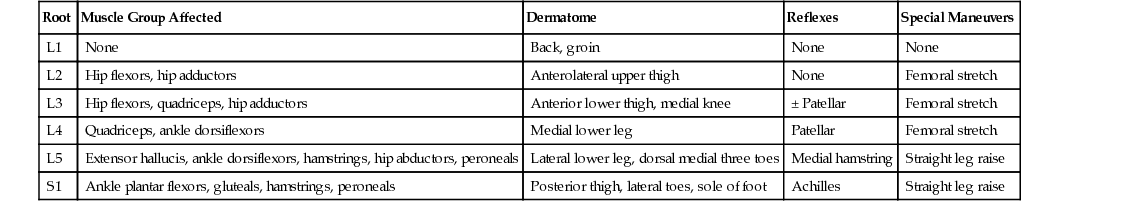
Lindsay Ramey, Zacharia Isaac, Sharon Alzner Low back pain is the most common musculoskeletal problem worldwide and is estimated to affect up to 85% of the population at some time in a person’s life. It has an estimated yearly prevalence of 38% and occurs most frequently in females and those aged 40 to 80 years.1 In the United States, back pain is the second most common reason for visits to a physician. It is also a leading cause of hospital admissions and subsequent surgery. Low back pain is commonly classified by symptom duration as acute, subacute, or chronic (Table 181-1). Approximately 30% to 60% of people with acute low back pain recover within 1 week, and 80% to 90% recover within 6 weeks.2 However, recurrence rates are high, with up to 50% reporting recurrence of pain within 6 months.2 Although low back pain is typically transient, if it persists and becomes subacute, there is an increased risk for developing chronic low back pain. The average prevalence of chronic low back pain is approximately 15% in adults and 27% in the elderly and has been shown to be increasing as the population ages.3 TABLE 181-1 Classification of Low Back Pain Risk factors for development of low back pain are broad. Age older than 65 years is a prominent risk factor for the development of musculoskeletal impairment, with a majority of these cases involving the back. Genetic disposition, obesity, and smoking have also been linked to accelerated degenerative disk disease, increasing the risk of low back pain.3 Studies of identical twins support the strong influence of genetic factors on the development of degenerative disk disease. Jobs involving heavy lifting, pulling, pushing, prolonged walking or standing, and vehicular driving have been found to be predictors of future low back pain.4 Preexisting psychological conditions such as anxiety, depression, or somatization disorder, in addition to maladaptive coping strategies, lower socioeconomic status, and poor general health, are risk factors for chronic low back pain.5 In fact, these factors are stronger predictors of long-term disability than any anatomic findings on imaging. The total cost of low back pain in the Unites States exceeds $100 billion annually, most of which is spent on those who develop chronic, disabling low back pain. Fewer than 5% of back pain patients account for 75% of the total costs.6 In addition to the financial burden, chronic low back pain can have a significant impact on quality of life, with 60% of patients reporting inability to perform daily activities and 25% being unable to work.7 Given the significant socioeconomic burden of chronic low back pain, it becomes pertinent to understand the natural course of low back pain and risk factors for developing chronic pain to help direct diagnostic and treatment decisions. The lumbar spine consists of five lumbar vertebrae that increase in size caudally. Each vertebral body is separated by shock-absorbing intervertebral disks, consisting of a gelatinous nucleus pulposus surrounded by the fibrous rings of the anulus fibrosus. The nucleus pulposus consists of water, proteoglycans, and collagen; it is 90% water at birth and desiccates with time as part of the degenerative cascade. The neural arch is formed laterally by the pedicles, which connect the posterior elements to the vertebral bodies, and encloses the central canal where the spinal cord and cauda equina reside. The posterior elements consist of the laminae, spinous processes, and articular processes that form the facet joints. The space between adjacent pedicles forms the foramen through which spinal nerve roots may enter and exit the spinal canal. In addition, there are ligamentous structures supporting the lumbar spine. Pain can arise from the innervated intervertebral disks, facet joints, ligaments, or spinal nerve roots. The lumbar spine is supported by various muscles that help provide dynamic stabilization to the spine and pelvis. Posteriorly, the paraspinal muscles consist of the erector spinae, multifidi, psoas, and quadratus lumborum. Anteriorly, the abdominal musculature, including the transversus abdominis, plays a critical role in supporting the lumbar spine. There is evidence to support that the structure and function of these spinal stabilizers are altered in patients with low back pain.8 In addition, these muscles can be a potential source of myofascial low back pain. Low back pain has been classified based on pathophysiology as either mechanical or the result of a systemic medical illness. Medical causes of low back pain include