CHAPTER 43
Low Back Pain
Stephen A. Ferrara, DNP, RN, FNP-BC, FAANP
Low back pain (LBP) is one of the leading reasons for primary care visits. The prognosis of LBP varies widely in the literature. It has long been believed that 90% of cases improve with nonspecific treatment within 6 weeks. However, recent cohort studies estimate short-term recovery ranging from 39% to 79% (da C Menezes Costa et al., 2012). LBP continues to be a costly condition in terms of actual health care dollars spent, time lost from work, and reduced quality of life (Casazza, 2012; Machado, Maher, Herbert, Clare, & McAuley, 2010; Miller, 2012).
Pain is subjective, and there may be few if any objective findings. In fact, a precise pathognomonic diagnosis can be given in only 10% to 20% of patients with LBP (Casazza, 2012; Stanton et al., 2008). Because back pain may spontaneously resolve on its own, the back pain sufferers who seek health care attention are those for whom the pain is severe or disabling or lasts beyond a reasonable time, or for those seeking secondary gain. In most cases, LBP is labeled as lumbar strain because the physical examination reveals no gross abnormalities and recovery is usually quick.
This chapter discusses the etiologies of LBP and the evaluation and treatment of patients. Primary care providers must have a good understanding of the anatomic, biomechanical, and physiologic factors of back pain, as this will aid in the evaluation and treatment of patients with LBP.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
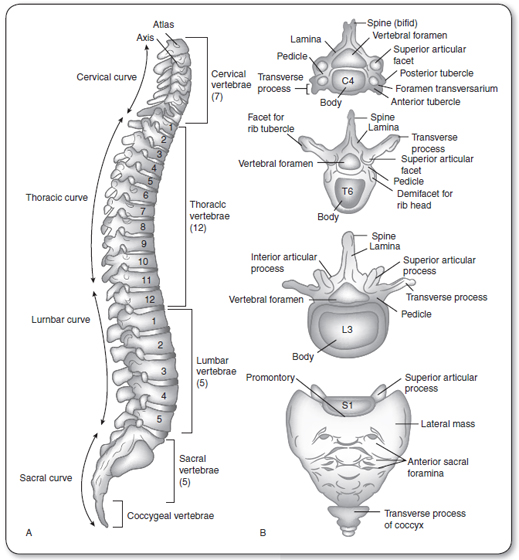
Anatomy of the Spine
The spine is divided into 4 sections: there are 7 cervical, 12 thoracic, and 5 lumbar vertebral sections, and the fused sacrum (Hainline, 1995; Figure 43.1). The bony vertebral bodies and intervertebral discs provide weight bearing and shock absorption. The posterior elements—vertebral arches, transverse and spinous processes, and facet joints—protect the spinal cord and nerve roots. The facets, ligaments, and paraspinal muscles provide stability and balance (Brady, 1996; Wipf & Deyo, 1995). Pain may arise from any of these structures. The combined anterior and posterior elements are referred to as a functional unit.
The lumbar vertebra is a static structure made up of the anterior vertebral body and posterior elements (spinous process, articular facets, and transverse process). There is a strong potential for pain at the vertebral body and facet articular cartilage secondary to increased pain sensitivity. The most common etiologies are degenerative joint disease and fracture of any part of the vertebra (body, compression fraction secondary to osteoporosis, pars interarticularis stress fractures).
The intervertebral disc plays a major role in LBP. It is composed of the outer annulus fibrosis, made up of multiple layers of collagen fibers, and the inner nucleus pulposus, made up of a colloidal gel of proteoglycans and collagen. It is 80% fluid (Al-Magdassy, 1996; Cyriax, 1991; Hainline, 1995). Its functions are absorbing shock, providing resistance to compression, and allowing flexibility of the vertebral column (Hainline, 1995). A compromised disc lends itself to abnormal motion and disc herniation, with potential radiculopathy and pain. The neurologic components of spinal anatomy are discussed later in this chapter.
Degenerative disc disease is usually secondary to an annular tear, with subsequent leakage of nuclear material and dehydration of the disc (Hainline, 1995). Large annular tears may lead to prolapse or herniation of the nuclear material and subsequent nerve root compression. With aging, the percentage of water decreases and the disc becomes less able to function normally, increasing the risk of disc herniation in the older population.
