Fig. 54.1
Multiple peribronchovascular opacities with spiculated consolidative peripheral opacity in left upper lobe
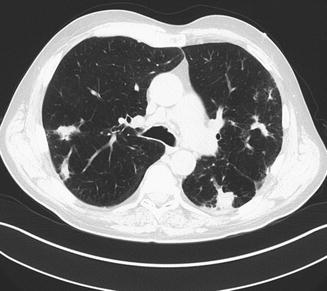
Fig. 54.2
Patchy peribronchovascular opacities present in both lungs

Fig. 54.3
Cavitary foci within the consolidative opacity. Moderate centrilobular and panlobular emphysema with a 5.8 cm bulla in right middle lobe
Question
What are the differential diagnoses, diagnostic approach and treatment of this patient’s symptoms and progressive radiographic changes?
Answer
The differential diagnosis of this patient’s progressive pulmonary infiltrates is broad and includes both infectious and non-infectious etiologies.
Non-infectious etiologies include bronchiolitis obliterans with organizing pneumonia (BOOP), malignancy (although the time course is somewhat rapid), drug-induced lung disease, alveolar hemorrhage, atypical cardiogenic edema and recurrent aspiration bronchiolitis and pneumonitis. Notable, however, is the absence of historical or clinical features suggestive of these entities. Also noteworthy is his combined duration of moderate to high dose corticosteroid therapy.
Infectious differential diagnoses include recurrent bacterial pneumonia potentially in the setting of noted bronchiectasis. Infectious aspiration bronchiolitis and pneumonitis, and viral infection would be less likely. Fungal pathogens include Pneumocystis jirovecii and other fungal organisms. He had no recent history of travel to endemic areas of fungal infections.
Due to the severity of his underlying lung disease/emphysema, degree of hypoxemia as well as the aforementioned diagnostic considerations, and the potential low yield for bronchoscopy and associated risk for hypoxia with transbronchial biopsy, the patient was referred for video-assisted thoracoscopic biopsy (VATS). The patient underwent a left sided VATS with specimens obtained from the left upper lobe, lingua and lower lobe segments.
The pathology was notable for readily identified fungal organism with acute angle branching, septated hyphae morphologically consistent with Aspergillus, marked acute and chronic intraalveolar hemorrhage, associated bronchiolitis obliterans-organizing pneumonia, necrotizing granulomas centered along bronchovascular structures suggestive of invasive pulmonary aspergillosis (IPA), angioinvasive aspergillosis, and a component of chronic pulmonary necrotizing aspergillosis.
Principles of Management
Diagnostic Approach
Aspergillus is a fungus that is ubiquitous in nature and inhalation of spores are common. In healthy hosts, spores are eliminated by immune defenses and mucociliary clearance mechanisms of the lung. Germination is the conversion of spores to hypal elements, which branch at a 45-degree angle. There are over 200 species of Aspergillus; however, the most common species that cause illness in descending order are A. fumigatus, A. flavus, A. niger and A. terreus [1, 2]. Aspergillus infection is primarily the result of impaired airway clearance from a compromised immune system or chronic lung disease. Aspergillosis illness can be due to allergy, (Allergic Bronchopulmonary Aspergillosis), airway or lung invasion (Aspergillus Tracheobronchitis or Invasive Pulmonary Aspergillosis (IPA or Chronic Pulmonary Aspergillosis), a cutaneous infection or extra-pulmonary dissemination, including CNS involvement [3].
The diagnosis of IPA can be challenging, as patients may initially be asymptomatic. Criteria for the diagnosis of invasive fungal disease were initially formulated in 2002 and updated in 2008 [4]. Definitions for proven, probable and possible IPA for the susceptible populations have been stated. The population at risk can be broken down into classic risk factors and newer identified risk factors [5–8].
Risk Factors for Invasive Aspergillosis
Classic Risk Factors
Severe and prolonged neutropenia
Allogeneic stem cell transplant recipients
Severe Graft Versus Host Disease
Systemic corticosteroid use for greater than 3 weeks
Conditions or drugs that cause chronic impaired cellular immune response such as patients with autoimmune disease, anti-rejection medication
Newer Risk Factors
Critical illness
Solid organ transplant recipients
Chronic Obstructive Pulmonary Disease, including patients on inhaled corticosteroids
End stage Liver Disease/Alcoholic Hepatitis
HIV infection
Diabetes
In a retrospective multicenter study of 1209 patients selected with culture positivity for Aspergillus, 12 % had evidence of disease [1]. Patients with hematologic malignancy or transplants accounted for the majority of cases; malnutrition (27 %), corticosteroid use (20 %), HIV infection (19 %), diabetes mellitus (11 %) and chronic obstructive pulmonary disease (9 %) were associated with evidence of invasive infection. In a single-center retrospective study of 239 patients hospitalized with COPD who had Aspergillus isolated from the lower respiratory tract, 22 % had probable invasive aspergillosis [7]. Inhaled corticosteroids may increase the risk of invasive aspergillosis in patients with COPD [9, 10].