inflammatory, infectious, neoplastic, and visceral sources. Systemic medical causes of low back pain are rare but frequently associated with the need for time-sensitive treatment. If no primary systemic source is identified, the pain is classified as mechanical pain. Mechanical causes of low back pain include direct injury, deformity, imbalance, or overuse of identifiable structures in the lumbar spine, but are most commonly degenerative in nature. Structural sources of mechanical low back pain include the intervertebral disks, facet joints, vertebral bodies, nerves and nerve roots, ligamentous structures, paraspinal muscles, and sacroiliac joints. For example, wear and tear of the spine with aging can lead to intervertebral disk degeneration and herniation, facet and uncovertebral arthritis, osteophyte formation, ligamentous and capsular hypertrophy, and spondylolisthesis at various rates, which can be sources of pain independently or can lead to nerve root compression with resulting pain. When nerve root injury is contributing to low back pain, it can produce symptoms radiating down the leg including pain, weakness, paresthesias, and altered reflexes in a specific dermatomal or myotomal distribution, termed radiculopathy. Radiculopathy is reported in approximately 7% of patients with low back pain.2 Radicular pain is commonly attributed to direct compression of the spinal nerve roots with resulting structural, biochemical, and vascular changes in and around the spinal nerve. In addition, mechanical stimulation of the lumbar spinal nerve roots has been shown to increase the production of the pain-generating neuropeptide substance P.9 Studies have shown that disk herniations and tears in the anulus fibrosus can produce increased inflammatory mediators, such as phospholipase A2, cyclooxygenase 2, nitric oxide, cytokines, interleukins, and immunoglobulins, which can lead to local swelling and swelling of the spinal nerve roots.9 Pain can be further classified as nociceptive or neuropathic. Nociceptive pain is associated with tissue damage. Neuropathic pain is associated with minimal or no tissue damage and is more related to a dysfunction of the pain regulatory function of the central and peripheral nervous system. Why damage to specific anatomic locations produces severe pain in some but no pain in others is quite complicated and not fully understood but relates to numerous factors including local inflammation, biomechanical factors, muscular strength and flexibility deficiencies and imbalances, and centrally mediated pain regulatory systems that are influenced by mood, sleep, cardiovascular health, and psychosocial context. Symptomatically, mechanical lumbar spine disorders can be classified as axial or radicular pain. Axial low back pain is typically isolated to the back at the lumbar spine or lumbosacral junction with varying degrees of gluteal symptoms. New, acute low back pain typically is axial pain only but can be severe, disrupting sleep, work, and activities of daily living. It is often exacerbated by prolonged sitting, standing, leaning, or bending and is mitigated by frequent positional shifts. Extension typically worsens pain mediated from the posterior elements, whereas flexion typically worsens pain mediated from anterior elements. The seated position, forward flexion, and Valsalva maneuver can increase intradiskal pressure, worsening disk-mediated low back pain. Facet loading may worsen facet-mediated pain. Patients with the syndrome of lumbar radiculopathy will often have leg and thigh pain greater than low back pain. Pain can be severe even in the absence of neurologic deficit. Neurologic symptoms of numbness, tingling, weakness, reflex changes, and root tension signs may be seen on examination. Symptoms are exacerbated by prolonged sitting, coughing, sneezing, Valsalva maneuver, and bending. Pain is often mitigated by frequent positional shifts and walking. Pain radiating past the knee and into the calf or foot is typically radicular and represents nerve root or peripheral nerve injury. However, pain in the buttocks and thigh is not always radicular and can come from anatomic locations outside of the spine. It can be referred from adjacent bone, ligament, or muscle structures, making it important to evaluate the hip, pelvis, and surrounding musculature to rule out any other contributing pathology before attributing this type of pain to the lumbar spine. Other specific causes of low back pain have a more identifiable presentation. Patients with lumbar spinal stenosis, narrowing of the spinal canal with or without compression of the spinal