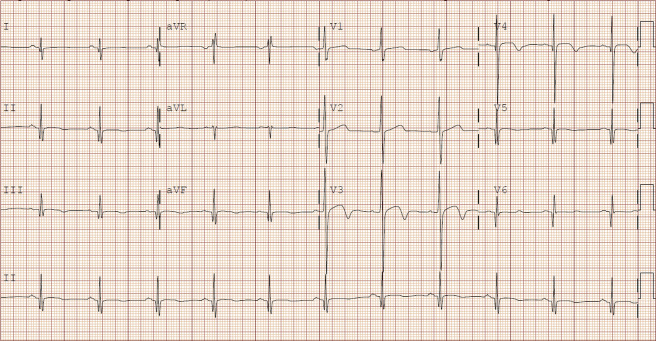
A 34-year-old man presented to the emergency department (ED) for chest pain and lightheadedness. The patient had no significant medical history, family history, or drug use. Symptoms were present at rest and with activity. Before this, he was active, biking 1 to 2 hours daily. Blood pressure was 104/62 mm Hg. An ECG was obtained at arrival to the ED ( Figure 1 ).
Interpretation
The ECG revealed a narrow complex, sinus rhythm with rate of 67 beats/min. QRS axis was normal. PR and QRS intervals were normal; the QTc was 448 ms. There was 1 mm of ST-segment elevation in anterior leads (V3 and V4). T-wave inversions were present in anterior leads (V3 to V5) and inferior leads (II, III, and aVF). Q waves were observed in inferior leads (II, III, and aVF) and lateral leads (V5, V6, and I).
Clinical Course
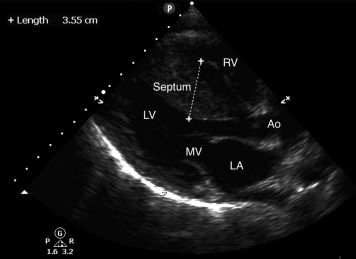
Given the history and abnormal ECG result, the differential included acute coronary syndrome and hypertrophic cardiomyopathy. Point-of-care ultrasonography was performed and showed asymmetric hypertrophy of the anterior septum ( Figure 2 ). To further evaluate for ischemia, serial ECGs were obtained that did not show dynamic changes, and serial troponin test results were negative (<0.03 ng/mL). The patient was admitted to an observation unit with telemetry monitoring for cardiology consultation and transthoracic echocardiogram with Doppler. He was found to have severe, asymmetric septal hypertrophy with associated diastolic dysfunction. There was no evidence of outflow tract obstruction or systolic anterior motion of the anterior mitral valve leaflet at rest. There were no episodes of ventricular tachycardia during his stay, and he was discharged with continued cardiology follow-up.
Hypertrophic cardiomyopathy is a genetic disease characterized by ventricular hypertrophy without a recognized precipitant cause (eg, hypertension, aortic stenosis). It is among the most common causes of sudden cardiac death in young persons. The diagnosis should be considered in young patients presenting with syncope, presyncope, chest pain, palpitations, exertional fatigue, or shortness of breath.
Almost all patients with hypertrophic cardiomyopathy will have an abnormal ECG result. However, there are many different ECG findings in hypertrophic cardiomyopathy, with no single finding being pathognomonic. Pathologic Q waves, ST-T wave changes, left ventricular hypertrophy, left atrial enlargement, and conduction disturbances may be present. Rhythm abnormalities may include premature ventricular contractions, atrial flutter, supraventricular tachycardia, sinus bradycardia, or atrioventricular blocks. Predictably, increased QRS voltage is often observed in patients with hypertrophic cardiomyopathy. However, this is rarely observed in isolation of other suggestive ECG findings.
Q waves in hypertrophic cardiomyopathy have been defined as measuring greater than or equal to 0.04 seconds or greater than or equal to 25% of the height of the ensuing R wave. Q waves are typically in the inferior or lateral leads. Lateral Q waves are thought to represent septal hypertrophy and are more specific for the diagnosis of hypertrophic cardiomyopathy. In this patient, Q waves in II, III, aVF, V5, V6, and I were narrow but met criteria based on depth greater than or equal to 25% the height of the ensuing R wave.
ST-segment elevations observed in hypertrophic cardiomyopathy may simulate those observed in acute myocardial infarction, early repolarization syndrome, left ventricular hypertrophy, pericarditis, or other conditions. In this case, given the presence of ST-elevation and T-wave inversions, acute coronary syndrome remained on the differential and prompted serial ECG and troponin tests to rule out acute myocardial infarction.
Unfortunately, ECG findings in hypertrophic cardiomyopathy do not correlate with the degree of hypertrophy or obstruction present, the risk of sudden death, or the severity of patient symptoms. Determining which patients require further diagnostic evaluation in the ED remains a complex clinical question. If the diagnosis is considered, echocardiography with Doppler can be obtained to assess the location and extent of hypertrophy, as well as the presence and severity of systolic dysfunction, diastolic dysfunction, outflow obstruction, atrial dilation, or associated valvular abnormalities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