The superior and inferior posterior lumbar facets are synovial articulations situated between each vertebral body (Cyriax, 1991; Hainline, 1995; Margo, 1994; Wipf & Deyo, 1995). They play a potential role, along with the intervertebral discs, which play a major role, in lower back dysfunction and pain.
Ligaments play a major role in stability and restriction of motion in the lumbar spine. The key ligamentous structures include the anterior and posterior longitudinal ligaments, which help reinforce the annulus. As the ligament descends toward the sacrum, it narrows, increasing the risk of a herniated nucleus pulposus. The ligamentum flavum and the interspinous and supraspinous ligaments all provide further support to spinal movement (Al-Magdassy, 1996; Hainline, 1995).
FIGURE 43.1
(A) Lateral view of vertebral column. (B) General features of different kinds of vertebrae.
Source: Adapted from Snell (1992).
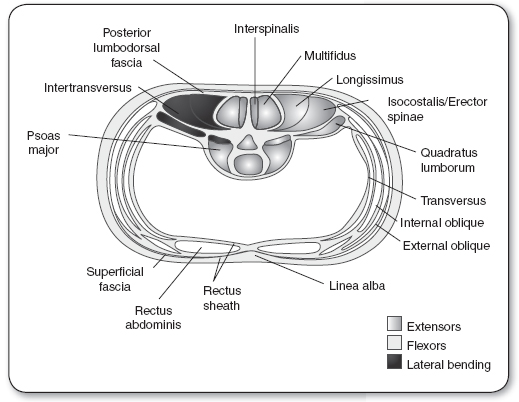
Muscles can be divided into anterior and posterior muscle groups. Most posterior is the erector spinae, made up of the lateral iliocostals, the intermediate longissimus, and the medial spinalis. The middle layer is the thick multifidus, and the deep posterior muscles include the rotators, interspinalis, and intertransversarii (Figure 43.2). The anterior muscle group includes the abdominal muscles that play a major role in lumbar stabilization. They include the psoas (which is a primary hip flexor), the outer external obliques, the intermediate internal obliques, and the inner transversus abdominis. The remaining anterior muscles include the midline rectus abdominis and the lateral quadratus lumborum that functions as a lateral trunk flexor (see Figure 43.2). All these muscles play a role in trunk motion and stabilization.
The anatomy of LBP is a combination of fact and theory. Studies have shown that pain can be reproduced by injecting hypertonic saline into the ligamentum flavum in facet joint capsules. Supra- and infraspinous ligaments are innervated by afferent branches of the posterior primary rami, and muscle spasms are thought to be a motor reflex to pain. The role of muscle injury as it relates to back pain has not been fully elucidated. Strains and sprains, however, remain the leading diagnoses.
Sciatic pain requires both mechanical and inflammatory stimuli. The sciatic nerve arises from L4–S3 nerve roots (common peroneal and fibial nerves), passes over the lower edge of the sciatic notch, and lies just beneath the piriformis muscle and just above the obturator internus muscle (see Figure 43.2). The nerve innervates the gluteus medius and minimus as well as the tensor fasciae latae before passing beneath the piriformis muscle. After passing through the main branch of the sciatic nerve, it innervates the hamstring and the muscles of the lower leg, and provides sensory innervation of the leg and foot (Borenstein, Wiesel, & Boden, 1995).
FIGURE 43.2
Cross-section of body musculature and fascia through the third lumbar vertebra. The primary motions of the lumbar spine are flexion, extension, and lateral bending (only a small portion of rotation occurs in the lumbar spine). Flexors are anterior to the spine and extensors are posterior. The muscles that cause lateral bending are contiguous to the vertebral bodies in a lateral position.
 EPIDEMIOLOGY
EPIDEMIOLOGY
One particular challenge of determining the epidemiologic prevalence of LBP is that diagnostic testing often fails to correlate with a patient’s reported symptoms. Therefore, surveys are used to determine the prevalence of LBP in the population. Data from the 2002 National Health Interview Survey suggest that LBP was the most common pain among various pain syndromes; an estimated 54 million American adults reported LBP in the last three months (Deyo, Mirza, & Martin, 2006). The prevalence of LBP is slightly higher among women, at 28.3%, than men, at 24.3%—with an increase in prevalence in persons aged 45 years and older. There is a greater incidence in American Indians and Alaskan Natives (35%) followed by whites (27.4%), Hispanics (24.3%), African Americans (23.9%), and Asians (19%; Deyo et al., 2006). Generally, the prevalence of back pain fell with increased levels of education and family income.