cord, typically have back pain and neurogenic claudication. Patients often describe their legs as feeling heavy or wooden. Neurogenic claudication is defined as thigh and calf pain worsened by standing or walking and alleviated with sitting. This can be differentiated from vascular claudication in that patients with vascular claudication may have altered peripheral pulses, more difficulty with uphill walking, no symptoms with standing alone, and a steady degree of symptomatic severity from day to day. In contrast, patients with neurogenic claudication have significant day-to-day variability, and symptoms with standing still. Walking with a shopping cart is often better tolerated in neurogenic claudication because the patient is flexed forward, thus expanding the spinal canal diameter. Neurologic changes are usually more subtle, with vibratory loss in the distal lower extremities, increased pain with lumbar extension, absent root tension signs, mild balance deficits, and largely normal strength on examination. In conus medullaris and cauda equina syndromes, saddle anesthesia, urinary retention or incontinence, lower extremity weakness, and recent-onset erectile dysfunction can be seen. Cauda equina syndrome involves compression of multiple lumbosacral nerve roots below the termination of the spinal cord, called the cauda equina, leading to the aforementioned symptoms and hyporeflexia in the lower extremities. This syndrome can be caused by several conditions, including trauma, tumors, spondylolisthesis, and direct compression secondary to severe spinal stenosis or a large disk herniation. It is a very rare but serious neurologic condition, and urgent surgical referral is recommended. Other conditions to consider are the seronegative spondyloarthropathies, spinal tumors, vertebral fractures, and spinal infections. Seronegative spondyloarthropathies (see Chapter 215) typically are seen in younger patients with symptoms of pain, stiffness, and reduced range of movement in the morning that improves with activity. Family history and additional joint symptoms should be explored. Tumors of the spine may occur in patients with prior history of malignant disease; localized pain is frequently reported to increase in the supine position and at night. Although classically taught “red flags” for tumor include age older than 50, weight loss, and failure to improve after 1 month, there is low diagnostic accuracy for any of these factors independently.10 In patients with recent spinal surgery, recent skin or urine infections, history of intravenous drug abuse, or immunocompromised states, infection should be considered. Although fever is commonly sited as a red flag for spinal infection, this finding has low sensitivity and lack of fever does not rule out infection. Vertebral fracture should be considered in the differential if there is a history of significant trauma, older age, or corticosteroid use.11 Among all primary care patients with low back pain, fewer than 5% have a serious systemic pathology. However, given the important clinical implications, it is paramount to screen for these diagnoses. Physical examination starts with careful observation of the patient; the examiner looks for discomfort or frequent change of positions and evaluates the patient’s affect. Spinal examination then begins with observation of the lumbar spine, looking for any asymmetries or abnormal curvature. Palpation and percussion of the spinous processes should be performed to evaluate for osseous pain and spinal infection. The range of motion of the lumbar spine should be assessed in flexion, extension, lateral flexion, and rotation to evaluate for changes in symptoms throughout the movements. The normal range of motion of the lumbar spine is 40 to 60 degrees of forward flexion, 20 to 35 degrees of extension, 15 to 20 degrees of lateral flexion, and 3 to 18 degrees of rotation. Pain with movement in specific directions should be noted. As previously explained, anterior sources of pain tend to worsen with forward flexion and posterior sources of pain tend to worsen with extension. Although limitations in range of motion may not permit identification of the specific source of pain, assessment of range of motion can provide an index for future comparison to assess therapeutic response. Facet loading can be performed by placing the patient in hyperextension with a slight rotation toward each side to help identify facet-mediated pain. Anatomic alignment during neutral standing should be noted. Romberg testing should be performed to test balance. Gait should be examined to look for antalgia, footdrop, spastic or mechanical movement, Trendelenburg gait, and widened or narrowed steps. The skin and lower extremity pulses should be examined to look for vascular insufficiency as a potential cause of thigh or calf symptoms. In addition, if patients are describing symptoms of cauda equina syndrome, rectal examination should be considered to evaluate for loss of rectal tone. Neurologic examination should be undertaken, assessing the symmetry of the patient’s strength in hip flexion, knee extension, knee flexion, ankle dorsiflexion, ankle plantar flexion, foot eversion, great toe extension, and hip abduction bilaterally. In addition, the patient should be observed walking on heels and toes to assess for functional strength in L5 and S1, respectively. It may be difficult for the examiner to overcome the quadriceps, even if there is some weakness. The examiner should have the patient perform single-legged sit-to-stand testing bilaterally, with examiner support for balance, to pick up mild quadriceps weakness. Because plantar flexion weakness may be difficult to detect, it is recommended to test the S1 myotome with repeated standing calf raises on each leg to elicit any mild weakness or muscular atrophy. Sensation to both light touch and pinprick should be checked for sensory deficits throughout the dermatomes listed in Table 181-2. Bilateral reflexes should also be elicited at the patella (L4 nerve root), and Achilles (S1 nerve root). Babinski examination and evaluation for clonus, muscle spasticity, or increased tone can help assess for upper motor neuron involvement. Because disk herniations are most common at L4-L5 and L5-S1, clinical changes in these myotomes and dermatomes should be thoroughly assessed. If the patient’s symptoms are radicular in nature, root tension signs can help identify irritation of the lumbar nerve roots. The straight leg raise test is performed to assess for damage to L5-S1. With the patient in the supine position, the examiner raises the straight leg to approximately 70 to 90 degrees of hip flexion. If the patient’s typical pain or paresthesias are reproduced at any point when the leg is in 20 to 70 degrees of hip flexion, the test result is positive and indicates that a nerve root impingement from a herniated disk is likely contributing, referred to as sciatica. Studies have reported a high sensitivity but low specificity of the straight leg raise.12 If the unaffected leg is tested and symptoms are reproduced in the symptomatic leg, this is called a positive crossed straight leg raise and has increased specificity for disk herniation.12 A modification to the straight leg raise can be performed in the seated position and is referred to as the seated slump test. The patient is asked to slump forward, allowing the thoracic and lumbar spine to collapse into flexion, and then to fully flex the cervical spine toward the chest. The patient is then asked to extend each leg fully and dorsiflex the ankle to see if there is reproduction of symptoms down the leg.13 Another root tension sign, the femoral nerve stretch test, is used to look for an upper lumbar radiculopathy in L2-L4 distribution. With the patient in the prone position, the leg is flexed at the knee and the hip is brought into extension. The test result is considered positive if a reproduction of typical pain in the anterior thigh occurs. The most recent guidelines from the American Academy of Family Physicians, American College of Physicians, and American Pain Society do not recommend routine imaging for patients with acute or nonspecific low back pain, because this does not improve clinical outcomes and exposes patients to unnecessary radiation.14,15 A systematic review and meta-analysis of six trials comparing immediate imaging with usual care for patients with acute and subacute low back pain, without suspicion for infection or malignancy, found no significant difference in short- or long-term outcomes for pain or function.16 However, if a patient has certain red-flag symptoms, described earlier, or if clinical improvement has not occurred in 4 to 6 weeks, plain radiographs of the lumbar spine are the preferred initial diagnostic tool.14 Typically, anterior-posterior and lateral views are sufficient. Oblique views can also be obtained to visualize the pars interarticularis but are not routinely recommended. Because plain radiographs have low sensitivity and specificity,15 their diagnostic yield is limited; persistent pain or suspicious symptoms may prompt additional imaging. The most widely used imaging modality to further evaluate low back pain and radiculopathy is magnetic resonance imaging (MRI). Its principal use is to evaluate the bone structures and soft tissues, and it can be helpful to look for degenerative disk disease, disk herniations, spinal stenosis, and cord or root compression. With the addition of gadolinium, it can be used to look for tumor or infection and can distinguish epidural scar tissue in postoperative patients. MRI, however, is an expensive diagnostic tool. Guidelines recommend MRI acutely only if patients have severe or progressive neurologic deficits or symptoms of a serious underlying condition.14 MRI can also be considered for a patient with persistent low back pain with symptoms of nerve root impingement refractory to conservative treatment, for which interventional procedures are being considered. Although it is superior for identification of potential pain generators in the spine, MRI abnormalities do not always correlate with clinical complaints, and multiple studies have found common pain-producing degenerative findings in asymptomatic patients.17 In cases where radiographic findings are consistent with clinical presentation, the magnitude of radiographic findings does not correlate with symptom severity or clinical outcome, and symptom improvement does not correlate with resolution of radiographic defects.18 For this reason, physicians should focus on clinical presentation rather than radiographic abnormalities. Contraindications to MRI include pacemaker, retained metal fragments such as from a gunshot wound, and severe claustrophobia. Most currently used orthopedic metal does not preclude MRI imaging. Other diagnostic tools used for low back pain are radionuclide bone scintigraphy and computed tomography (CT). Bone scintigraphy is helpful if the history and physical examination raise suspicion for osteomyelitis, bone neoplasm, or occult fracture. The addition of bone scan with single-photon emission computed tomography (SPECT) can identify recent pars fracture and facet osteoarthritis. CT can be helpful in assessing the bone architecture of the spine and can also provide helpful imaging in a postsurgical patient with excessive hardware or in those with contraindications to MRI. CT imaging can be used to assess for degenerative disorders such as spondylosis, spondylolysis, spondylolisthesis, and spinal stenosis as well as to show cortical irregularities in osteoarthritis. It can be used in combination with myelography to visualize the borders and contents of the dural sac and to evaluate for cord compression. Other diagnostic workup may be considered on a case-by-case basis. Laboratory testing, such as erythrocyte sedimentation rate and C-reactive protein, can be helpful in a patient with constitutional symptoms to quantify systemic inflammation, as can be seen with infection, inflammatory spondyloarthropathies, or neoplasm. Neoplasm may also be associated with an abnormal complete blood count, alkaline phosphatase, or calcium level. Electrodiagnostic studies can be helpful in assessing neurologic changes associated with denervation caused by subacute and chronic radiculopathy. Electromyography may not be able to detect acute changes until approximately 3 to 4 weeks after the initial insult. The needle electromyographic portion of the examination can identify radiculopathy with high specificity; however, it is relatively insensitive to the clinical syndrome of radicular pain without motor or reflex changes. The goal of diagnostic testing is to help guide management strategies and improve patient outcomes. Unless there is clear indication that testing can aid in this process, routine testing is not recommended, especially in a population with low clinical suspicion, because this can lead to false positives, unnecessary medical expenses, and avoidable patient anxiety. Many patients have come to expect imaging, so it is important for the clinician to educate the patient and provide reassurance. Imaging for reassurance has not been shown to improve outcomes. In one randomized trial, low-risk patients who received an educational intervention rather than radiography were equally satisfied with their care and had no difference in clinical outcomes.19
Low Back Pain
Definition and Epidemiology
By Symptom Duration
By Pathophysiology
By Symptom
Acute: Less than 6 weeks
Mechanical
Axial low back pain
Subacute: 6 weeks to 3 months
Systemic medical (nonmechanical)
Radicular pain
Chronic: More than 3 months, with symptoms more than half the days in the last 6 months
Pathophysiology
Clinical Presentation
Physical Examination
Diagnostics
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree