Chapter 92
Major Vascular Procedures 
General Approach to the Vascular Patient
Coronary Artery Disease
They do, however, significantly increase preoperative cost. In a large randomized trial evaluating coronary artery revascularization before elective major vascular surgery, no significant difference was noted in perioperative myocardial infarction or mortality between the groups who were randomized to either coronary revascularization or no revascularization prior to the vascular procedure. This suggests that the routine strategy of coronary artery revascularization before elective vascular surgery among patients with stable cardiac symptoms should not be universally recommended. The American College of Cardiology in collaboration with the American Heart Association published guidelines in 2007 that include a stepwise algorithm for determining preoperative cardiac risk based on patient and surgery risk factors undergoing noncardiac surgery (see http://circ.ahajournals.org/content/116/17/e418.full; accessed July 23, 2012).
Respiratory Dysfunction
Because vascular reconstructive procedures are frequently long, require a general anesthetic, and use abdominal or thoracic incisions, postoperative respiratory complications are common. Patients with vascular disease often have preexisting chronic obstructive pulmonary disease (COPD) from tobacco abuse, which increases the risk for postoperative complications as well. ![]()
In patients with significant pulmonary dysfunction, it may be preferable to avoid general anesthesia, if possible. Spinal or epidural anesthesia is a frequently used alternative, particularly for lower extremity revascularization procedures. Additionally, a retroperitoneal approach can be used instead of the standard transabdominal approach for some aortic procedures. The retroperitoneal incision results in less postoperative pain and pulmonary dysfunction compared with an abdominal incision. Effective postoperative pain control is essential in order to prevent postoperative pulmonary complications. Pulmonary toilet, including coughing and incentive spirometry, is critical in the postoperative period and is made possible with effective relief of incisional pain. Epidural analgesia has become the method of choice for pain control postoperatively in patients undergoing thoracic or abdominal vascular procedures (Chapter 87).
Monitoring
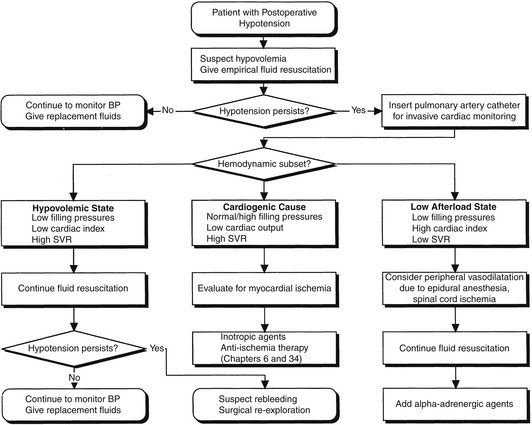
Hemoglobin, hematocrit, platelet count, and coagulation studies must also be monitored closely during the postoperative period. Blood pressure must be closely followed and tightly controlled to avoid wide fluctuations in either direction. Hemodynamic instability should be immediately assessed, and management should proceed in a stepwise and thoughtful manner ![]() (Figure 92.E1).
(Figure 92.E1).
Procedure-Specific Care: Abdominal Aortic Reconstruction 
All patients require monitoring in the ICU after open aortic reconstruction, with many patients requiring mechanical ventilation overnight. Cardiac complications are a major cause of postoperative morbidity and mortality, as previously described (see Figure 92.1). Invasive hemodynamic monitoring with a pulmonary artery catheter should be considered to direct fluid resuscitation and optimize cardiac function (Chapters 7, 8, and 11). Significant intraoperative blood loss and fluid shifts can result in hypotension in the postoperative period. Postoperative fluid requirements after aortic reconstruction may be significant because of large fluid shifts. Once the patient’s volume status has been optimized, cardiac function can be augmented with inotropic drugs if hypotension persists. Significant postoperative hypertension may result in suture line bleeding and increase myocardial oxygen consumption and therefore should also be avoided. Postoperative hypertension should be treated with short-acting vasodilators such as nitroglycerin or nicardipine for rapid titration. Occasionally, hypertension can result from postoperative pain, which, when present, should be treated accordingly (Chapter 87).
Postoperative hemorrhage is usually the result of either a technical problem or an acquired coagulopathy. Many factors contribute to postoperative coagulopathy after aortic surgery. Hypothermia, which can lead to the inactivation of clotting factors, is common with prolonged operative times and large fluid shifts. Other common causes of postoperative bleeding include decreased platelet function secondary to preoperative antiplatelet therapy, inadequate reversal of heparin with protamine sulfate, and development of a dilutional coagulopathy secondary to large intraoperative blood losses. In addition, in cases of prolonged supraceliac aortic cross clamp time, coagulation abnormalities can arise as a result of hepatic ischemia. Therefore, it is imperative to replace clotting factors and platelets as necessary and to normalize the body temperature as the first steps in the treatment of postoperative bleeding. If the patient has excessive blood loss or if the bleeding continues despite normal coagulation parameters, reoperation to look for technical causes of bleeding may be indicated.
If a patient develops paraplegia after aortic reconstruction, magnetic resonance imaging of the spinal cord should be performed immediately to rule out an epidural hematoma as a cause of the neurologic decline. If present, immediate neurosurgical consultation is required for decompressive laminectomy. If there is no epidural hematoma, efforts should be focused on therapies to maximize blood flow to the spinal cord. Augmentation of blood pressure with vasoactive agents will increase the perfusion pressure to the spinal cord. If rapid improvement is not seen, consideration should be given to placement of a lumbar drain catheter to reduce the pressure surrounding the spinal cord.