Clinical presentation of IPA can be nonspecific, with patients developing fever, chest pain, dyspnea, cough and/or hemoptysis. A classic triad described in patients with neutropenia is fever, pleuritic chest pain and hemoptysis [11]. Absence of the triad should not exclude patients from the possibility of IPA in patients with risk factors for the disease.
Chest CT radiograph is more sensitive than plain chest radiographic imaging. HRCT is recommended in all cases of suspected IPA [4, 12]. Findings on HRCT indicative of invasive pulmonary disease include macronodules with or without a surrounding “halo” of ground glass changes, air-crescent sign, cavitary lesions, and areas of consolidation. A retrospective study of chest imaging in 235 patients with invasive aspergillosis demonstrated one or more macronodules (94 %), halo sign (61 %), consolidation (30 %), infarct shaped nodules (27 %), cavitary lesions (20 %) and air-crescent signs (10 %) [13].
Diagnosis is based on both isolating the organism or markers of the organism and the probability that it the cause of the disease.
Culture of the organism in combination with evidence of tissue invasion on histopathology or culture from a normally sterile site provides the most certain evidence of IPA. Tissue biopsy with histopathologic demonstration of tissue invasion by fungal hyphae is considered the “gold standard” [14].
Laboratory testing that can aid in the diagnosis of invasive infection includes enzyme immunoassays that detect galactomannan, a polysaccharide in the Aspergillus cell wall in serum or bronchoalveolar fluid. False-positive galactomannan tests have been reported in patients receiving pipercillin/tazobactam antibiotics.
Testing serum for an additional antigen, 1, 3 Beta-D glucan, is not specific for aspergillus, since the antigen is present in other fungi [6, 12].
Investigative studies looking for DNA evidence by PCR has shown mixed results.
Bronchoscopy is routinely performed in suspected cases of IPA. However, bronchoscopy has several limitations, including sampling error due to patchy involvement in the lung, and the potential risk in this patient population that may be coagulopathic or thrombocytopenic.
Therapy
The Infectious Diseases Society of America (ISDA) released guidelines for the treatment of invasive aspergillus in 2008 and The American Thoracic Society (ATS) published guidelines in 2011 for the treatment of fungal infections [4, 15, 16]. When invasive disease is suspected or documented, early aggressive anti-fungal treatment is essential. Therapy is often prolonged from months to more than a year, with duration of therapy dependent upon the patient’s location of infection, underlying disease, and response to therapy, which includes assessment of clinical and radiographic resolution, improvement in immune function and microbiologic clearance.
Antifungal Therapy
Three classes of antifungal agents are used for the treatment of aspergillus: polyenes, azoles and echinocandins. Choice of therapy may be dependent upon the patient’s organ function, immune status and prior therapies.
Treatment can be divided into initial therapy or salvage therapy. At present, monotherapy is recommended.
Monotherapy
Triazoles
These antifungal agents include voriconazole, posaconazole, itraconazole and fluconazole.
Voriconazole has emerged as standard therapy for the treatment of invasive aspergillus. An international, multicenter randomized open-label trial involving 277 patients with confirmed or probable invasive aspergillus compared voriconazole with amphotericin B deoxycholate as initial therapy [17]. The majority of patients had hematologic malignancy and many had undergone hematopoietic stem cell transplant. At 12 weeks, 53 % of those patients treated with voriconazole compared to 32 % treated with Amphotericin B had a greater likelihood of complete or partial response, a lower mortality rate (29 % vs. 42 %), a lower rate of adverse reactions and less likelihood of requiring a change in therapy due to intolerance or poor response (36 % vs. 80 %). The efficacy of voriconazole compared with lipid formations of Amphotericin B is unknown since there are no available studies of comparison.
Voriconazole may also be used in those patients with CNS disease. Despite a mortality rate, which has previously approached 100 %, in one retrospective study, 31 % of patients who were treated with voriconazole survived for a median observation of 390 days. The vast majority of the patients had received other antifungal therapy other than voriconazole for a median of 31 days prior to changing to voriconazole [18].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