The prevalence of back pain alone and back pain with sciatica (defined as pain radiating along the course of the sciatic nerve to below the knee in one or both legs) is summarized in Table 43.1. The total costs of back pain exceed $100 billion in the United States per year (Katz, 2006).
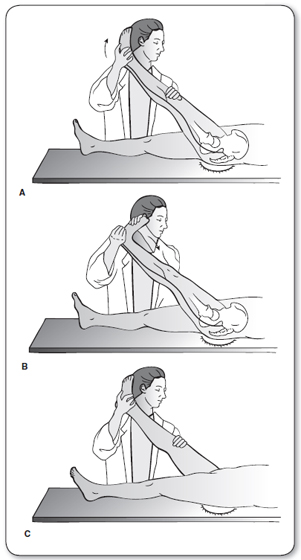
Back-Extension Exercises
The following exercises are to be performed in accordance with the comfort of the patient. The patient should perform only one exercise on any one particular day, and progress to the next exercise only when the pain from the previous one decreases. For patients with sciatic-type conditions, if symptoms intensify in either or both legs (increased pain, numbness, or tingling), patients should discontinue that exercise and contact with their physical therapist or primary care provider. If symptoms diminish in the legs, continue as instructed, even if accompanied by a temporary increase in lower back pain.
1. Lying on the stomach: Lie on your stomach with your arms close to your body and your head turned to one side or supported by a towel roll or small pillow under your forehead. Take a deep breath, then relax for 5 minutes. Perform one to two times per day.

2. Pillow under the chest: Lie on your stomach with your arms close to your body and your head turned to one side. While in this position, a pillow should be placed directly under the chest. Take a deep breath, then relax for 5 minutes. Perform one to two times per day.

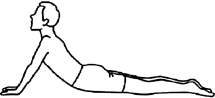
3. Prone on elbows: While lying on your stomach, place your elbows under your shoulders so that you are resting on your forearms. Take a deep breath, then relax for 30 seconds. Perform 10 repetitions, one to two times per day.

Classification of Low Back Pain Syndromes |
MECHANICAL OR ACTIVITY-RELATED CAUSES | REFERRED PAIN |
Segmental and discal degeneration Myofascial or soft tissue injury disorder Disc herniation, with possible radiculopathy Spinal instability, with possible spondylolisthesis or fracture Vertebral body fracture Spinal canal or lateral recess stenosis Arachnoiditis, including postoperative scarring | Gastrointestinal disorders Genitourinary disorders, including nephrolithiasis, prostatitis, and pyelonephritis Gynecologic disorders, including ectopic pregnancy and pelvic inflammatory disease Abdominal aortic aneurysm Hip pathology Psychosocial causes Compensable injury Somatoform pain disorder Psychiatric syndromes, including delusional pain Drug seeking Abusive relationships Seeking disability or out-of-work status |
SYSTEMIC DISORDERS | |
Primary or metastatic neoplasm, including myeloma Osseous, discal, or epidural infection Inflammatory spondyloarthropathy Metabolic bone disease, including osteoporosis Vascular disorders such as atherosclerosis or vasculitis | |
NEUROLOGIC SYNDROMES | |
Myelopathy from intrinsic or extrinsic processes Lumbosacral plexopathy, especially from diabetes Neuropathy, including inflammatory demyelinating type (i.e., Guillain-Barré) Mononeuropathy, including causalgia Myopathy, including myositis and metabolic causes |
Source: Wheeler (1995).
4. Press-ups: While lying on your stomach, place your hand under the shoulders, and slowly straighten your elbows. Keep the lower part of the body relaxed while raising the back upward as far as possible. Then relax and return to the starting position. Only raise the back as far as the pain will allow. Perform 10 repetitions, one to two times per day.
5. Back bending: While standing, place your hands on your low back. Slowly bend backward as far as possible, then relax, and return to the starting position. Perform 10 repetitions, one to two times per day.

6. Back-strengthening exercises:
(A) Lying on your stomach, with your forehead supported by a rolled towel or a pillow, raise one arm off the floor, keeping it straight. Do not lift your head. Hold for 10 seconds. Relax. Repeat 5 to 10 times, then repeat with the other arm.
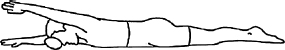
(B) Lying on your stomach, raise one leg off the floor, keeping it straight. Hold for 10 seconds. Relax. Repeat 5 to 10 times, then repeat with the other leg.
(C) Lying on your stomach, with your forehead supported by a rolled towel or a pillow, raise both arms off the floor, keeping them straight. Do not lift your head. Hold for 10 seconds. Relax. Repeat 5 to 10 times.
![]()
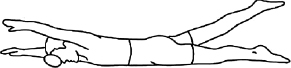
(D) Lying on your stomach, with your forehead supported by a rolled towel or a pillow, raise one arm and the opposite leg off the floor at the same time, keeping them straight. Do not lift your head. Hold for 10 seconds. Relax. Repeat 5 to 10 times, then repeat with the other arm and leg.
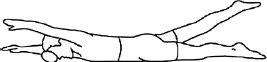
(E) Support yourself on both hands and knees. From this position, raise one arm and the opposite leg at the same time, as shown below, keeping them straight. Hold for 10 seconds. Relax. Repeat 5 to 10 times, then repeat with the other arm and leg.

7. Hip flexor stretching: Lie down on your back near the right edge of the table. Pull the left knee to your chest and let the right leg hang off the side of the table. You may use a weight on the right ankle. Be sure to hold your left knee as close to the chest as you can throughout the exercise. Hold for 10 seconds, then relax. Repeat 5 to 10 times, then move to the other edge of the table and stretch the other side.
LBP has numerous etiologies. Fewer than 3% of cases are secondary to a serious medical disease. Most cases of LBP are mechanical in origin. Mechanical conditions of the spine, including disc disease, spondylosis, spinal stenosis, and fractures, account for up to 98% of cases of LBP, with the remaining cases the result of systemic and visceral disease (Miller, 2008; Stanton et al., 2008). There are many opinions as to the actual neurogenic etiology of LBP, and only 10% to 20% of cases can actually be attributed to an anatomically defined lesion.
Epidemiologic studies also reveal distinct characteristics in the occupational and psychological profiles of people with long-term disability due to LBP. The psychosocial variables tend to be better determinants of long-term disability than diagnostic findings. Many patients present with depression, anxiety, maladaptive pain coping behaviors, poor general health status, and functional impairment (Chou & Shekelle, 2010). When working with patients who have LBP, providers must keep in mind the possibility of secondary gain—either financial gain (through a lawsuit for a motor vehicle accident or other liability) or the desire to remain off work and collect disability. These issues must be carefully and sensitively discussed if the provider has evidence that this is the nature of the patient’s LBP disability (Becker et al., 2010).
There are equal numbers of reports of LBP in heavy laborers compared to those in sedentary occupations. The loss of productivity, however, and time lost from work are greater in heavy laborers. The risk factors in both settings may be biomechanical (twisting and other repetitive motions that occur on the job). In sedentary occupations, there is an increased risk secondary to muscular deconditioning or the chronic mechanical stress from sitting positions (Beattie, 1996).
Osteoporosis increases the risk of spinal compression fractures. Genetics may play a role in osteoporosis as well as congenital isthmic spondylolisthesis, spinal osteochondrosis (Scheurmann’s disease), and spinal stenosis associated with achondroplasia. In addition, certain athletic activities, such as gymnastics and football, may increase the risk of spondylolysis and isthmic spondylolisthesis because they involve repetitive hyperextension.
 DIAGNOSTIC CRITERIA
DIAGNOSTIC CRITERIA
Differential Diagnosis
Although there are no true diagnostic criteria for LBP, Table 43.1 shows the multitude of LBP syndromes. This section focuses on the more common etiologies, or specific diagnoses of secondary back pain. The provider must be able to differentiate between benign causes, such as lumbar strain and disc disease, and the more ominous and life-threatening disorders that require quick referral, such as cauda equina syndrome, malignancy, and vertebral fracture with neurologic compromise. A thorough history and a detailed physical examination, including a neurologic examination, are warranted.
LBP can be divided into three clinical courses: acute, subacute, and chronic. It is useful to differentiate these three categories when approaching treatment protocols. The definitions are as follows:
 Acute: 0 to 6 weeks
Acute: 0 to 6 weeks
 Subacute: 6 to 12 weeks
Subacute: 6 to 12 weeks
 Chronic: More than 12 weeks
Chronic: More than 12 weeks
It is also important to categorize back pain along with its etiology for correct treatment and accurate referral.
Mechanical or Activity-Related Causes
DEGENERATIVE DISC DISEASE
There appears to be a correlation between annular tears of the disc and degenerative disc disease. As previously stated, there is also a correlation with herniated nucleus pulposus. A slow leak over time of the nuclear material will lead to desiccation of the disc. How does this lead to back pain? One explanation is an inflammatory pathway involving chemical factors. This pathway may explain why pain is relieved when a corticosteroid or nonsteroidal anti-inflammatory agent is administered (Miller, 2008; Rudy, Weiner, Lieber, Slaboda, & Boston, 2007). The other theory is an immunologic phenomenon, described by in vitro studies. It is theorized that the nuclear material, previously sheltered from the immune system, generates an autoimmune response once it is exposed.
Degenerative disc disease may present with isolated LBP or with radicular symptoms. The diagnosis can be made with plain radiographs, noting diminished disc space between the vertebral bodies, or by MRI, which notes changes in T2-weighted images (Chou, Fu, Carrino, & Deyo, 2009; Davis, Wippold, & Burnberg, 2011; Roberts, Willick, Rho, & Rittenberg, 2009).
LUMBAR SOFT-TISSUE INJURY/STRAIN/SPRAIN
Most cases of LBP fall into this category, known as nonspecific back pain. This pain usually resolves spontaneously in 2 to 6 weeks. If the pain persists longer than this, a secondary cause must be considered (i.e., disc vs. facet). In this type of pain, the most common etiologic factors are poor conditioning, excess weight, and sudden overuse or overload activities.
HERNIATED LUMBAR INTERVERTEBRAL DISC
Herniated disc is diagnosed in a small percentage of patients with LBP. Lumbar disc herniation is most common in persons aged 30 to 40 years; it is less common in adolescents and young adults and rare in the older population (Becker et al., 2010; Miller, 2008; Stanton et al., 2008). Acute herniation of the nucleus pulposus may result from sudden overload of the intervertebral disc or from repetitive microtraumatic loading (Miller, 2008; Netter, 2003). For most patients with a herniated disc, back pain precedes the onset of sciatica. The back pain may or may not linger as the pain and paresthesias begin to radiate down the leg (Miller, 2008).
The onset of sciatic pain may be gradual or sudden. Pain and radicular symptoms may be worsened by sitting for a long period, rising from a sitting or supine position, or coughing or sneezing.
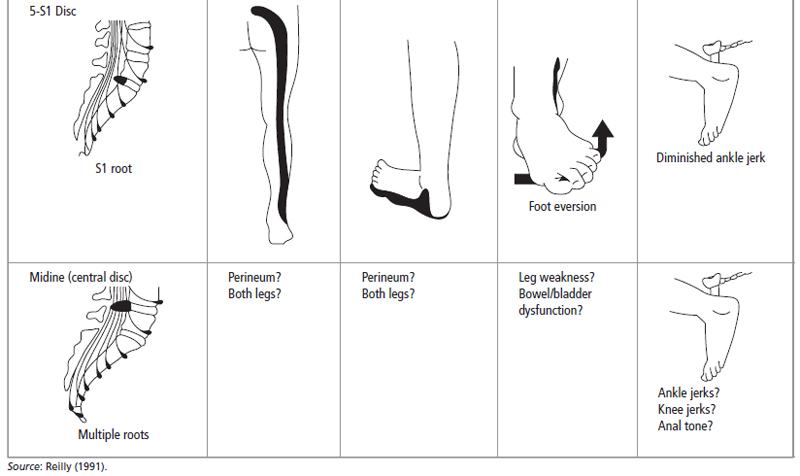
Herniated discs occur at the L4–5 or L5–S1 level in 95% of cases (Miller, 2008; Stanton et al., 2008). The neurologic examination should focus on the L5 and S1 nerve roots. A herniated disc at the L5 nerve root may cause pain and numbness radiating from the back to the anterior thigh, anterolateral leg, medial foot, and great toe. There are no reflex changes, and the motor examination reveals weakness in the great toe extensor as well as the dorsiflexors of the foot (Table 43.2).
Patients with an L5–S1 disc herniation (sacroiliac [SI] root) have pain and numbness of the posterior thigh and leg, posterior–lateral foot, and lateral toes; a diminished ankle reflex; and weakness of the plantar flexors of the foot that can be seen with difficulty on toe walking (see Table 43.2). It is rare to see clinical herniations above the level of L4.
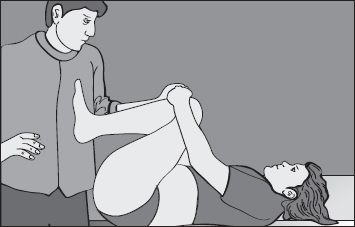
A positive straight-leg raise (SLR) test helps confirm nerve root irritation. This test has a sensitivity of 95% with proven disc herniation, and its absence can actually rule out disc herniation. A crossover test or crossed SLR is less sensitive but more specific for disc herniation (Figure 43.3). Electromyography may aid in the diagnosis of a particular radiculopathy, but it is better used to discriminate radicular pain from peripheral neuropathy.
Plain x-rays are not helpful in diagnosing a herniated disc, but they should be used to rule out tumor, infection, fracture, and spondylolisthesis as clinically warranted. A herniated disc is usually confirmed when an imaging study such as CT or MRI shows an abnormality corresponding to the clinical examination. However, these sophisticated and expensive studies should not be ordered too early in the course of a workup for LBP, especially if the patient is not considered a surgical candidate. These tests should be ordered in patients who have a long protracted course, or early in the case of cauda equina syndrome, a progressive neurologic deficit, or the suspicion of tumor or infection (Beattie, 1996).
SPINAL STENOSIS
Spinal stenosis (narrowing of the spinal canal) may be secondary to hypertrophy of the facet joints (osteoarthritis), hypertrophy of the ligamentum flavum, or spondylosis of the intervertebral disc that is often superimposed on a congenitally narrow canal (Stanton et al., 2008).
Spinal stenosis is most likely in the older population. Patients present with an insidious onset of pain and numbness that worsens with walking. The pain of spinal stenosis is referred to as pseudoclaudication because of its similarity to vascular claudication (Casazza, 2012). Patients may have adermatomal distribution of pain and sensory deficit as well as an abnormal SLR test. To differentiate this from a herniated disc, the factors that exacerbate and relieve the pain should be noted. Spinal stenosis is relieved by sitting and aggravated by standing; a herniated disc is exacerbated by sitting and relieved by standing (Casazza, 2012).
In spinal stenosis, deep tendon reflexes may be decreased, with weakness in one or both lower extremities. The diagnosis is confirmed by MRI imaging revealing a narrow spinal canal. Plain films would point out only the degenerative changes that lead to spinal stenosis.
SPONDYLOLYSIS/SPONDYLOLISTHESIS
These disorders are most common in young adolescents and young adults who are involved in sports such as gymnastics, tennis, weight lifting, and football (linemen). These sports put the lumbar spine into hyperextension. Spondylolisthesis is the slipping of one vertebral body forward on the one below. The extent of slippage is graded from grade I to grade IV (total forward displacement). Often spondylolisthesis is secondary to bilateral spondylolysis. Spondylolisthesis is best seen on plain lateral radiographs.
FIGURE 43.3
(A) Straight-leg raising. (B) In this position, dorsiflexion of the foot reproduces sciatic pain. (C) A positive crossed SLR test: back pain on the involved side induced by straight-leg raising the noninvolved leg.
Source: Adapted from Hoppenfeld (1976).
Spondylolysis is a stress fracture or fatigue fracture of the pars intrarticularis. This stress fracture is usually caused by repetitive overload of the pars with repeated hyperextension. The symptoms may include LBP with or without radiation, a tight hamstring, and relief of symptoms with rest. The severity and extent of the defect may change the clinical findings. For example, a unilateral defect may be found in an asymptomatic person. This lesion would be considered inactive, whereas a patient with an active lesion or significant spondylolisthesis may have severe hamstring tightness, gait disturbance, and neurologic symptoms. X-rays may reveal a defect through the pars interarticularis. This may be seen on standard anteroposterior and lateral views but is usually seen better on oblique radiographs that truly outline La Chapele’s “Scotty dog” (Hoppenfeld, DeBoer, & Buckley, 2009).
VERTEBRAL COMPRESSION FRACTURE
Vertebral compression fractures are most consistent with osteoporosis in women over age 65 and men over age 75 with decreased bone mass. Osteoporosis in itself has no signs and symptoms and may progress silently for years until an ominous compression fracture leads to pain and disability. The patient may have pain and a tender point at the level of fracture and may splint the back to avoid mobility at the fracture site. Plain films may reveal the fracture or a decrease in vertebral height. Bone mineral densitometry can be used to diagnose osteoporosis by calculating the patient’s bone mineral density and comparing it to the normal bone density for age (see Chapter 45).
FACET SYNDROME (ARTHROPATHY)
Arthropathy of the facet joints may be difficult to diagnose. Patients may have LBP with or without radiation to the buttocks. Hyperextension may precipitate facet impingement and exacerbate symptoms (Casazza, 2012). The physical examination may be unremarkable except for pain on extension of the trunk. SLR and the neurologic examination are usually unremarkable. A plain radiograph may or may not demonstrate changes at the facet joints. MRI demonstrates degenerative changes at the intervertebral discs and at the facet joints.
PIRIFORMIS SYNDROME
Piriformis syndrome has become a common diagnosis, especially when it relates to buttock pain without LBP symptoms. The piriformis muscle is an external rotator of the hip. It traverses over the sciatic notch and inserts on the greater trochanter of the femur. Piriformis syndrome is common in athletes, persons who excessively abduct the hip or overuse the muscles of the buttock, and persons who have excessive compression over the sciatic notch (e.g., sitting on an overstuffed wallet). The physical examination may reveal tenderness over the sciatic notch, pain with forced internal rotation of the hip, and pain and weakness with simultaneous abduction and external rotation of the hip. The neurologic examination is normal, as are plain radiographs (Scheele, Luijsterburg, Bierma-Zeinstra, & Koes, 2012).
SI SPRAIN
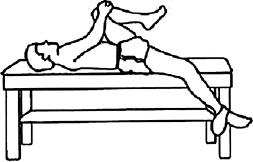
The SI joints are often overlooked as an etiology for LBP. There is controversy as to whether the SI joints can be sprained, because they are among the strongest joints in the body. True subtle motion at this joint may predispose a person to injury of this joint. Clinically, the patient may present with pain at the SI joint. This SI pain should be differentiated from that of piriformis syndrome or other pathology that may be referred to the groin and posterior thigh. Pain may increase when the patient lies on the affected side. There are several provocative tests, including Gaenslen’s extension test (Figure 43.4), the Patrick/FABER test (Figure 43.5), and the SI compression test. Unlike patients with sciatica and piriformis syndrome, there is no tenderness at the sciatic notch. Plain radiographs may or may not show changes at the SI joint; nevertheless, they are valuable in ruling out other potential diagnoses (e.g., fracture, malignancy, infection, ankylosing spondylitis).
Degenerative Disorders: Osteoarthritis
Osteoarthritis is the most common degenerative disorder. Degeneration of the articular cartilage involving both the facet joints (as previously described) and vertebral columns occurs. It is easily diagnosed by correlation of symptoms and plain x-ray findings. Other possibilities that cause back pain must still be considered before making a diagnosis.
Systemic Disorders
INFLAMMATORY DISEASES
The seronegative arthropathies, rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, Reiter’s syndrome, and arthritis associated with inflammatory bowel disease are a few of the inflammatory arthropathies that may lead to LBP. The diagnosis is made usually after the failure of other diagnoses. The workup includes laboratory tests specific for each disorder (see the “Diagnostic Studies” section later in this chapter).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree