tolerability |
Intravenous N-acetylcysteine infusion |
Indications: Subjects with severe nausea/vomiting unable to tolerate oral NAC, short-gut, known ileus, and pregnant women Dose 1. Loading Dose: 150 mg/kg NAC in 200 ml D5W over 1 h Dose 2. 50 mg/kg NAC in 500 ml D5W over 4 h Dose 3. 125 mg/kg NAC in 1000 ml D5W over 19 h Dose 4. 150 mg/kg NAC in 1000 ml D5W over 24 h Dose 5. 150 mg/kg NAC in 1000 ml D5W over 24 h |
Cautions 1. Contraindications: sulfa allergy 2. If Acetadote (Cumberland Pharmaceuticals, Nashville, TN) is unavailable, standard oral NAC can be mixed for IV administration using a leukopore filter. (Consultation with local ICU pharmacy) 3. Telemetry monitoring recommended for arrhthymias and adverse effects 4. Potentially severe anaphylactoid and hypersensitivity reactions reported in up to 3 % of treated patients Bronchospasm, nausea, rash, and pruritis have been reported If reaction occurs, hold infusion, administer IV fluids, IV diphenydramine, and corticosteroids as needed Consider restarting infusion at 50 % rate if reaction abates and not severe |
Table 64.2
Recommended diagnostic evaluation for adults with ALF
Etiology | Diagnostic testing | Treatment |
|---|---|---|
Acetaminophen | Acetaminophen level Urine tox screen | N-acetylcysteine |
Acute viral hepatitis | anti-HAV IgM, HBsAg, anti-HBc IgM, anti-HCV, HCV RNA, HSV-DNA (PCR)a, CMV-DNA (PCR)a, EBV-DNA (PCR) or serologiesb | Entecavir for HBV Acyclovir for HSV |
Wilson’s disease | Ceruloplasmin, 24-h urine copper, slit-lamp examc | Chelation therapy |
Autoimmune hepatitis | Anti-nuclear antibody (ANA), anti-smooth muscle antibody (ASMA), Immunoglobulin levels, liver biopsy | Corticosteroids |
Ischemia | Transthoracic echocardiograma | Fluids/pressors |
Budd-Chiari | Liver ultrasound with Doppler | Anticoagulation |
Pregnancy-related Toxemia HELLP Acute fatty liver of pregnancy | Serum pregnancy testing | Urgent delivery |
Idiosyncratic DILI | Medical history and drug exposure | Drug cessation Consider N-acetylcysteine |
The etiology of ALF is closely linked with the likelihood of hepatic recovery and spontaneous survival. For example, subjects with APAP overdose, hepatitis A, hepatic ischemia, and pregnancy related ALF generally have a favorable prognosis for spontaneous recovery (50–70 %) while subjects with idiosyncratic drug-induced liver injury (DILI), autoimmune hepatitis, and indeterminate ALF only have a 20–50 % likelihood of spontaneous recovery [1,5]. The modified King’s College Criteria (Table 64.3) are frequently used to help guide treatment and management decisions in both APAP and non-APAP related ALF patients [7].
Table 64.3
King’s college criteria for adverse outcomes in ALF
Acetaminophen overdose | Non-acetaminophen ALF |
|---|---|
Arterial lactate >3.5 mmol/l 4 h after resuscitation OR pH <7.30 or arterial lactate >3.0 mmol/l 12 h after resuscitation OR INR >6.5 (PT >100 s) Serum creatinine >3.4 mg/dL Stage 3 or 4 encephalopathy | INR >6.5 (PT >100 s) OR any three of the following INR >3.5 (PT > 50 s) Age <10 or >40 years Serum bilirubin >17.5 mg/dL Duration of jaundice >7 days Etiology: drug reaction |
Correction of Coagulopathy
ALF is frequently associated with thrombocytopenia as well as marked derangements in various clotting factor levels leading to an elevated INR, low Factor V levels (<50 %), and evidence of disseminated intravascular coagulation. Serial measurement of INR and Factor V levels can provide important prognostic information at the bedside regarding the recovery of hepatic function. However, clinically significant spontaneous bleeding is observed in <10 % of patients presumably due to reduced synthesis of clotting inhibitors as well [8]. Therefore, blood products, such as fresh frozen plasma (FFP), platelets, and cryoprecipitate should not routinely be given, unless invasive procedures are planned or there is active bleeding. However, parenteral vitamin K (10 mg SQ or IV for 3 days) is recommended for all ALF patients.
Hemodynamic Support
ALF patients frequently require fluid challenges as well as vasopressor support during their ICU course to support adequate tissue perfusion. Resuscitation with normal saline is an appropriate first-line response to hypotension in ALF patients, but the potential for exacerbation of cerebral and pulmonary edema particularly in patients with AKI must be considered. While IV albumin is useful in the management of cirrhotics with spontaneous bacterial peritonitis, large-volume paracentesis, and hepatorenal syndrome, there is little evidence to guide its use in ALF patients. In volume-refractory hypotension, norepinephrine or dopamine should be used to maintain an adequate MAP (i.e.≥60 mmHg), though there is little data to recommend a specific agent [5]. Norepinephrine can provide blood pressure support while minimizing tachycardia and preserving hepatic blood flow [5]. Vasopressin can also be used, though caution is needed in patients with an elevated ICP [9]. In patients with hypotension that is refractory to fluids and vasopressor support, hydrocortisone treatment for adrenal insufficiency may be of value. Studies have shown that patients with ALF can have adrenal insufficiency, with both low baseline cortisol levels as well as failure to respond appropriately to cosyntropin stimulation testing [10]. Patients who fail to respond to stimulation testing have a greater likelihood of hemodynamic instability requiring vasopressor support [10]. However, corticosteroids are not routinely recommended for ALF patients due to the lack of improved outcomes and potential for increased infections [5,11].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







